Ankle Injuries
Acute Injuries
13.1 Lateral Ankle Sprain
Clin Sports Med 1997;16:433; Phy Sportsmed 1993;21:123; Phy Sportsmed 1998; 26:29; Med Sci Sports Exerc 1999;31:S429
Cause: Excessive, rapid ankle inversion; the majority of ankle sprains involve the anterior talofibular ligament.
Epidem: Most common injury in athletics; 85% of all ankle injuries are sprains, more than 4 × as frequent than medial ankle sprains; 85% are lateral and 85% involve the ATFL.
Pathophys: Inversion or an internal rotation force to a plantar-flexed ankle, which may result in partial or complete disruption of the lateral ligamentous complex; (anterior talofibular [ATFL], calcaneofibular [CFL], and, much less commonly, the posterior talofibular ligaments [PTFL]).
Sx: The pt may appreciate a “tear” or “pop” at the time of injury, which may indicate a complete tear; the pain is intense and localized to the lateral ankle, often anterior or inferior to the lateral malleolus; the pain may initially improve in the first few hours, only to return with the presence of increased swelling; normal ROM is dorsiflexion (DF) 15-20°, plantar flexion (PF) 50°, eversion (Ev), inversion (Inv).
Si:
May have antalgic gait or other gait abnormalities.
Ecchymosis over lateral ankle.
Decreased active ROM.
Access sensation in the distribution of the deep peroneal nerve (first webbed space of the foot).
Access motor function and presence of dorsalis pedis and posterior tibial pulses.
Tibiofibular squeeze test to assess for syndesmotic injury (see 14.4).
May have pos Talar tilt test:
Performed with the pt seated and with the ankle in 10° of plantar flexion.
Stabilize the medial aspect of the distal part of the leg, just proximal to the medial malleolus, with one hand and apply an inversion force slowly to the hindfoot with the other hand; the affected side is compared against the normal side; if the talus gaps and rocks open this indicates laxity of the ATFL.
May have pos anterior drawer test:
Performed with the foot in 10° of plantar flexion: tests for anterolateral rotatory instability due to anterior talofibular ligament instability.
Stabilize the distal part of the leg with one hand and apply an anterior force with the other hand on the heel, and attempt to subluxate the talus anteriorly from beneath the tibia.
The affected ankle is compared to the pt’s normal ankle.
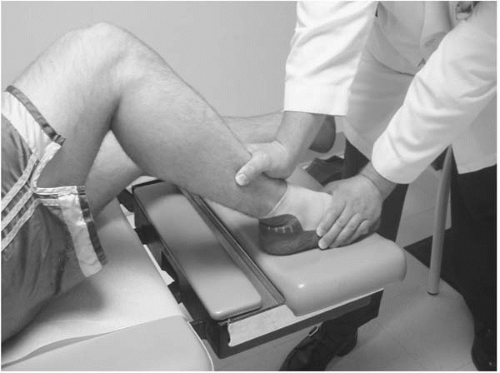
Alternative modified anterior drawer test (Figure 13.1) may be performed by having the pt rest each foot on the examining table with the knees bent at 90°; the examiner then stabilizes the foot on the exam table and provides a posterior
force on the distal tibia and estimating the degree of posterior displacement of the tibia on the talus (anterior drawer).
Talar tilt and anterior drawer tests may be difficult to perform in acute setting.
Grading sprains:
Cmplc: Traction injuries of the peroneal and posterior tibial nerves can occur in severe injuries.
Diff Dx: Peroneal compartment syndrome, chronic syndesmotic injury (see 13.4), peroneal tendon subluxation (see 13.3), talar dome lesion (see 13.5), ankle fracture, Achilles tendon rupture (see 13.6), midfoot injury (see 14.18), lateral process fracture of the talus (prevalent in snowboarders, poorly visible on x-ray, CT if suspect).
X-ray:
To rule out fracture or syndesmotic injury.
Radiographic assessment of the syndesmosis: one of the more challenging and important tasks that the clinician must perform is to rule out an injury to the syndesmosis; the mortise and AP views must be utilized to review the criteria for diagnosing injury to the syndesmosis.
Standard: anteroposterior (AP), lateral, and mortise views.
Consider foot and leg films when clinically indicated.
The radiographs should be evaluated for:
The presence or absence of a medial malleolar fracture or widening of the space between the medial malleolus and the talus (aka medial clear space).
The presence or absence of a fibular fracture, its relationship to the tibial plafond (ie, at, above or below), and the orientation of the fracture (ie, transverse, oblique or comminuted).
Displacement of the distal tibiofibular joint (to assess competency of the syndesmosis; aka tibiofibular overlap).
Displacement of the talus from its normal anatomic position beneath the tibia (aka: talar tilt; not the same as talar tilt test).
Ottawa Rules: a decision protocol designed to avoid obtaining films on all ankle injuries by identifying patients at negligible
risk for fracture; 97%+ sensitivity for ruling out a fracture, but only a 31-63% specificity for ruling in fractures (Jama 1993;269:1127); essentially an ankle x-ray series is necessary only if there is pain near the malleoli and any of these findings:
Inability to bear weight both immediately and in the emergency room (4 steps); or
Bone tenderness at the posterior edge or posterior tip of either malleolus.
Rx: Refer to orthopedic surgeon if tibiofibular overlap is > 10 mm, there is > 2 mm difference between medial and lateral talar tilts, medial clear space is > 2 mm greater than superior, all medial and displaced lateral malleolar fractures, and lateral malleolar fracture > 2 mm displacement; consider referral for Grade III injuries; early protected mobilization and functional rehabilitation for all grades of sprain.
Ankle Rehabilitation:
Phase I: (Immediate postinjury) PRICEMM and early motion:
Use crutches or cane if unable to walk without limp; emphasize normal heel-toe gait with progressive wt-bearing over 1-5 d
Protect from further damage: ankle brace to limit inversion and eversion; Grade II sprains may require a short period of immobilization with a posterior splint or short leg cast; Grade III sprains may require up to 6-8 wks of immobilization.
Relative rest: limit activity; avoid abusing activity.
Compression: wrap ankle with ace wrap or ankle brace to control swelling; horseshoe felt around lateral malleolus may improve effectiveness of compression wraps.
Elevate: keep leg above heart as much as possible to help control swelling.
Medications: large-scale studies have demonstrated that nonsteroidal anti-inflammatory drug (NSAID) used postinjury resulted in reduced subject pain, time lost from training, cost of treatment and increased exercise endurance; however, NSAID use was also associated with increased ligament laxity, decreased range-of-motion, and increased swelling; it is possible that the analgesic effects allow athletes to resume training prematurely (Am J Sports Med 1997;25:544); if NSAIDs are used, consider starting 48 hr postinjury to decrease risk of increased bleeding at injury site; acetaminophen for pain, as needed.
Modalities: physical therapy (electric-stim or ultrasound).
Ice bath followed by stationary bike: immerse foot in ice bucket until foot is numb, and then ride bike until numbness wears off; repeat 4 ×.
ROM exercise: write the capital letters of the alphabet with the big toe by moving at the ankle; only move to the point of stretching.
Phase II: Begin as soon as one can tolerate the listed activity without compensation (see 22.5):
Stationary bike.
Balance and proprioception exercises: BAPS, foam roller balance.
Theraband exercises: loop Theraband or surgical tubing around forefoot, hold proximal ends in hands; invert and evert against resistance.
Heel raises and Achilles stretching: raise up on the balls of both feet, lifting the heels off the door; lower the heels slowly; repeat 30 repetitions; when stronger, raise up on strong foot, lower with only the injured foot.
Contrast bath: 20 min.
Phase III: Begin when able to walk without limp:
Add stairmaster, slide board, squats, and lunges.
Balance and proprioception exercises: stand on effected leg on mini-trampoline; close eyes for 20 sec (go ahead and try it while healthy—it is an ankle workout); repeat 6 ×; stand on affected leg on mini-trampoline, play catch with a 1-2 kg medicine ball (or any ball); a useful alternative to a mini-trampoline is to use a folded towel on a hardwood floor.
Ice ankle after exercise for 20 min.
Phase IV:
Gradual return to jogging.
Jump rope.
Dot jumping, agility drills, balance and proprioception exercises (see above).
Ice, as needed.
Consider ankle brace for return to full activity.
Progression from phase to phase is dependent upon individual progression, NOT time.
Prevention: Most common risk factor for ankle sprain is a history of previous sprain; complete supervised rehabilitation should be completed before return to practice; athletes suffering a moderate or severe sprain should wear an appropriate brace for at least 6 mo; properly fitting braces or correctly applied tape does not interfere with athletic performance; ankle taping provides effective support for less than 20 min of exercise, however it may help provide additional propioception via the skin and reduce injury; lace-up braces and stirrup-style braces offer longer lasting support; ankle strengthening and proprioception training are the most effective form of prevention (Am J Sports Med 1999;277:573).
Return to Activity:
Normal range of motion.
85% of pre-injury strength.
Minimal swelling.
No pain with ADLs.
Pain-free execution of functional drills such as hopping on injured leg or sprinting tight figure-eight pattern.
Good proprioception as demonstrated by ability to single-leg stand with eyes closed for 25-30 sec.
13.2 Medial Ankle Sprain
J Emerg Med 1999;17:651; Clin Sports Med 1997;16:435
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree