Arthroscopic Distal Clavicle Excision
Jeffrey S. Abrams
The acromioclavicular joint (ACJ) can be a common source of joint pain. This diarthrodial joint can be traumatized resulting in articular injury and potential instability. Following Mumford and Gurd’s independent descriptions of open resection, the operation has undergone changes to be performed using arthroscopic techniques (1, 2). The advantages of arthroscopy include a minimally invasive technique that does not disturb the deltotrapezial fascia, preservation of the ACJ capsule, reduce morbidity allowing for earlier functional recovery, and can be combined with treatment of articular pathology. Minor forms of acromioclavicular instability have been treated with nonoperative treatment or distal clavicle resection (3). As greater degrees of distal clavicle subluxation are noted (i.e., grade III separation), resection of distal clavicle alone is insufficient treatment. The purpose of this section is to address the articular resection of the ACJ.
The ACJ capsule has been studied and extends between 1.5 and 2.0 cm medially (4). Resection of distal clavicle has been reduced from the original description of 2 cm of clavicle removal in order to avoid destabilization. There have been two arthroscopic approaches popularized: direct and indirect. The direct approach is an isolated intracapsular resection of the distal clavicle with a superior viewing portal. The indirect approach is a subacromial approach entering and viewing the ACJ from the inferior aspect. The advantage of the indirect approach is the ability to combine this operation with other procedures, including a subacromial decompression and rotator cuff repair. A common clinical situation that suggests a direct approach is the management of an isolated problem, as in osteolysis of the distal clavicle. Both surgical approaches emphasize preservation of the ACJ capsule and surrounding soft-tissue attachments.
INDICATIONS/CONTRAINDICATIONS
The most common indication for arthroscopic excision of the distal clavicle is pain originating from the ACJ that has not responded to nonoperative management. The pain can be isolated to the superior and lateral aspect of the shoulder or potentially radiate proximally along the trapezius to the cervical region. Cross-chest movement, reproduced when removing a shirt or taking off a sweater, can often increase pain. Applying direct digital pressure on the joint can reproduce pain and tenderness. It is frequently helpful to palpate both AC joints simultaneously, noting if there is asymmetry in the clinical response to palpation. It is important for the examining physician to appreciate that this problem can be combined with other pathology (i.e., rotator cuff tears, superior labrum anterior and posterior [SLAP] tears). The physical examination and mechanism of injury can raise suspicion of additional diagnosis.
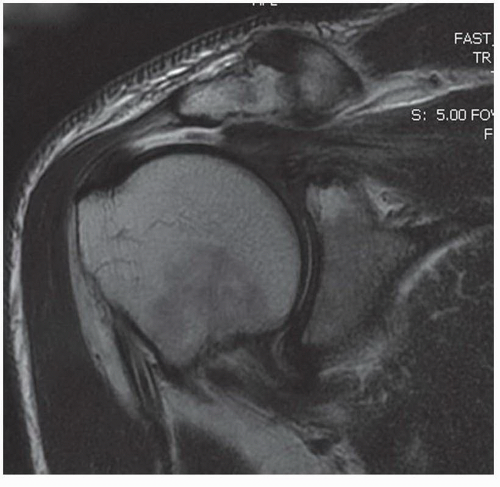
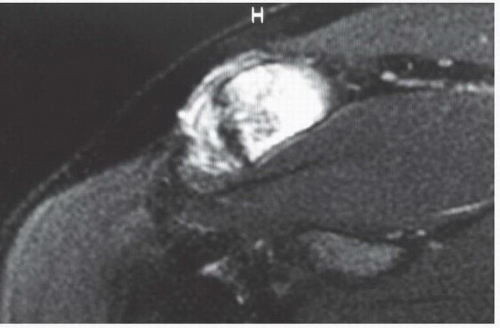
Indications for surgical treatment include degenerative arthritis, osteolysis of the distal clavicle, and rheumatoid arthritis. Rotator cuff tears can develop in conjunction with an arthritic ACJ (Fig. 2-1). Relative contraindications to arthroscopic distal clavicle resection are patients with symptomatic instability of the ACJ. These patients may require surgical stabilization of the coracoclavicular and acromioclavicular attachments. Select patients with mild instability, that is, grade I, can be considered for nonoperative management or distal clavicle excision (3). Another relative contraindication may be large extracapsular bone deformity. Here, in addition to excision, one may choose to reconstruct the soft-tissue attachments, which is often easier to perform with an open surgical procedure.
PREOPERATIVE PLANNING
Proper patient selection for distal clavicle excision is determined with history, physical exam, and imaging studies. Some patients with ACJ degenerative joints have additional pathology (i.e., rotator cuff tears or SLAP lesions). Examination and identification of additional pathology are an important part of planning your procedure.
The major benefit of distal clavicle excisions is to eliminate contact with the medial margin of the acromion and to reduce subacromial crowding of the rotator cuff muscle and tendons. The diagnosis is designed by clinical exam and confirmed by radiologic studies. Imaging studies play a role in preoperative planning. Patients may have a complex diagnosis that includes the ACJ, which may be confusing. A local injection into the ACJ may help identify this component of pain, relieved with injection. Patients being considered for ACJ resection should have a trial of nonoperative treatment prior to considering surgical intervention.
Radiographs of the shoulder should be obtained in three views: anteroposterior to the ACJ, transcapular or Y view, and axillary view. Here, the morphology of the acromial arch can be examined. Certain anatomic variants can be encountered (i.e., mesoacromion or an open physis, called an os acromiale) or increase bone inflammatory activity (Figs. 2-2 and 2-3). This is important to consider when selecting patients prior to surgery.
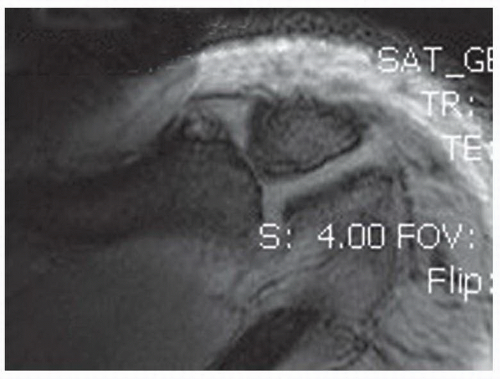
The surgical approach to the distal clavicle may be directly from a superior viewing portal in an isolated pathology, that is, osteolysis of the distal clavicle, or from a subacromial or bursal approach, when impingement is felt to be a component requiring treatment. The majority of cases of distal clavicle excision are approached from the inferior border of the clavicle, viewing from the subacromial bursae. When a direct approach is being considered in a patient with osteolysis, a space between the clavicle and the acromion makes entrance into the joint more accessible (Fig. 2-4). In patients with hypertrophic degenerative arthritis, there is minimal spacing and the indirect bursal approach is preferred when using standard arthroscopic equipment (Fig. 2-5).
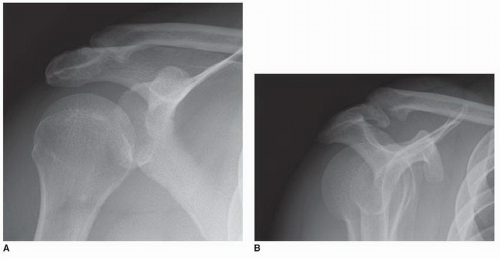 FIGURE 2-5 Degenerative changes of the ACJ. A: Oblique-oriented, narrow joint. B: Outlet view demonstrating inferior osteophytes. |
Additional imaging is helpful to identify coexistent pathology. In North America, MRI and ultrasound are commonly used to diagnose rotator cuff, biceps, articular cartilage, and other soft-tissue problems. These studies commonly identify age-related changes in the ACJ. The coronal views may demonstrate significant muscle impression in a supine patient (Fig. 2-1). The sagittal views demonstrate the outlet appearance of the subacromial arch. The transverse views can identify an os acromiale, cysts in the distal clavicle, and signs of advanced degenerative changes. Following examination and imaging studies, informed consent of the preoperative plan and treatment of encountered pathology should be completed.
Instrumentation for distal clavicle excision includes the following
Arthroscopic viewing: Most indirect approaches use a standard 4.5 scope and direct approaches a small 2.7-mm scope.
Shaving system: Soft-tissue resector and a burr (4.0 or 5.5) are used to perform resection. Small burrs 2 and 3.5 are available for a direct approach.
Electrocautery provides a clear visual field to identify proper landmarks, resect bone, and reduce the risk of heterotopic ossification.
Saline pump to assist with visualization, irrigation, and removal of debris.
One of the challenges of bursal surgery in the shoulder is hemostasis. This is best achieved with controlling the patient’s blood pressure, managing irrigation and suction of saline, and cauterizing the bleeding vessel during the procedure. Newer forms of anesthesia including combined neurologic blocks with sedation have reduced the need for pain medication. The blood pressure can be maintained at moderate levels throughout the procedure with less analgesic medications. Elderly patients and patients with increased risk factors should have a predetermined safe range for their blood pressure. Judicious use of cautery and creating an independent inflow cannula can provide flexibility to control bleeding. Special care in monitoring blood pressure in a sitting or beach-chair position is important to obtain reliable measurements during the procedure.
Patients with multiple medical problems and elevated risk factors should undergo preoperative consultation and planning. These discussions should include treating medical physicians, anesthesiologist, and surgeons. Anticipating problems can be helpful in the intraoperative and postoperative periods.