Anterior Cervical Corpectomy and Fusion
Andrew H. Milby
John M. Rhee
John G. Heller
Illustrative Case
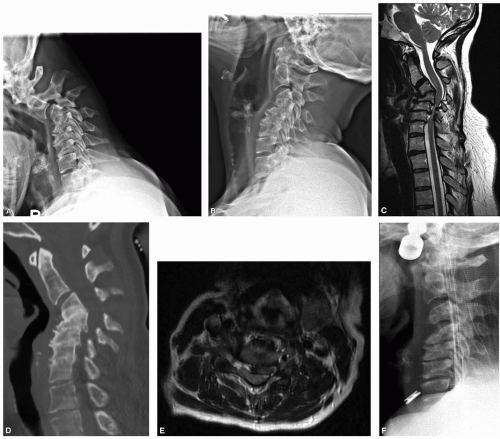
A 43-year-old woman with cervical myelopathy and deformity. There is retrovertebral cord compression behind C4, and disk-based spinal cord and root compression at C5-6 and C6-7, associated with significant cervical kyphosis. The patient was placed in preoperative cervical traction to improve alignment (Figure 2-1).
Indications
The primary indication for cervical corpectomy is retrovertebral cord compression requiring vertebral body resection for adequate anterior decompression of the cord.
Other less common indications include the need to remove vertebral body lesions (eg, tumors or osteomyelitis).
If retrovertebral compression does not exist and an anterior approach is selected, we generally favor anterior cervical diskectomy and fusion (ACDF) because it allows for segmental screw fixation at every level, better restores lordosis, is biomechanically more stable, and is less likely to kick-out or settle, especially in osteoporotic bone.
Depending on bone quality, alignment, and other circumstances, if greater than a one-level corpectomy is needed, we strongly consider supplemental posterior fixation to prevent construct settling or failure.
Other options for addressing retrovertebral cord compression include a posterior or combined anterior-posterior approach.
Radiologic Assessment
Determine the extent of partial versus complete corpectomies needed at each level based on need for retrovertebral access.
When possible, we perform diskectomies at levels that require disk-based decompression and do not demonstrate retrovertebral cord compression.
For example, a corpectomy at one level combined with diskectomy(ies) at other level(s)
Be aware of the locations of vertebral arteries (both medial-lateral and ventral-dorsal) and side dominance. Anomalies of the artery entering the vertebral body requiring resection may be a contraindication to corpectomy at that level or may require hemicorpectomy instead.
This is best evaluated on axial CT scan, but may also be seen on axial MRI.
In general, we have a low threshold for obtaining preoperative CT scans in corpectomy patients (Figure 2-2).
Estimate potential screw lengths at planned instrumentation levels.
Determine the need for foraminal decompression at various levels.
Determine whether areas of deformity are fixed or flexible (eg, if fusion exists across disk spaces and/or facets). For flexible deformities, consider use of preoperative traction for gradual deformity correction. Our case appeared stiff, but clearly demonstrated mobility with traction.
Special Equipment
Diamond-tipped or side-cutting burr, lumbar drain availability in cases of ossification of the posterior longitudinal ligament (PLL)
Gardner-Wells traction intraoperatively in cases of significant deformity or if unable to obtain segmental distraction across the corpectomy with Caspar pin distractor
Caspar pins generally allow for distraction across one and sometimes two corpectomy levels depending on the size of the vertebrae.
Fibular strut allografts and/or cages as indicated for corpectomy reconstruction
Sagittal saw as needed for autograft harvest and/or allograft sizing
Positioning
Refer to chapter on ACDF.
If harvesting iliac crest, then use ipsilateral side (prep out for graft harvest the same side as exposure if taking graft).
Place folded sheet bump under ipsilateral hip if iliac crest bone graft (ICBG) harvest
Perform corpectomy and measure defect before proceeding with ICBG harvest
Anesthesia/Neuromonitoring
Nasotracheal intubation may facilitate access to C3 and above (allows dental apposition).
Look at the lateral x-ray preoperatively to determine whether this may be necessary—in most cases, it is not.
Mean arterial pressure goal >80 mm Hg in the setting of myelopathy.
Refer to the Neuromonitoring chapter for recommendations regarding use of neuromonitoring.
Localization
Refer to ACDF chapter.
Approach
Refer to ACDF chapter.
Consider use of oblique longitudinal incision to allow for extensile exposure.
This may be helpful in more than four-level surgery, those with significant hyperlordosis (to be able to reach the top and bottom of the construct with the appropriate line of sight), or those with very thick necks.
In the majority of three- to four-level cases, however, a transverse incision centered at the sagittal midpoint of the operative levels will allow adequate access, especially when combined with generous mobilization of tissues.
Retractor Placement
Refer to ACDF Chapter.
Especially when performing multilevel anterior surgery, spend time during exposure to adequately relax the incision and mobilize the multiple fascial planes to avoid forceful retraction on the soft-tissue structures of the neck.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree