Arthroscopic Capsular Releases for Loss of Motion
Ruth A. Delaney
Ryan W. Simovitch
Lindsay R. Miller
Laurence D. Higgins
DEFINITION
Shoulder stiffness can be a function of soft tissue scarring and contracture or osseous changes.
The stiff or frozen shoulder has been given the name adhesive capsulitis.
There is no consensus on the definition of adhesive capsulitis, but it is generally agreed to be a condition with functional restriction of active and passive shoulder motion without an osseous basis for this limitation.18
Its key distinguishing feature is restriction of passive external rotation in the face of a normal glenohumeral joint on radiograph.4
An exception to this statement is that calcific tendinitis may be seen on radiograph.
There are principally two forms of adhesive capsulitis that result in loss of range of motion and can be safely addressed by arthroscopic releases:
Primary adhesive capsulitis (idiopathic)
Secondary adhesive capsulitis
Intrinsic
Associated with, for example, rotator cuff disorders, calcific tendinitis, biceps tendinitis, previous shoulder surgery, or proximal humerus fracture
Extrinsic
Remote or local abnormality extrinsic to the glenohumeral joint such as prior ipsilateral breast surgery, cervical radiculopathy, previous humeral shaft fracture, scapulothoracic abnormality, acromioclavicular arthritis, or clavicle fracture
Systemic
Associated with disorders such as diabetes mellitus and less commonly hyperthyroidism, hypothyroidism, hypoadrenalism, or even myocardial infarction
Shoulder stiffness can result from intra-articular adhesions, capsular contracture, subacromial adhesions, and subdeltoid adhesions.
The essential tenet of treating the stiff shoulder is recognizing the anatomic region responsible for the stiffness and releasing the specific structures in this region in a controlled fashion.
An adequate appreciation of anatomy is key to restoring motion and avoiding injury to accompanying tendons and nerves.
ANATOMY
Shoulder motion occurs principally along two interfaces:
Glenohumeral articulation
Scapulothoracic articulation
On average, the normal ratio of glenohumeral motion to scapulothoracic motion is 2:1, with the majority of elevation occurring through the glenohumeral joint.
Capsuloligamentous structures contribute to stability of the shoulder joint and act as checkreins at the extremes of motion in the nonpathologic state.
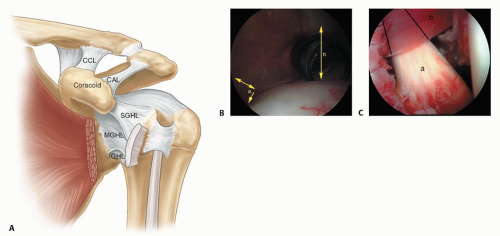
Many areas within the capsule are thickened and contain the glenohumeral ligaments (FIG 1A):
Superior glenohumeral ligament
Coracohumeral ligament
Middle glenohumeral ligament
Inferior glenohumeral ligament complex
Anterior band
Axillary fold
Posterior band
The rotator interval is a triangular region between the anterior border of the supraspinatus tendon and the superior border of the subscapularis. It contains the superior glenohumeral ligament and the coracohumeral ligament.
During shoulder motion, tightening and loosening of the glenohumeral ligaments and capsule are accompanied by lengthening and shortening of the rotator cuff and deltoid muscles.
A plane between the deltoid and humerus (subdeltoid) exists that, when scarred, can limit glenohumeral motion.
A plane between the rotator cuff and acromion exists and is occupied normally by a subacromial bursa.
Scar tissue and adhesions in this interface can limit excursion of the rotator cuff and thus glenohumeral joint motion (FIG 1B).
Several structures that are important to preserve are in continuity or proximity to the regions of the capsule that are released arthroscopically in the stiff shoulder.
The subscapularis tendon is superficial to the middle glenohumeral ligament. The superior two-thirds of the subscapularis is intra-articular.
The biceps tendon courses through the rotator interval.
The axillary nerve runs adjacent to the inferior border of the subscapularis and then is juxtaposed to the inferior glenohumeral ligament and capsule as it exits the quadrangular space (FIG 1C).
The posterior capsule overlies a distinct layer of rotator cuff muscle posteriorly adjacent to the glenoid.
The posterior rotator cuff tendons and capsule are juxtaposed and virtually indistinguishable more laterally.
Release of the posterior capsule should be done adjacent to the glenoid to avoid rotator cuff muscle and tendon disruption.
Contracture of specific capsular regions and ligaments correlates with specific clinical losses of range of motion. This must be determined preoperatively to guide arthroscopic release (Table 1).
Table 1 Contracture of Specific Capsuloligamentous Regions and Their Influence on Shoulder Motion | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
PATHOGENESIS
Shoulder stiffness can be primary or secondary.
Primary stiffness is often termed adhesive capsulitis.
Adhesive capsulitis, also referred to as frozen shoulder, can be idiopathic and is more common in women.
Secondary stiffness occurs as a result of scar formation and adhesions after trauma or surgery of the shoulder as a result of disruption of soft tissue, release of cytokines, and the body’s inflammatory response seen after injury.
Secondary stiffness can also result iatrogenically, as would be the case after a Putti-Platt or Magnuson-Stack procedure.
The pathogenesis of frozen shoulder has been divided into three stages (Table 2). The stages coexist as a continuum and occur over a variable time course in individual patients.
NATURAL HISTORY
Although the natural history of secondary shoulder stiffness is relatively accepted as protracted and refractory to nonoperative treatment, the time course and end result of adhesive capsulitis (primary and secondary) are more controversial.
In the absence of operative intervention, recent reports have shown measurable restrictions in range of motion at follow-up in 39% to 76% of patients,3,11,13 in addition to persistent symptoms in up to 50% of patients2 with adhesive capsulitis.
Adhesive capsulitis can be protracted, with the mean duration of symptoms of 30 months.13
There is a weak correlation between restricted range of motion and pain.
Some patients have severe pain but near-normal range of motion.
Some patients have very restricted range of motion but no pain.
In one study, restricted range of motion was found in more than 50% of patients with adhesive capsulitis, but functional deficiency was identified in only 7% of the patients.13
The impact of restricted range of motion or pain on an individual patient’s quality of life largely depends on that patient’s functional demands.
Adhesive capsulitis in diabetics tends to be more protracted and more resistant to nonoperative treatment than idiopathic adhesive capsulitis.
Table 2 Pathogenesis of Frozen Shoulder | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with idiopathic adhesive capsulitis often deny a traumatic event but complain of the insidious onset of pain that is refractory to physical therapy and predates the loss of motion.
Patients with secondary adhesive capsulitis often have a history of trauma, surgery, or medical comorbidities.
A history of fracture or extended immobilization should be elicited.
Previous surgeries including rotator cuff repair, capsular shift, Putti-Platt, Bristow-Latarjet, open glenoid bone grafting, and open reduction and internal fixation of a fracture should be documented as a potential cause of stiffness.
Comorbidities, including diabetes mellitus and thyroid disorders, should be recorded because they are associated with adhesive capsulitis.
Symptoms expressed by patients with shoulder stiffness include the following:
Loss of range of motion that translates into functional limitations
Painful arc of motion
Pain often radiating to the deltoid area due to “non-outlet” impingement6
Periscapular pain as a result of transferred pain to the scapulothoracic articulation because of restricted glenohumeral range of motion
Acromioclavicular joint pain due to increased scapulothoracic motion
A comprehensive examination of the involved shoulder must be done to note any concomitant pathology. Physical examination methods include the following:
Passive range-of-motion examinations: Results are compared to the contralateral shoulder. Loss of passive range of motion should always be compared to loss of active range of motion.
Assessing the anterosuperior capsule: A loss of passive external rotation in adduction suggests contracture of the anterosuperior capsule in the region of the rotator interval.
Assessing the anteroinferior capsule: A loss of passive external rotation in abduction suggests contracture of the anteroinferior capsule.
Assessing the inferior capsule: A loss of passive flexion and abduction suggests contracture of the inferior capsule.
Assessing the posterior capsule: Cross-chest adduction can be measured in degrees by recording the angle between an imaginary horizontal to the ground and the axis of the arm. A loss of passive internal rotation suggests contracture of the posterior capsule.
The shoulder should be examined for signs of previous surgery, trauma, deformity, and atrophy.
Manual motor testing of rotator cuff and deltoid muscles should be done.
Active and passive range of motion should be noted in all planes both in seated and supine positions. Shoulder motion should be viewed from the front and back of the patient.
Assessing range of motion in a supine position controls compensatory scapulothoracic motion and lumbar tilt, yielding a more accurate examination.
An equal loss of passive and active range of motion suggests adhesive capsulitis as the cause.
Greater loss of active than passive range of motion suggests rotator cuff or nerve injury.
Global loss of passive range of motion is typical of adhesive capsulitis, whereas loss of range of motion in one plane is usually attributable to postsurgical scarring or trauma.
Lidocaine intra-articular injection test: Passive and active range of motion in all planes should be recorded before glenohumeral injection. Passive and active range of motion should be evaluated after the injection to note any improvement after pain relief. A more accurate assessment of range of motion can be made after pain is alleviated. The recorded increase in range of motion after the injection indicates the extent to which loss of motion is attributable to adhesions and soft tissue contracture as opposed to pain from non-outlet impingement or a symptomatic acromioclavicular joint. The injection can also be therapeutic in the early stages of adhesive capsulitis when synovitis is present. An intra-articular injection may also be coupled with a subacromial injection.11
IMAGING AND OTHER DIAGNOSTIC STUDIES
Routine radiographic evaluation should include an anteroposterior (AP) view of the shoulder in neutral, internal, and external rotation as well as scapular Y and axillary lateral views.
Disuse osteopenia is often noted.
Concomitant findings may include calcific tendinitis or hardware signifying a previous surgical procedure (eg, open reduction and internal fixation, Putti-Platt) (FIG 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree