Arthroscopic Partial Repair of the Rotator Cuff
Patrick J. Denard
Stephen S. Burkhart
INDICATIONS/CONTRAINDICATIONS
With adherence to mechanical principles and proper tear pattern recognition, the vast majority of rotator cuff tears, including massive rotator cuff tears, can be completely repaired arthroscopically. However, there exists a subset of patients whose rotator cuff tears are considered “irreparable.” Historically, such patients were treated nonoperatively or with acromioplasty and débridement alone. While these methods frequently result in temporary pain relief, functional improvement was unpredictable and results deteriorated with time (1, 2).
The concept of partial rotator cuff repair evolved from the observation of patients who appeared to be “copers,” that is, had normal function despite large rotator cuff tears. Such tears, termed “functional rotator cuff tears,” have normal function by satisfying five biomechanical criteria (3):
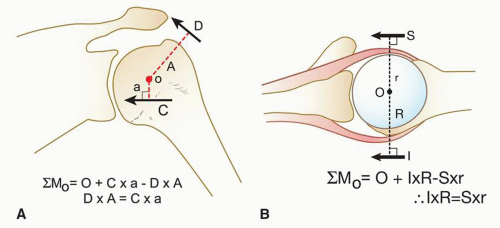
Force couples must be balanced in the coronal and transverse planes (Fig. 4-1).
A stable fulcrum kinematic pattern must exist.
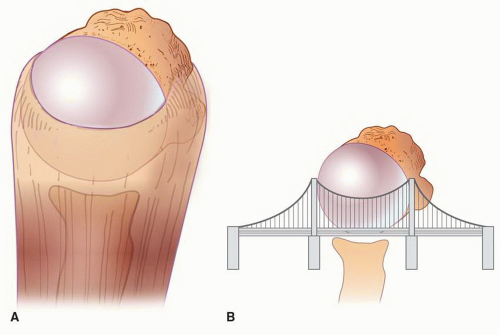
The shoulder’s “suspension bridge” must be intact (Fig. 4-2).
The tear must occur through a minimal surface area.
The tear must possess edge stability.
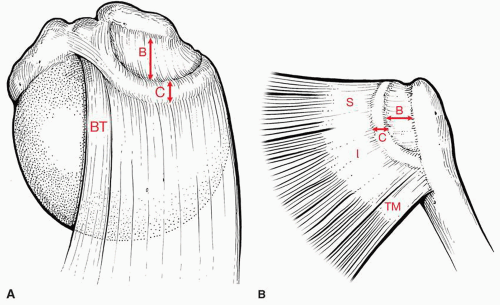
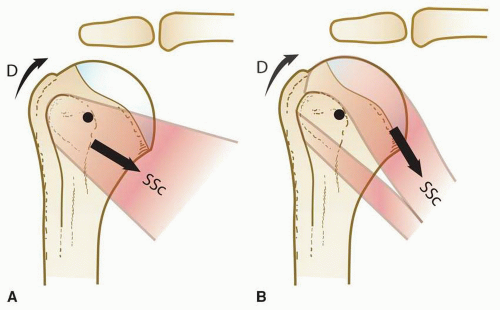
In a patient whose massive, dysfunctional rotator cuff tear is not completely repairable, the goals of partial rotator cuff repair are to effect enough of a repair to regain overhead function, to improve strength with the arm at the side, and to achieve pain relief. A biomechanical study quantified the increased force required for the subscapularis and infraspinatus and teres minor to maintain stable glenohumeral abduction as tear size increases (4). Subscapularis force requirements increased by 45% in a 7-cm tear and 86% in an 8-cm tear; similar measurements were reported for the posterior cuff. Viewed another way, a reduction in tear size by as little as 1 cm may result in a near 50% reduction in force requirements. Thus, restoring overhead function may be achieved by partial repair that balances the force couple between the anterior and posterior portions of the shoulder; typically, this requires an intact subscapularis tendon anteriorly and an intact inferior half of the infraspinatus tendon posteriorly. Anatomically, this corresponds to the anterior and posterior attachments of the rotator cable (Fig. 4-3). It is important to understand that while there has been much recent interest in biologic augmentation materials, simply “covering the hole” will not restore force couples. Moreover, partial rotator cuff repair is preferable to tendon transfer because the former respects and preserves the normal mechanics of the rotator cuff, whereas tendon transfers adversely affect shoulder mechanics (Fig. 4-4).
The indications for partial rotator cuff repair comprise persistent pain and dysfunction due to any rotator cuff tear that is not completely repairable. Obviously, a complete rotator cuff repair is the primary goal of surgery. However, this can only be determined intraoperatively, and thus the indications for partial rotator cuff repair are similar to those for any rotator cuff tear. Partial repairs are recommended whenever complete closure of the defect is not possible.
There are few contraindications for partial rotator cuff repair. In low-demand elderly patients with preoperative functional rotator cuff tears, who require pain relief only and who are unable to protect the repair postoperatively, or who do not wish to participate in a long rehabilitation program, the surgeon may consider a subacromial decompression, biceps tenodesis or tenotomy, and débridement alone. Advanced cuff tear
arthropathy is a relative contraindication to arthroscopic partial rotator cuff repair, and these patients are often more likely to benefit from arthroplasty. In addition, arthroscopic partial rotator cuff repair is contraindicated in patients with significant permanent neurologic deficits or medical conditions precluding surgery.
arthropathy is a relative contraindication to arthroscopic partial rotator cuff repair, and these patients are often more likely to benefit from arthroplasty. In addition, arthroscopic partial rotator cuff repair is contraindicated in patients with significant permanent neurologic deficits or medical conditions precluding surgery.
PREOPERATIVE PLANNING
The clinical presentation of patients with rotator cuff tears that are only partially repairable is similar to those for whom complete rotator cuff repair is possible. However, patients are often older with a prolonged history of pain in the anterolateral aspect of the shoulder. Pain is typically aggravated by repetitive use of the arm overhead, and in chronic cases, pain can be constant with a significant component of night pain. In patients whose tears are only partially repairable, symptoms are usually prolonged, severe, and functionally disabling.
Physical examination in these massive tears demonstrates atrophy of the supraspinatus and infraspinatus muscles, tenderness over the anterolateral humerus, and palpable subacromial crepitus. Although passive range of motion is generally at or near normal, active range of motion is typically significantly limited, with many patients demonstrating only a shoulder “shrug.” Strength is limited. An external rotation lag sign indicates involvement of the infraspinatus tendon, while a horn-blower’s sign may be used to detect teres minor involvement (5, 6). Subscapularis tear size may be estimated by the bear-hug and belly-press tests that may be positive in tears of the upper 30% and the liftoff that does not become positive until tears greater than 75% of the subscapularis (7).
We routinely obtain five views of the shoulder (anteroposterior [AP]) views in internal and external rotation, axillary view, outlet view, 30-degree caudal-tilt view] preoperatively in all shoulder patients. The AP view commonly shows sclerosis of the undersurface of the acromion and sclerosis and cystic changes in the region of the greater tuberosity. Acromioclavicular joint arthritis may be variably present. In massive tears, patients may demonstrate proximal migration of the humerus. We do not consider proximal migration alone a contraindication for partial rotator cuff repair. In some cases, the proximal migration may actually be reversed following repair. In most cases, the absence of adaptive changes of the greater tuberosity, the “rounding off” of the tuberosity occurring from acromial articulation, is a good prognostic sign for obtaining a successful repair.
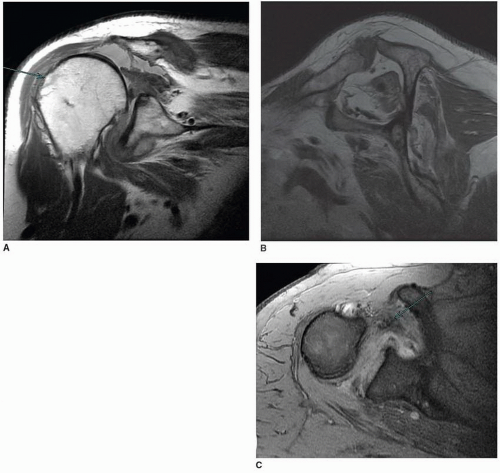
An MRI can provide information on tear size, tear configuration, and tendon involvement, as well as findings to suggest whether a massive rotator cuff tear is potentially repairable (8). Combined tear length greater than 2 cm on coronal images and width greater than 2 cm on the sagittal images suggests that interval slides or partial repair will be necessary in over 75% of cases (Fig. 4-5). Combined length and width greater than 3 cm predicts the need for interval slides or partial repair in all cases. Careful evaluation of the axial views also is necessary to identify subscapularis tendon involvement, which significantly increases the complexity of repair (Fig. 4-5C). Although nonretracted tears of the subscapularis tear are harder to appreciate, medial biceps subluxation virtually always indicates a tear of the upper tendon border. An MRI may also demonstrate a spinoglenoid ganglion cyst, which can cause symptoms that mimic a rotator cuff tear.
Some authors have advised against repairing tears with Goutallier grade III (50% fatty infiltration) or higher (2, 9). We do not feel that fatty degeneration is a contraindication to surgical repair (Fig. 4-5B).
The senior author has demonstrated that individuals with 50% to 75% fatty degeneration can reliably obtain improvement in function and that even individuals with greater than 75% fatty degeneration can sometimes functionally improve with repair (10). Additionally, while we agree with the current trend toward repairing symptomatic rotator cuff tears as soon as possible, in our experience, patients have shown marked improvement even when undergoing repair of chronic tears more than 10 years after initial injury (11).
The senior author has demonstrated that individuals with 50% to 75% fatty degeneration can reliably obtain improvement in function and that even individuals with greater than 75% fatty degeneration can sometimes functionally improve with repair (10). Additionally, while we agree with the current trend toward repairing symptomatic rotator cuff tears as soon as possible, in our experience, patients have shown marked improvement even when undergoing repair of chronic tears more than 10 years after initial injury (11).
SURGERY
The principles and techniques used for arthroscopic partial rotator cuff repair are the same as those used when the rotator cuff tear is completely repairable. Although massive tears are technically demanding and may require advanced techniques, the essential elements of any arthroscopic rotator cuff repair are the following:
Visualization
Angle of approach
Creating a stable construct
Tear pattern recognition
Visualization
During arthroscopic shoulder surgery, nothing is more frustrating than poor visualization. Particularly in the subacromial space, bleeding can obscure visualization and frustrate attempts to obtain an effective rotator cuff repair. To maximize visualization, we use several techniques. First, the patient’s systolic blood pressure is maintained below 100 mm Hg (preferably less than 90 mm Hg) if not medically contraindicated. Second, we routinely maintain the subacromial pressure at 60 mm Hg using an arthroscopic pump. If bleeding occurs, the pressure may be temporarily increased up to 90 mm Hg to tamponade bleeding or to enhance visualization until bleeding is controlled. However, the duration of high subacromial pump pressures is restricted to minimize subcutaneous swelling. Electrocautery may be used to cauterize bleeding, although this can sometimes be difficult and time-consuming. Most important, careful attention must be paid to fluid leakage from noncannulated portals. Fluid flow from these portals creates a suction effect by virtue of the Bernoulli principle and draws blood into the subacromial space. Simply blocking these portals using digital pressure will facilitate a clear view by controlling turbulence within this closed system. In general, outflow cannulas are not used because they increase turbulence and exaggerate the Bernoulli effect.
Angle of Approach
The proper angle of approach is essential in repairing any rotator cuff tears. One of the great advantages of arthroscopy compared to open shoulder surgery is the ability to reach all areas of the shoulder with different arthroscope angles and portals. Although most surgeons primarily rely on the 30-degree arthroscope, we frequently use a 70-degree arthroscope. The acute angle of the 70-degree arthroscope is particularly valuable in performing advanced techniques such as subscapularis repair, subcoracoid decompression, and interval slides.
Portal placement is critical to the angle of approach, and for that reason, with the exception of the initial posterior portal, we use an 18-gauge spinal needle to precisely establish all portals in an outside-in fashion. The three standard portals that are used during arthroscopic rotator cuff repair are posterior, anterior, and lateral subacromial. An anterosuperolateral portal is also required for subscapularis tendon repair. In addition to the most commonly used portals for arthroscopic repair, one should not hesitate to establish accessory portals for anchor placement or suture passage if the standard portals (combined with manipulation of the arm) do not afford a proper angle of approach. We commonly place anchors for instance through small percutaneous incisions to achieve the proper “deadman” angle (12).
Posterior Portal
Many surgeons create a posterior portal 1 to 2 cm inferior and 1 to 2 cm medial to the posterolateral corner of the acromion. We feel this location is too lateral and superior. During longer cases such as massive rotator cuff repairs, subcutaneous swelling will cause the skin incision to shift superiorly and laterally. We establish a posterior portal by palpating the soft spot of the glenohumeral joint and enter the joint at or just below the equator of the humeral head. The exact position varies from patient to patient but is approximately 4 cm inferior and 4 cm medial to the posterolateral corner of the acromion. This portal is used for initial glenohumeral arthroscopy, and the same skin puncture is used for viewing and working in the subacromial space.
Anterior Portal
This is established using an outside-in technique just superior to the lateral half of the subscapularis tendon for diagnostic glenohumeral arthroscopy. This same skin puncture can be used as an anterior working portal and inflow subacromial portal and can be used during distal clavicle resection if indicated.
Lateral Subacromial Portal
This portal is approximately 4 cm lateral to the lateral aspect of the acromion, in line with the posterior border of the clavicle. One must ensure that the portal is parallel to the undersurface of the acromion. This portal serves as a viewing and working portal in the subacromial space.
Anterosuperolateral Portal
This portal is created in the presence of a subscapularis tear. It is established through the rotator interval just anterior to the supraspinatus tendon and directly above the long head of the biceps. The point of entry is approximately 1 to 2 cm lateral to the anterolateral corner of the acromion. The placement should allow a 5- to 10-degree angle of approach to the lesser tuberosity and should be parallel to the subscapularis tendon. This angle of approach is perfect for performing arthroscopic coracoplasty.
Creating a Stable Construct
Advances in technology have allowed us to transfer the weak link in rotator cuff repair from implants to the rotator cuff tissue itself. Several principles under the surgeon’s control are important to consider to optimize biomechanical stability including anchor properties, suture properties, knot tying, and margin convergence.
Traditional open repair relied on transosseous tunnels for fixation of the rotator cuff to bone. However, transosseous fixation is susceptible to failure under cyclic load through cutting of suture through metaphyseal bone. In contrast, under cyclic loading, suture anchors fail by cutting of suture through the tendon. Minimizing suture cutout can best be achieved by increasing the number of fixation points (Fig. 4-6). This is particularly relevant in massive rotator cuff repairs where tissue quality is often less than ideal. Anchor pullout strength is optimized when the angle of insertion (deadman’s angle) and tension reduction angle are both less than or equal to 45 degrees. A
final anchor factor to consider is suture abrasion that occurs through the anchor eyelet or against the anchor surface itself. Abrasion is minimized by using biodegradable anchors (compared to metal anchors) with a flexible suture loop eyelet. Our current workhorse anchor of choice in rotator cuff repair is the BioComposite Corkscrew-FT (Arthrex Inc., Naples, FL), which is a fully threaded biocomposite anchor with a no. 5 polyester suture eyelet.
final anchor factor to consider is suture abrasion that occurs through the anchor eyelet or against the anchor surface itself. Abrasion is minimized by using biodegradable anchors (compared to metal anchors) with a flexible suture loop eyelet. Our current workhorse anchor of choice in rotator cuff repair is the BioComposite Corkscrew-FT (Arthrex Inc., Naples, FL), which is a fully threaded biocomposite anchor with a no. 5 polyester suture eyelet.
We use only permanent sutures in rotator cuff repair. The healing time of rotator cuff repairs is beyond the viability of resorbable sutures. We use no. 2 Fiberwire (Arthrex Inc.), which is a polyblend suture shown to have higher load to failure and less susceptibility to suture abrasion than no. 2 Ethibond (Ethicon, Somerville, NJ). Several other current generation polyethylene sutures are also commercially available.
Secure knot tying relies on achieving knot security and loop security. Knot security, which is the effectiveness of the knot at resisting slippage, depends on friction, internal interference, and slack between throws. Loop security is the ability to maintain a tight suture loop around tissue as the knot is tied. Sliding knots can potentially damage the tendon as they slide through the rotator cuff or abrade and weaken the suture as they slide against the eyelets of the anchors (especially metal anchors). We tie strictly an arthroscopic surgeon’s knot, which is a static (nonsliding) knot composed of a base of three half-hitches in the same direction, followed by three reversing half-hitches on alternating posts. This knot has demonstrated the highest combination of knot and loop security compared to commonly used sliding knots. We also use a double-diameter knot pusher (Surgeon’s Sixth Finger; Arthrex Inc.), which allows the tissue to be secured and manipulated into place. Most importantly, continuous tension can be maintained on the post limb as knots are tied to prevent loosening of the soft-tissue loop between throws (i.e., loop security) as successive half-hitches are thrown. Although the Surgeon’s Sixth Finger has an initial learning curve, once mastered, it is highly efficient and has demonstrated superior loop security compared to knots tied with a single-diameter knot pusher (13).
For knot tying, a translucent cannula is valuable. When there is significant deltoid or adventitial swelling, knots may be tied entirely within the cannula. Before tying, retrieve both limbs out a separate cannula and hold all other sutures in temporary holding portals. When pushing half-hitches down the inner metallic sleeve of the Sixth Finger knot pusher, unravel any twists in the suture by turning the outer plastic sleeve followed by past-pointing to tighten each throw. In this way, knot security is maximized by minimizing slack between throws. Switching posts can be easily performed without rethreading, by flipping the half-hitch through differential tensioning of the suture limbs. Since the post limb is always the limb under the most tension, the wrapping limb can be converted to the post limb by tensioning it to a greater degree than the original post limb, thereby “flipping” the post. This is not only easy but it also optimizes the strength of any knot. Tissue indentation by the suture is a final indicator of good loop security.
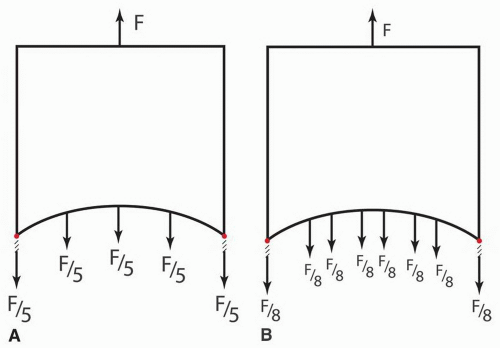
Despite technological advances, one of the simplest and most important biomechanical principles in massive rotator cuff repair is margin convergence by side-to-side suturing. The technique of “margin convergence” not only allows repair of seemingly irreparable tears but also minimizes strain at the repair site. This theoretically decreases the risk of rerupture and subsequent failure of the rotator cuff repair. In the case of a U-shaped tear (discussed below), margin convergence along two-thirds of its length reduces strain to one-sixth the original value (Fig. 4-7) (14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree