Anterior/Posterior Cervical Instrumentation
Amir H. Fayyazi
Howard S. An
INTRODUCTION
There have been enormous advances in techniques and instrumentation available for fixation of the cervical spine since Hadra first internally fixed an unstable cervical spine in 1891 (1). During this time, there has been a gradual progression toward the use of rigid internal fixation for fusion and stabilization, culminating in the development of multiple instrumentation systems and techniques currently used in the cervical spine. The benefit of rigid internal fixation initially popularized by the Arbeitsgemeinschaft fur Osteosynthesefragen (AO) Group in the appendicular skeleton also applies to the axial skeleton. This includes reduction, maintenance of alignment, early mobilization, and enhanced fusion rates. Although anterior fusion can be accomplished without internal fixation, in most cases, it necessitates the use of postoperative immobilization for varying intervals depending on the pathology of the lesion.
The benefits of internal fixation are well known; it must not be seen as a substitute for fusion but rather as an adjuvant for stabilization. The method chosen should be based upon the pathoanatomy of the lesion, mechanism of injury, and the surgeon’s own experience with the technique. A thorough knowledge of the relevant surgical anatomy and precise adherence to the described technique should lead to successful stabilization of the cervical segment with a minimal risk of complications. Despite this, even in the hand of an experienced surgeon, instrumentation in the cervical spine is associated with multiple complications. An understanding of these complications and steps necessary to prevent and to manage these issues is essential. In this chapter, we will review the various methods of internal fixation used in the cervical spine, describing the indications, surgical techniques, and potential complications.
ANTERIOR CERVICAL INSTRUMENTATION
The odontoid screw fixation and anterior cervical plate fixation in the subaxial spine are some of the most common procedures performed, and there are numerous clinical and biomechanical studies that have accessed the stability and efficacy of these implants (2,3,4,5,6,7). Other less common techniques include anterior C1-C2 arthrodesis with either plating, intra-articular, or lateral mass screws (8,9,10,11,12).
Anterior Odontoid Screw Fixation
Indications
Conventional treatment of odontoid fractures has included traction, Minerva casts, halo-vest orthosis, braces, and operative fixation. Nonunion rates vary from 0% to 64% depending on the series, with an accepted value of 33% for type II odontoid fractures. Nondisplaced type II fractures or fractures displaced less than 5 mm can be treated successfully with traction and application of halo orthosis. For fractures with displacements larger than 5 mm, age greater than 60 years, and previous loss of reduction, strong consideration should be made for operative fixation.
The advantages of anterior screw fixation over conventional posterior C1-C2 fusion are immediate rigid fixation, preservation of the axial rotation at the C1-C2 facet articulation, minimal postoperative bracing, and the avoidance of the complications associated with bone grafting. This operative approach has gradually gained acceptance in the United States as the preferred technique in the management
of odontoid fractures (2). Its proponents feel that operative morbidity is lessened by an anterior cervical approach, and blood loss is minimal. Fracture patterns indicated for treatment with this method include Anderson-Alonzo type II, type III with a shallow base, and combined C1-C2 injuries. There are two specific situations where anterior dens screw fixation was contraindicated (2): (a) rupture of the transverse ligament of C1 with concomitant C1 ring fracture with coronal separation of greater than 7 mm, and (b) odontoid fractures (type II and III) with an oblique sagittal projection into the C2 vertebral body paralleling the screw preventing interfragmentary compression with this technique (2).
of odontoid fractures (2). Its proponents feel that operative morbidity is lessened by an anterior cervical approach, and blood loss is minimal. Fracture patterns indicated for treatment with this method include Anderson-Alonzo type II, type III with a shallow base, and combined C1-C2 injuries. There are two specific situations where anterior dens screw fixation was contraindicated (2): (a) rupture of the transverse ligament of C1 with concomitant C1 ring fracture with coronal separation of greater than 7 mm, and (b) odontoid fractures (type II and III) with an oblique sagittal projection into the C2 vertebral body paralleling the screw preventing interfragmentary compression with this technique (2).
Technique
Patients are initially placed in the supine position on a radiolucent operative table. Awake nasotracheal intubation is preferred in order to prevent further neurologic injury. Under local anesthesia, the Mayfield headset is then applied and connected to the operating table by means of a crossbar that allows for intraoperative imaging in two planes. If reduction is necessary, maneuvers are performed while the patient is awake, and the neurological exam is rechecked prior to the induction of anesthesia. It is important that anatomic reduction be obtained prior to the beginning of the procedure; after induction, positional changes are potentially dangerous and, if possible, should be avoided. Some degree of extension is necessary during the positioning to allow for adequate surgical exposure. Biplanar fluoroscopy with good resolution of the images is essential for correct screw placement. A plastic bite block may be utilized for the intraoperative AP dens view. If an AP dens view is unobtainable, then a submental radiographic view can be utilized.
The steep approach angle for odontoid screw placement necessitates initial skin incision at the C5-C6 disc space level. The standard anteromedial approach to the cervical spine is then utilized with the transverse incision extending from midline to the anterior border of the sternocleidomastoid. The platysma is then split in a linear fashion and the carotid sheath identified. The retropharyngeal space is entered by scissor dissection just medial to the palpable carotid pulse. Blunt dissection with a peanut or the surgeon’s finger clears the prevertebral fascia and extends cephalad to the anterior tubercle of the atlas. An incision is then made through the anterior longitudinal ligament at the inferior portion of C2. The technique varies as to whether the one- or two-screw technique is utilized. Graziano et al. found that there was no statistical difference between the one- and two-screw techniques in both torsion and bending stiffness (7). They felt that the use of one screw for odontoid fixation would lessen the chances for malposition. If the two-screw method is chosen, then preoperative CT scanning may be helpful in determining the dimensions of the dens.
For single-screw fixation, a 2-mm K-wire is inserted midline at the anterior inferior border of C2. It is then advanced under fluoroscopic control, with confirmation of direction in both the AP and lateral planes through the body of C2 into the odontoid. A second wire can be utilized for rotational stability while tapping and screw placement is in progress. A 3.5- or 4-mm screw can then be placed under constant fluoroscopic visualization. Another option is to use a cannulated screw system were the screw can be advanced over the guide wire. The tip of the screw should come to rest in the apical portion of the dens for optimum fixation. Biplanar permanent radiographs should be taken for final confirmation of screw placement. Postoperative immobilization varies according to the surgeon’s preference and the degree of expected patient compliance for 6 to 12 weeks. The two-screw technique starts 2 to 3 mm lateral to the midline and proceeds in a similar fashion. The use of two screws for insertional stability is recommended for oblique fracture patterns. Ideal mechanical stability would be achieved with short threaded screws or by overdrilling the near cortex for lag screw compression.
For treatment of odontoid nonunion, Montesano et al. advocates the use of a special anteriorly angled curette for debridement of the fibrous tissue at the nonunion site, followed by addition of a small amount of cancellous bone graft obtained from the body of C3 (13). This technique is not universally accepted. Other authors consider nonunion a relative contraindication to the use of this technique.
Complications
Anterior odontoid screw fixation has been quite successful in treatment of type II or type III dens fractures with no complication rate and a high rate of fusion at multiple centers (14,15,16,17). On the other hand, Aebi et al. have noted a major complication rate of 20% with this procedure; the complication rate is similar to posterior wiring for treatment of odontoid fractures (2). Both Bohler et al. and Aebi et al. consider anterior odontoid screw fixation the procedure of choice for management of acute fractures of the odontoid (2,4).
By far the most common complication associated with this technique is pseudarthrosis, which has been reported to be as high as 27% (18). Other noteworthy papers have reported a lower but significant rate of pseudarthrosis. Blauth et al. have noted pseudarthrosis in 8 of 71 patients (11%) treated with anterior fixation (19). Suchomel et al. have noted a 90.5% fusion rate in 21 patients at 6 months (20). Finally, Henry et al. have noted a 92% union rate in 61 patients at an average of 14.1 weeks (21).
Other common complications associated with this instrumentation
technique include initial malpositioned screws (Fig. 8.1), insufficient reduction and failure of fixation (Fig. 8.2), screw migration (Fig. 8.3), and limited, painful range of motion following fusion. Despite the fact that this technique has been in use for close to two decades, it is very difficult to clarify the rate of these complications from published data. The rates of malpositioned screws have been reported to be as high as 4% (19) to 44% (22). Insufficient reduction has been noted to be from 1.5% (19) to 41% (23). Additionally, there appears to be a trend toward loss of reduction if the fracture is not adequately reduced prior to fixation (23). Failure of fixation has been noted to be 3% by Henry et al. (21), 6% by Grosse et al. (24), and 41% by Chang et al. (23). Others have reported failure of screw fixation due to screw migration in 9% of 32 patients (22). Finally, despite union of dens fracture, 10% (21) to 22% (24) will have persistent pain or limited range of motion after anterior odontoid fixation.
technique include initial malpositioned screws (Fig. 8.1), insufficient reduction and failure of fixation (Fig. 8.2), screw migration (Fig. 8.3), and limited, painful range of motion following fusion. Despite the fact that this technique has been in use for close to two decades, it is very difficult to clarify the rate of these complications from published data. The rates of malpositioned screws have been reported to be as high as 4% (19) to 44% (22). Insufficient reduction has been noted to be from 1.5% (19) to 41% (23). Additionally, there appears to be a trend toward loss of reduction if the fracture is not adequately reduced prior to fixation (23). Failure of fixation has been noted to be 3% by Henry et al. (21), 6% by Grosse et al. (24), and 41% by Chang et al. (23). Others have reported failure of screw fixation due to screw migration in 9% of 32 patients (22). Finally, despite union of dens fracture, 10% (21) to 22% (24) will have persistent pain or limited range of motion after anterior odontoid fixation.
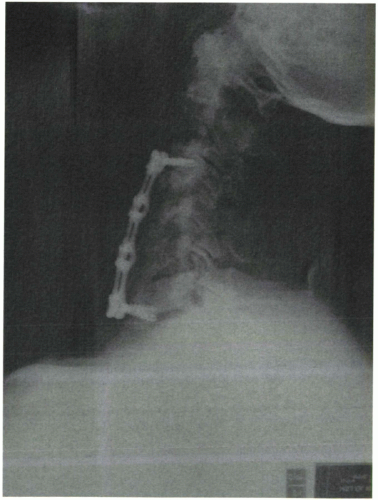
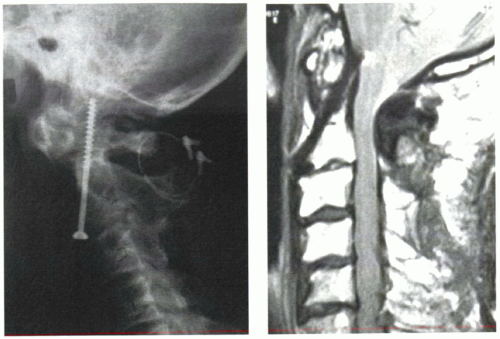 Figure 8.1 Lateral x-ray and sagittal MRI demonstrating a misplaced anterior odontoid screw with impingement of the brain stem. |
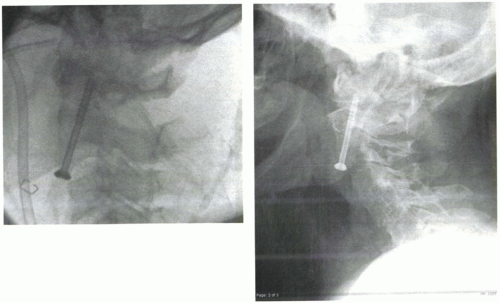 Figure 8.2 Intraoperative fluoroscopy and postoperative lateral x-ray demonstrating displacement of fracture after anterior odontoid screw fixation. |
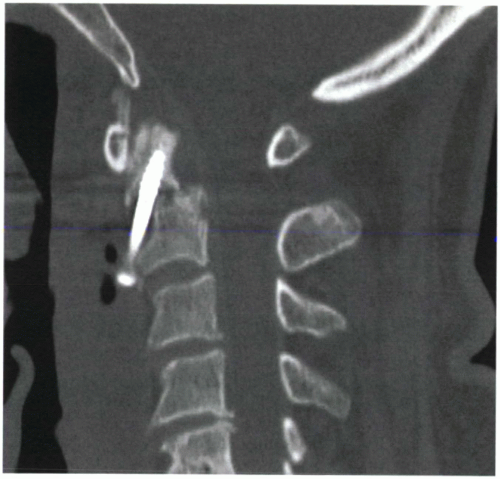 Figure 8.3 Lateral x-ray and CT reconstruction views demonstrating an anterior odontoid screw cut-out. |
The rare complications associated with odontoid screw fixation include carotid artery rupture and esophageal perforation (22). Other potential structures at risk include the vertebral artery and the spinal cord with grossly malpositioned screws.
How to Prevent and Manage Complications
To prevent complication with anterior odontoid screw fixation, one must have a clear understanding of the fracture line and comminution. The anterior odontoid screw is only effective in treatment of fracture lines that are perpendicular to the direction of the screw. The use of this technique in comminuted fractures and fracture lines from posteriosuperior to anterioinferior is fraught with complication and should be avoided at all times. In these situations, a posterior approach should be utilized for stabilization of upper cervical spine. Although lateral C-spine radiographs are quite sensitive in demonstrating the displaced odontoid fractures, the morphology of the fracture line in the majority of cases cannot be adequately evaluated on routine radiographs and should be evaluated preoperatively using computed tomography with sagittal reconstructions.
This procedure is technically demanding and requires the use of biplanar, high-resolution fluoroscopy for accurate screw placement; radiographic visualization is absolutely essential and at times can be very difficult, especially in older patients with osteoporosis and spondylosis. We prefer to use two c-arms for orthogonal views of the odontoid process. The lateral c-arm should be centered at the C2 and view magnified in order to visualize the odontoid process to prevent posterior misplacement. The second c-arm can be positioned for an anterioposterior view of the odontoid process. We routinely use a submental view of the odontoid instead of an open-mouth odontoid view that is very difficult to obtain intraoperatively despite the use of a plastic bite block.
Finally, one should never attempt this technique if the odontoid fracture cannot be reduced on the operating table. Depending on the surgeon’s preference, Gardner-Wells tongs, Mayfield tongs, or a halo ring attachment can be used for both reduction and maintenance of the head during the procedure. We prefer to use a Mayfield tong or a halo ring device attached to the table through the Mayfield arm; this setup offers better stability and does not require traction for maintenance of reduction.
In cases of pseudarthrosis or in patients with persistent, painful range of motion following successful anterior fixation, posterior stabilization and fusion is recommended. When a malpositioned odontoid screw is noted, a revision procedure may be indicated. This can be accomplished either by revision of the anterior screw (25) or by removal of the screw followed by posterior spinal fusion and instrumentation. In the majority of cases with displacement of the fracture, screw migration, or screw cut-out, a posterior fusion and instrumentation is necessary. The indication for removal of the odontoid screw in this situation is potential injury to the soft tissue or neural elements.
Anterior odontoid screw fixation is contraindicated in cases with concomitant C1-C2 instability and should never be attempted. This instability may be difficult to assess prior to surgery and may be noted postoperatively. Once C1-C2 instability is noted, a posterior stabilizing procedure is required.
Anterior C1-C2 Intra-articular Screw Fixation
Indication
The indication for the use of anterior C1-C2 lateral mass screw fixation cannot be adequately stated at this time due to a lack of adequate published reports. Despite this, its use has been reported in highly selected cases with posterior C1-C2 nonunion (11,12). In these two case reports, good results have been noted in early follow-up. In another case report by Reindl et al., this technique was used in conjunction with anterior odontoid screw with good results (10).
Technique
Complication
At this time, there is not enough information on complication rates with this procedure. Potential complications associated with the instrumentation include inadequate stabilization due to malpositioned screw, screw migration, injury to the vertebral artery, potential breach into the occipitocervical joint, and potential placement of the screw into the spinal canal.
How to Prevent and Manage Complications
Prior to attempting this procedure, a thorough understanding of upper cervical anatomy is essential. It is also essential to radiographically visualize the bony structures prior to screw placement.
Anterior C1-C2 Lateral Mass Plates
Indication
Anterior C1-C2 plating through a transoral approach has been reported by Louis (8). This technique is only indicated in selective cases and only when other methods of fixation cannot be used.
Complication
The major complications noted by the author include infection in two cases treated with plate removal. Screw loosening occurred in three cases, which resulted in the passage of the screw through the digestive tract without complication (8).
How to Prevent and Manage Complications
Prior to attempting this procedure, a thorough understanding of upper cervical anatomy is essential. It is also essential to radiographically visualize the bony structures prior to screw placement.
Anterior Cervical Plates (Subaxial)
Indication
Anterior cervical discectomy and fusion is seen as the standard for treatment of degenerative conditions in the cervical spine. Fusion methods popularized by Bailey and Badgely, Cloward, and Smith-Robinson are widely accepted for the treatment of cervical spondylosis (26,27,28). These methods rely on the inherent stability of the bone graft in the interspace and are quite effective in degenerative situations. However, in the presence of instability, the bone graft alone cannot be the sole method of fixation. This instability can be either due to traumatic or pathologic causes or can be iatrogenic following multiple-level corpectomy.
Additional methods of stabilization are necessary for safe and effective treatment of unstable cervical spine segment. Treatment with prolonged halo-vest immobilization or cranial tong traction may not effectively treat the lesion and are fraught with their own sets of complications. Early mobilization of the patient has been recognized as an important factor in the treatment of acute spinal cord injury patients. Anterior stabilization and decompression can be performed alone or followed by staged posterior procedures when indicated by the pathology of the lesion.
The precise indications for the use of anterior instrumentation in the treatment of cervical spondylosis have yet to be defined. Many surgeons feel that it is too costly and unnecessary for routine use in single-level degenerative conditions. Current recommendations include reconstruction after vertebrectomy for tumor, multilevel spondylosis, fracture or soft tissue instability, or infection that has failed conservative treatment. Anterior plate stabilization is an important tool when intraoperative stability of a strut graft is questionable or the patient will not tolerate a halo-vest orthosis.
In traumatic injuries that predominantly involve the anterior vertebral body or the disc and require surgical stabilization, a standalone anterior plate may be sufficient and can potentially decrease the complication rate associated with posterior instrumentation. The use of anterior surgery in the treatment of posterior instability is not an established indication. It can, however, be used in selected patients with good bone quality or as a part of circumferential fusions. Koh et al. have demonstrated that, biomechanically, anterior plating may be effective in treatment of cervical burst fracture; however, these devices are not as stable as posterior plating for treatment of flexion-distraction injury (29).
Biomechanics of Anterior Cervical Plating
A number of different plate designs are currently available or have been used in the past. Initially, the plates had an unconstrained design and were associated with a high rate of screw loosening and dislodgement. To prevent this complication, newer plates employed a constrained type of the design, where there is no motion between the plate and the screw. Despite lack of clinical evidence, a number of complications have been blamed on this constrained (“rigid”) design. These include a high pseudarthrosis rate, presumably due to the load-bearing feature of the plate and prevention of subsidence due to the static position of the screws. The optimal amount of load that needs to be placed on the graft and the end plate in a clinical setting is not known. Furthermore, locked anterior cervical plates have
also been noted to subside 1 to 1.5 mm per segment soon following the procedure.
also been noted to subside 1 to 1.5 mm per segment soon following the procedure.
To increase the load seen by the graft and in order to allow subsidence, newer plate designs (“dynamic plates”) allow some motion at the screw-plate interface (30). It is thought that by allowing the graft to subside, a higher fusion rate is obtained. However, these designs carry their own design flaws. These devices allow load-sharing by the graft at the expense of construct stability (31,32). Additionally, as the graft subsides, these plates impinge on the adjacent level discs, resulting in early arthrosis. Furthermore, there is no conclusive evidence that the rate of construct failure in a long cervical construct is any lower with the semiconstrained devices versus the older constrained plates (33). Despite the lack of clinical evidence, the dynamic plates have recently become quite popular. One of the reasons for this popularity is the ease of use—the screws can be placed in multiple angles, which was not available in the older rigid designs. This difficultly with initial rigid screw systems has been overcome by recent developments that allow variable angular position of the screws in rigid cervical plates (34).
Technique
For safe and effective surgical approach, proper preoperative positioning is imperative. For most cases, Gardner-Wells tong traction is sufficient to provide intraoperative stability. A small towel-roll is placed between the shoulders, and the arms are secured at the sides with foam protective devices and an overlapping towel. Longitudinal traction with cloth tape applied at the shoulders may be beneficial. The iliac crest is also elevated with the use of a rolled towel or large IV bag.
Standard anteromedial Smith-Robinson approach can be made for one- or two-level fusions (28). It is extremely important to dissect the fascial planes fully for adequate exposure. Occasionally, a longitudinal incision along the anterior border of the sternocleidomastoid may be required for longer constructs. Blunt dissection with a peanut or the finger clears the prevertebral fascia and allows the subperiosteal mobilization of the longus coli muscles. Blunt selfretractor blades are then positioned beneath the reflected longus coli muscles to protect the esophagus and carotid sheath from injury. Identification of the involved level(s) is usually confirmed by a portable lateral cervical spine film. Decompression or vertebrectomy is then performed according to the character of the lesion. Meticulous preparation of the graft may obviate the need for supplemental anterior fixation. Anterior plating may avoid the complications of anterior graft without fixation or staged posterior arthrodesis in cases of vertebral body fracture. If intraoperative stability cannot be achieved with extensive reconstructive grafting for multilevel degenerative or widespread tumor destruction, then plate fixation can be an important adjuvant to stabilization techniques with immediate rigid fixation.
Placement and selection of the size of the plate depend on the instrumentation system chosen for implantation. The authors favor a system with a convergent screw design for additional safety rather than a divergent design. The plate is then positioned just above the graft-vertebral body interface, and this also allows for cephalad and caudal screw placement. This reduces the potential for injury to adjacent, healthy cervical disc spaces. The plate is then contoured to fit the anterior surface in order to maximize bony contact. The plate may have a prebent, gentle lordotic curve that can be modified to fit the construct with plate benders, but one has to be aware that excessive bending will also change the orientation of the screws at either end. Also, correct positioning of the plate in the midline must be done to reduce the incidence of iatrogenic injury and to provide maximum bone surface for fixation. Contouring of the surface of the plate-bone interface is then performed with a rongeur or high-speed burr to increase the stability of the construct. The local anatomy is then reviewed prior to fixation to ensure the plate is correctly centered. The uncinate processes can be used as a marker on either side for reference.
The drill guide is then inserted into the plate and drilled with appropriate degrees of convergence and cranial/caudal orientation. Preoperative radiographs or CT scans are utilized to estimate the width of the vertebral body. Depending on the systems used, either unicortical or bicortical fixation can be used. Fluoroscopy can also be utilized for additional verification of these steps. It is important that intraoperative traction be reduced to 5 lbs prior to screw placement. Proximal and distal screws are then placed diagonally opposite for initial stability and partially tightened; the remaining screws are then placed and secured. An intraoperative radiograph is then taken for final verification of screw depth and orientation of the plate. The center screw can be utilized with long strut graft reconstructions for added stability. The screws are then locked in place in accordance to the instrumentation used to prevent the screws backing out. Revision with cancellous screws of greater diameter can be used if the initial screws do not achieve good fixation. Care is taken to inspect the esophagus prior to closure for any evidence of a tear in the muscular wall.
Complication
The anterior approach to cervical spondylosis involves dissection and retraction of numerous vital vascular, neural, and visceral structures (35,36). An overall 0.2% incidence of complications based upon an extensive review of published series has been reported (36,37). Soft tissue injury rate is to some extent dependent on the duration of procedure, which is much longer in instrumented cases. The incidence of vocal cord paralysis from recurrent laryngeal nerve injury ranges from 1% to 11% (38). The possible etiologies
are traumatic division, neuropraxia, compression from postoperative edema, and injury from thermal necrosis. Recurrent laryngeal nerve injury is manifested as hoarseness and an increased risk of aspiration due to the inability to completely close the larynx (37,39). Sympathetic chain injury is also uncommon and manifests as ipsilateral miosis, ptosis, and anhidrosis. Treatment options are limited. Midline soft tissue injury to the trachea, esophagus, and pharynx are uncommon.
are traumatic division, neuropraxia, compression from postoperative edema, and injury from thermal necrosis. Recurrent laryngeal nerve injury is manifested as hoarseness and an increased risk of aspiration due to the inability to completely close the larynx (37,39). Sympathetic chain injury is also uncommon and manifests as ipsilateral miosis, ptosis, and anhidrosis. Treatment options are limited. Midline soft tissue injury to the trachea, esophagus, and pharynx are uncommon.
Dysphagia following anterior cervical surgery is common but temporary and is estimated to occur transiently in 8% of patients (37). When persistent symptoms develop, evaluation should include a lateral radiograph to check bone graft and plate position (40). Esophageal lacerations occur in approximately 0.25% to 0.7% of patients (37). When identified, immediate primary repair should be performed, the wound appropriately drained, and the patient started on broad-spectrum antibiotics.
Vascular injuries during the surgical approach or decompression are rare but can have devastating sequelae (35). The carotid sheath contents, superior and inferior thyroid arteries, and the vertebral artery are all at risk. Avoidance of overzealous retraction and the use of blunt-edged retractors diminish the risk of injuries to these vessels. Knowledge of the vertebral artery anatomy and its relationship to the lateral disc space and vertebral body, as well as maintaining midline orientation during decompression, all serve to minimize the risk of injury estimated to occur in 0.3% to 0.5% of cases. This risk may be slightly elevated in instrumented cases, mainly due to the additional steps required in anterior vertebral body preparation, plate placement, drilling, and screw placement.
Spinal cord injury is perhaps the most devastating complication that occurs in anterior cervical surgery and occurs with an incidence of 0.1% to 0.64% (41). Neck manipulation during intubation, cervical malalignment following decompression and grafting, and postoperative epidural hematoma must all be considered in the evaluation of the patient with postoperative neurologic deterioration. Management should include maintenance of normotensive blood pressure, administration of steroids, and imaging studies to assess for possible graft dislodgment. Hardwarerelated spinal cord injury, either during drilling or screw placement, is extremely rare and can be completely prevented by close adherence to the surgical technique.
Pseudarthrosis rates following anterior grafting procedures range from 0% to 26% (42,43,44,45,46,47). Estimates of fusion for single-, two-, and three-level anterior cervical discectomy and fusion (ACDF) are 88% to 90%, 73% to 80%, and 70%, respectively (46,47). It should be noted that the lack of bony union does not imply clinical symptomatology (48,49). Furthermore, the literature is varied in terms of radiographic criteria for the description of osseous unions after interbody fusions (41).
Finally, hardware failure can be a common problem, especially in multilevel corpectomy cases. The rate of screw loosening is much higher in cases with nonconstraint screw-plate interface. This rate was noted to 5% in Herman and Sonntag’s data (50). In Lowery and McDonough’s report, the rate of screw loosening was 39% in nonconstraint plates and 18% in constraint plates (51). Although common, screw loosening may not be associated with unfavorable clinical outcome. A more serious complication is hardware kick-out and graft dislodgement (Fig. 8.4). Although graft dislodgement is quite unlikely in single-level ACDF procedures, as the length of the graft increases, the stability of the construct decreases and this complication presents. In the Macdonald et al. series, the incidence of graft dislodgement was 8% (52). In Sasso et al. data, the rate of plate failure after two-level corpectomy was 6% and after three-level corpectomy was 71% (53). Similar result was reported by Vaccaro et al., who noted a 9% failure rate in two-level corpectomy cases and a 50% failure rate in three-level corpectomy cases (54).
How to Prevent and Manage Complications
Complications associated with anterior cervical plating can be divided into either soft tissue- or plate-related. Soft tissue complications such as esophageal laceration, carotid or vertebral artery injury, and tracheal injury are to a certain extent
preventable with adherence to surgical technique. On the other hand, vocal cord paralysis and postoperative dysphagia cannot be fully prevented. The recurrent laryngeal nerve can be protected, although not in all cases if dissection is not extended to the interval between the esophagus and the trachea. Some authors also believe that a lefthanded approach to the lower cervical levels decreases the rate of laryngeal nerve injury, given the more predictable location of this nerve on the left when compared to the right side. On the other hand, postoperative dysphagia may be related to the duration of esophageal retraction; this complication may be decreased by replacing the retractor blade every few minutes and decreasing the local esophageal ischemia.
preventable with adherence to surgical technique. On the other hand, vocal cord paralysis and postoperative dysphagia cannot be fully prevented. The recurrent laryngeal nerve can be protected, although not in all cases if dissection is not extended to the interval between the esophagus and the trachea. Some authors also believe that a lefthanded approach to the lower cervical levels decreases the rate of laryngeal nerve injury, given the more predictable location of this nerve on the left when compared to the right side. On the other hand, postoperative dysphagia may be related to the duration of esophageal retraction; this complication may be decreased by replacing the retractor blade every few minutes and decreasing the local esophageal ischemia.
Plate complication is either due to screw loosening, plate fracture, or plate-graft dislodgement. Of these, graft dislodgement is by far the most serious and can result in catastrophic complications such as airway obstruction and death. As stated before, the rate of plate failure with three-level corpectomy is quite high, and this procedure should be avoided if at all possible (53,54). In these situations, posterior instrumentation alone is quite stable and an anterior plate does not add much to the stability of the construct (55). An alternative technique is the use of a hybrid construct made of a two-level corpectomy and a lower-level discectomy; this has been shown to be biomechanically stronger than a three-level corpectomy construct (56).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree