Assessment of Fracture Risk
Paul D. Miller
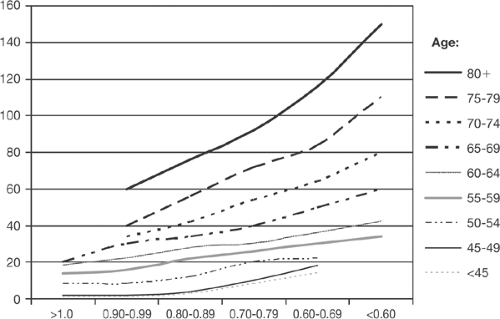
Use of Bone Mineral Density for Fracture Risk Assessment
As pointed out in Chapter 1, the T-score has (and will remain) an important “number” for the diagnosis of osteoporosis in nonfractured patients. The impact on the T-score value for fracture risk prediction depends heavily on how the T-score is interpreted [1,2]. A low T-score [or bone mineral density (BMD)] has very different risk prediction implications at age 50 years than it does at age 80 years [3]. Hence, in isolation, a T-score is not a T-score is not a T-score (Fig. 3.1). A low BMD predicts an increased risk for fracture, but increased age is even a greater predictor of risk at equivalent levels of BMD. Why increased age conveys a greater fracture risk at the same BMD value is unclear, except that perhaps older people may fall more often than younger people, and, that there are changes in bone quality (cortical shell and porosity, crystal size, collagen maturation, microarchitecture) that render the older bone more fragile than the younger bone at the same T-score [3,4,5]. The combination of a T-score and additional risk factors for fracture provides a more refined quantitative assessment of fracture risk than can be obtained by a low BMD alone. It is important to stress, however, that the diagnosis of osteoporosis can also be made based on the presence of a fragility (low-trauma) fracture, regardless of the level of the T-score, which is the manner in which osteoporosis was diagnosed before the World Health Organization (WHO) criteria were developed.
History of Fragility Fractures
A prior fragility fracture is predictive of a high risk for future fracture. In the field of osteoporosis, a fragility fracture is defined as a fracture that occurs spontaneously or from a fall equal to or less than one’s standing height.
Table 3.1. Metaanalysis of the effect of prior fracture on subsequent relative risk for future fracture risk | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Fractures that are predictive of a higher risk for future fracture in population studies as well as placebo arms of pharmacological clinical trials are vertebral compression fractures (VCF), hip fractures, wrist and forearm fractures, humeral and shoulder fractures, and rib fractures (Table 3.1) [6,7,8,9,10,11,12,13,14,15]. Fragility fractures at these sites are predictive of future fracture
risk independent of the BMD. Forearm fractures, previously shown to be predictive of a high risk for other nonforearm fractures, have recently been shown to also predict a high risk for other fractures in the large, longitudinal National Osteoporosis Risk Assessment (NORA) database. In NORA, all (global) fragility fractures were captured after the age of 45 years, before as well as after the first 1 to 5 years after entry into NORA. There were 8,554 prior wrist fractures for end of year 1 captured in NORA [16]. In these postmenopausal women, a prior wrist fracture was associated with a large increase in the incidence of another fracture, even at distant skeletal sites (e.g., hip), within a brief period of time. Just why a prior fragility fracture conveys a high risk for fracture at other skeletal sites is not clear, except to suggest that a fragility fracture is symbolic of systemic skeletal fragility.
risk independent of the BMD. Forearm fractures, previously shown to be predictive of a high risk for other nonforearm fractures, have recently been shown to also predict a high risk for other fractures in the large, longitudinal National Osteoporosis Risk Assessment (NORA) database. In NORA, all (global) fragility fractures were captured after the age of 45 years, before as well as after the first 1 to 5 years after entry into NORA. There were 8,554 prior wrist fractures for end of year 1 captured in NORA [16]. In these postmenopausal women, a prior wrist fracture was associated with a large increase in the incidence of another fracture, even at distant skeletal sites (e.g., hip), within a brief period of time. Just why a prior fragility fracture conveys a high risk for fracture at other skeletal sites is not clear, except to suggest that a fragility fracture is symbolic of systemic skeletal fragility.
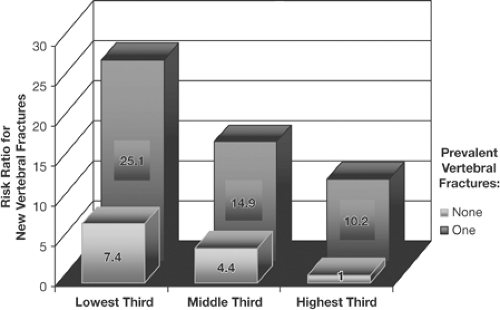
It was recognized in 1991 that the presence of a morphometric VCF increased the risk of future fractures of the vertebrae independent of the baseline BMD, and the presence of an existing VCF in combination with low BMD increased the future fracture risk far more that the risk predicted by either a VCF or low BMD alone [15] (Fig. 3.2).
Low BMD as measured by central or peripheral dual-energy x-ray absorptiometry (DXA), peripheral ultrasound, or spine quantitative computed tomography (QCT) is predictive of an increased risk for fractures at any other skeletal site [17,18,19,20,21,22,23,24,25,26,27].
In addition, from individual longitudinal studies, including population studies, and from metaanalysis, all these BMD measuring devices predict an increased risk of fracture in postmenopausal women or elderly men with an overlapping relative risk (RR) predictability: Risk increases approximately 2 times for each 1.0 SD reduction in BMD calculated from T-scores, or the variance from the mean of an aged-matched population [17].
Fracture risk prediction can also be enhanced by incorporating additional risk factors into the assessment of fracture risk. As risk factors for fracture increase, the risk for fracture also increases above and beyond the risk predicted by low BMD and increased age alone. The validation of how additional risk factors should be added to BMD to enhance risk prediction is important, since the current DXA reports may be misleading in their subjective pronouncements of fracture risk.
Effect of Age on Fracture Risk
It has been recognized since the forearm DXA studies of Hui et al [3] that fracture risk is dependent on the age of the patient (Fig. 3.1). Any given patient’s risk for fracture increases as age increases, even at the same BMD or T-score level [28]. Thus, DXA measurements capture an important, albeit small, part of the fracture risk. Understanding this fundamental point is pivotal to the proper interpretation of BMD values. The reason why risk is greater as age increases is not completely understood, but the higher risk for falls in the elderly may account for a portion of this age-related greater risk for fracture [29,30]. Older bone has less strength to resist fracture than younger bone at the same BMD or T-score, and investigators dedicated to measuring bone quality are refining our understanding of these issues [31]. It is important to point out, however, that even though the absolute risk for fragility fracture increases at the same level of BMD or T-score as age increases [32], fractures at both hip and nonhip skeletal sites are not infrequent in the younger (50–64 years), postmenopausal population. In the NORA study nearly 37% of all fractures occurred in this younger, untreated, postmenopausal group and was lower the lower the T-score value [33].
Combined Effect of Risk Factors
As previously mentioned, prior fracture in the postmenopausal population is an independent predictor of future fracture risk. Furthermore, combining a prevalent fracture (even an asymptomatic VCF) and low BMD translates into a much greater risk for future fracture than what would be predicted by low BMD or prior fracture alone [15]. Adding risk factors enhances risk prediction.
In 1993, data showed the interaction of risk factors captured in the Study of Osteoporotic Fractures (SOF) with low BMD to enhance fracture risk prediction for hip fractures [34]. More recently, data from multiple population studies have documented the strong association between the presence of nonvertebral or nonhip fractures and fragility fractures of other skeletal sites, including shoulder, wrist, and rib [13,14,35,36]. Therefore, in the
elderly population, any fragility fracture is symbolic of systemic skeletal fragility.
elderly population, any fragility fracture is symbolic of systemic skeletal fragility.
Clinicians should, therefore, incorporate BMD, age, and prior fracture in their assessment of fracture risk and patient management. Recent software upgrades in central DXA machines may use these three risk factors to calculate fracture risk. Broad implementation of standardized DXA reports can only be realized when the independent risk factors for fragility fractures in the postmenopausal population are validated and endorsed at an international level.
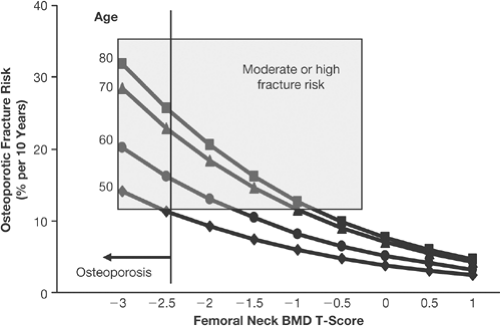
The World Health Organization Absolute Risk Project
The World Health Organization’s (WHO’s) absolute risk project is the large project assessing the long-term (10-year) risk for all fragility fractures as a function of validated risk factors from large international studies [28]. This work, spearheaded by Professor John Kanis, is still in progress and will require review and comment by the WHO per se before final publication and ultimate implementation [37]. Based on data that have already been presented at many scientific meetings, there are eight independent validated risk factors for fracture risk. Those that may be included in the implementation of standardized DXA reports are BMD, prior fragility fracture, age, and family history, since beyond 4 or 5 risk factors, the absolute risk level increases only slightly. The combined risk factor analysis refines risk stratification. When implemented, it is hoped that absolute risk prediction calculation will facilitate intervention decisions for the postmenopausal population based on risk beyond a T-score value alone. Risk stratification has been shown in previous analysis; however, they are either based on restricted population studies or use peripheral BMD technologies for risk assessment [38,39]. The WHO absolute risk study will link absolute risk for all fractures, calculated from validated population studies representing more than 90,000 postmenopausal women, to treatment intervention based on disutility costs of hip fracture using the current costs of drugs registered for the treatment of postmenopausal osteoporosis (PMO).
It is obvious that the government reimbursement plan will differ from nation to nation by the gross domestic product (GDP) of a given nation. The WHO project does not include other risk factors that clinicians might reasonably use in counseling patients: nonclinical (morphometric) vertebral fractures, bone turnover markers, hip axis length, hip structural analysis, and other risk factors that might become identified in smaller, less well-validated multination population studies [6,40,41,42,43,44,45,46,47,48]. Morphometric vertebral fractures, however, will be acknowledged by the National Osteoporosis Foundation (NOF) clinical implementation of the WHO absolute risk analysis as being a strong risk factor for future fracture. In addition, the WHO absolute risk model will provide broad generalizations that will focus on intervention strategies, but it will not eliminate individual clinician decisions. Nevertheless, the WHO risk project will take the field of osteoporosis to a level comparable to the cardiovascular field regarding intervention
decisions. In addition, the WHO absolute risk assessment may advocate treatment of women whose lower T-scores or younger age might otherwise have discouraged their healthcare providers from prescribing treatment for them [27] (Fig. 3.3).
decisions. In addition, the WHO absolute risk assessment may advocate treatment of women whose lower T-scores or younger age might otherwise have discouraged their healthcare providers from prescribing treatment for them [27] (Fig. 3.3).
The WHO selected absolute risk rather than relative risk, even though both calculations of risk have value. The power of any given BMD measurement device to predict risk is based on its ability to predict RR. Yet, RR does not incorporate other risk factors; it is the ratio of the absolute risk for the disease event in a target population to the absolute risk in a population not at risk for the disease event (BMD, smoking, etc.). Absolute risk incorporates the discovered cumulative risk factors into the prediction of the risk for fractures over a given period of time [49] (Table 3.2). As shown in Table 3.2, the relative risk for fracture per SD reduction in BMD is constant over age, which is incorrect. As other risk factors are included in this calculation, the absolute risk will increase with age.
Risk Determined By Vertebral Fracture Assessment
DXA is now a recognized technology for the identification of vertebral fractures. The presence of vertebral fractures, even if they are asymptomatic, is predictive of the risk for future (incident) vertebral fractures and nonvertebral fractures, independent of baseline BMD or T-score. In
addition, many patients without WHO-defined osteoporosis have prevalent VCFs [50]. The majority of prevalent VCFs are not recognized in postmenopausal women and elderly men. Population studies from the United States, Europe, Mexico, and Asia all suggest that VCF prevalence is similar across these ethnic groups and may be as high as 60% to 65% by the age of 65 years [51,52,53,54,55]. This suggests that osteoporosis is markedly underdiagnosed and that future fracture risk is markedly underestimated. Professor Harry Genant [56] has provided clinicians with a semiquantitative method for the identification of prevalent, as well as incident, vertebral clinical fracture (VCF) utilizing either plain radiography or DXA-based vertebral fracture assessment (VFA). The VFA technology for prevalent VCF detection by DXA has progressed to the point that it is becoming a standard of care in the risk assessment of the postmenopausal population. The International Society for Clinical Densitometry (ISCD) has provided guidelines for VFA determinations [57]. The ISCD indications for VFA by DXA are as follows [57]:
addition, many patients without WHO-defined osteoporosis have prevalent VCFs [50]. The majority of prevalent VCFs are not recognized in postmenopausal women and elderly men. Population studies from the United States, Europe, Mexico, and Asia all suggest that VCF prevalence is similar across these ethnic groups and may be as high as 60% to 65% by the age of 65 years [51,52,53,54,55]. This suggests that osteoporosis is markedly underdiagnosed and that future fracture risk is markedly underestimated. Professor Harry Genant [56] has provided clinicians with a semiquantitative method for the identification of prevalent, as well as incident, vertebral clinical fracture (VCF) utilizing either plain radiography or DXA-based vertebral fracture assessment (VFA). The VFA technology for prevalent VCF detection by DXA has progressed to the point that it is becoming a standard of care in the risk assessment of the postmenopausal population. The International Society for Clinical Densitometry (ISCD) has provided guidelines for VFA determinations [57]. The ISCD indications for VFA by DXA are as follows [57]:
Consider VFA when the results may influence clinical management.
When BMD measurement is indicated, performance of VFA should be considered in clinical situations that may be associated with vertebral fractures. Examples include:
Documented height loss of more than 2 cm (0.75 in.) or historical height loss of more than 4 cm (1.5 in.) since young adulthood
History of fracture after age 50 years
Commitment to long-term oral or parenteral glucocorticoid therapy
History of findings suggestive of vertebral fracture not documented by prior radiologic study
Table 3.2. Limitations of relative risk | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
If clinicians simply measure the height of their postmenopausal patients and perform a VFA in those who have lost more than 4 cm (1.5 in.) from their historical height, there is evidence that a large proportion of vertebral fractures will be detected [58].
Data suggest that all “grades” of prevalent vertebral fractures are predictive of future fracture and that this risk is increased within 12 months of the detection—even though the physician may not know when the prevalent vertebral fracture occurred [6,42,59,60]. The higher the grade (severity) of the existing vertebral fracture, or the more vertebral fractures present (one, two, or three), the greater the risk for future fractures. Furthermore, since these vertebral fractures, even those that are asymptomatic, are associated with a high risk of fractures even at nonvertebral sites, and are also associated with a higher morbidity and mortality as compared with age-matched patients without vertebral fractures, the detection of VCF will not only establish a diagnosis of osteoporosis regardless of the prevailing T-score [48] but will also identify a high risk for fracture group that merits treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree