Ankle and Lower Leg
Examination of the ankle
Inspection
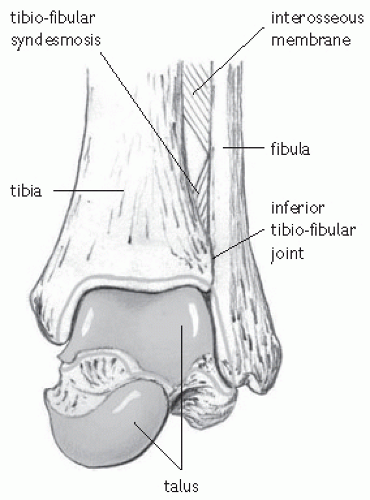
The ankle contains three joints:
Talocrural joint.
Inferior tibiofibular joint.
Subtalar joint.
With the feet in a symmetrical position the subtalar joint is in neutral; neither pronated or supinated. Pronation consists of:
Eversion.
Dorsiflexion.
Abduction of the foot.
Supination consists of:
Inversion.
Plantar flexion.
Adduction of the foot.
Look for evidence of abnormal biomechanics when standing, walking, supine, and prone:
Excessive pronation.
Excessive supination.
Fore foot varus.
Fore foot valgus.
Rear foot varus.
Rear foot valgus.
Ankle equinus.
Genu varum.
Genu valgum.
Leg length.
Palpation
See Fig. 23.1 for the bony anatomy of the ankle.
Lateral structures
Medial structures
Medial ligament.
Tibialis posterior.
Flexor hallucis longus.
Sustentaculum tali.
Navicular tubercle.
Midtarsal joint.
Posterior structures
Achilles tendon.
Retrocalcaneal bursa.
Posterior talus.
Calcaneum.
Active and passive movements
Ankle dorsiflexion (10-20°).
Ankle dorsiflexion can be restricted by inflexibility of gastrocnemius and soleus.
The minimum range of ankle dorsiflexion for normal locomotion is 10°.
Ankle plantar flexion (35-50°).
Dorsiflexion and plantar flexion take place between the talus and tibia and fibula.
Subtalar inversion (10-20°).
Subtalar eversion (5-10°).
Inversion and eversion take place at the talocalcaneal, talonavicular, and calcaneocuboid joints. Perform with ankle dorsiflexed to limit lateral motion.
Inversion is usually double that of eversion.
Resisted movements
Plantarflexion
Gastrocnemius (knee extended).
Soleus (knee flexed).
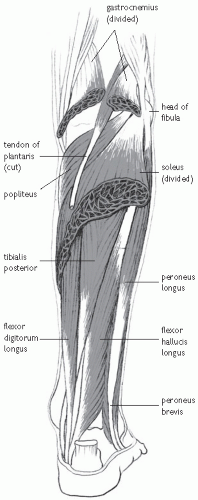
Flexor digitorum longus, flexor hallucis longus (flex the toes against resistance). See Fig. 23.2.
Dorsiflexion
Tibialis anterior (dorsiflex the foot against resistance).
Extensor digitorum longus (dorsiflex the toes against resistance).
Extensor hallucis longus (dorsiflex the big toe against resistance).
Inversion
Tibialis posterior (foot in plantar flexion, invert against resistance).
Eversion
Peroneus longus and brevis (foot in plantar flexion, evert against resistance).
Special tests
Ankle sprains are classified as:
Grade 1: is painful without instability.
Grade 2: demonstrates mild instability.
Grade 3: complete rupture.
Anterior draw test
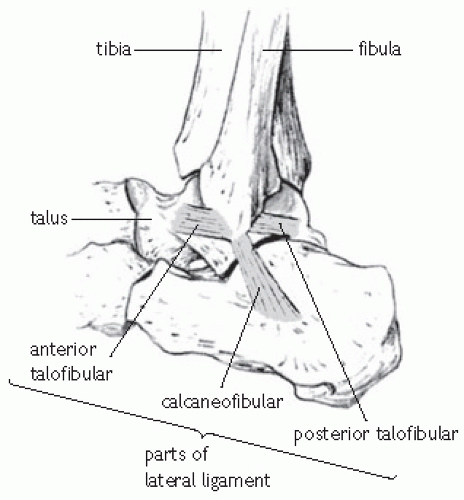
A positive anterior draw test in plantar flexion implies injury to the ATFL. It is performed by holding the heel and pulling the foot anteriorly, while applying a posterior force to the tibia. Alternatively, fix the foot to the examination couch and push the tibia posteriorly (knee flexed to relax gastrocnemius, foot in 10° plantar flexion). A positive anterior draw test in neutral suggests additional injury to the CFL and possibly the PTFL.
Talar tilt test
The talar tilt test examines for CFL instability. It is performed by holding the calcaneum and inverting the talus on the tibia. A talar tilt of 15° or 5° more than the opposite ankle is positive.
Tinels test
Tapping the posterior tibial nerve as it winds round the medial malleolus results in radiation of pain and paraesthesia along its course (heel and medial arch of the foot).
The squeeze test
Is positive when compression of the proximal tibia and fibula precipitates distal pain in the region of the interosseous membrane suggesting an injury to the syndesmosis.
External rotation test
Knee flexed 90°, foot held and rotated laterally with the ankle in neutral. Positive test—pain over the syndesmosis.
Functional tests
Squat.
Heel raise.
Single leg stance.
Single leg squat.
Lunge.
Hop.
Jump.
Investigations
Radiographs
The use of radiographs with acute ankle injuries is guided by the Ottawa rules.
Ankle radiograph—malleolar pain
Inability to weight-bear after injury and in Emergency Department.
Bone tenderness posterior edge or tip of medial malleolus.
Foot radiographs
Bone tenderness base of 5th metatarsal.
Bone tenderness navicular.
Inability to weight-bear after injury and in Emergency Department.
Stress radiographs
May provide further assessment for ankle instability. Stress views include the talar tilt and anterior draw test views. Variables include patient cooperation, amount of force used, amount of laxity on the uninvolved side.
CT may be useful for evaluating osteochondral injuries and stress fractures.
MRI may be useful if evaluating ligament injuries, tendon injuries, osteochondral injuries or meniscoid lesions in patients with a history of recurrent ankle pain and discomfort.
Musculoskeletal US images to evaluate associated tendon injuries.
Acute ankle sprain
History and examination
Acute ankle sprains can occur in any sport but are most common in sports that involve a change of direction or jumping e.g. football, rugby, basketball, netball, and volleyball. The lateral ligament includes the ATFL, CFL, and PTFL. The medial or deltoid ligament is composed of four bands— three superficial and one deep. The interosseous ligaments include the anterior tibiofibular ligament, posterior tibiofibular ligament, and interosseous ligament (see Fig. 23.3).
The mechanism of injury is important, an inversion injury suggests lateral ligament sprain, an eversion injury medial ligament sprain. Compression may suggest an osteochondral injury.
Inversion injuries account for 70-85% of all ankle injuries. They occur when the foot is plantar flexed and inverted. Inversion injuries lead to sprains of the lateral ligament complex including the ATFL, CFL, and PTFL.
The ATFL is most susceptible to injury. The CFL is injured in 40% of ATFL injuries. Complete tears of the ATFL, CFL, and PTFL result in ankle dislocation and are often associated with a fracture.
The location of pain and swelling normally indicates the ligaments injured, most commonly the anterolateral aspect of the ankle joint involving the ATFL.
Ability to weight-bear after the injury suggests a sprain and not a fracture.
Clinical examination includes palpation of the ligaments, tendons, and also the lateral and medial malleoli, base of the fifth metatarsal, and proximal fibula to consider collateral injuries.
Investigations
Radiographs are required if the patient cannot weight-bear or has point tenderness, particularly over the malleoli, tarsal navicular, base of the fifth metatarsal, or proximal fibular (Ottowa rules).
Repeat radiographs should be considered if there is no improvement or progress is delayed.
Radiographs should include the base of the fifth metatarsal to exclude a fracture.
Anteroposterior, lateral, and mortis views are required. Fractures including osteochondral injuries to the medial and lateral talar dome should be excluded.
Mortis views assess the distal tibial syndesmosis. Widening between the tibia and fibula (>5.5mm), and/or talus and medial malleolus (>4mm) indicates injury to the syndesmosis and deltoid ligament.
MRI not usually indicated unless unusual features (severe swelling, bruising or pain) suggest an osteochondral injury not observed on plain radiographs.
If symptoms persist 4-6 weeks after an apparently simple ankle sprain an MRI is indicated to exclude an osteochondral injury.
Treatment
Initial treatment traditionally consisted of protection, rest, ice, compression, elevation and support (PRICES). More recently a modification of this acronym substitutes ‘optimal loading’ for rest and the acronym becomes POLICE. Optimal loading is more appropriate in facilitating early rehabilitation.
Analgesics or NSAIDs for pain.
Compression and elevation help reduce swelling.
Protective devices include air splints or braces.
Surgery: operative repair of Grade 3 AITFL injuries and medial ankle ligament injuries does not improve outcome. Surgery is required for injuries associated with a distal AITFL rupture with widening of the ankle mortise.
Adequate rehabilitation is required to prevent functional instability and injury recurrence.
Restore range of movement.
Strengthen dynamic ankle stabilizers (ankle evertors and dorsiflexors).
Proprioception, e.g. wobble board, mini-trampoline.
Functional exercises, e.g. jumping, hopping, twisting.
Return to sport: athletes can return to sport when they can perform sport specific actions without pain or instability.
Functional bracing or taping may be required to prevent recurrence.
The recurrence rate for lateral ankle sprains is as high as 80%
Persistent painful ankle
Pain, swelling, and impaired function may persist for 4-6 weeks after an acute injury. Secondary injuries may be overlooked at the time of the original injury. With persistent symptoms one should look for occult injury in addition to acute ankle sprain. Functional instability resulting from inadequate rehabilitation is the commonest cause, although there are a number of other possible causes.
Osteochondral injuries
Initial radiographs may appear normal. Repeat radiographs or MRI are required for diagnosis.
Osteochondral injuries occur most commonly at the following sites:
Superomedial talus.
Superolateral talus.
Tibial plafond.
Fractures
Initial radiographs may appear normal. Follow-up radiographs or MRI may be required for diagnosis.
Lateral talar process.
Anterior calcaneal process.
Posterior talar process.
Os trigonum fracture.
Fracture base of fifth metatarsal.
Impingement syndromes
Anterior impingement syndrome.
Anterolateral impingement syndrome.
Posterior impingement syndrome.
Capsular injury resulting in synovitis can present with anterior impingement on dorsiflexion.
Synovium or ruptured ATFL becomes trapped between the lateral malleolus and talus provoking anterolateral impingement.
Tendon dislocation and rupture
Peroneal tendons
Radiographs may demonstrate a small bone chip.
Resisted eversion in dorsiflexion precipitates tendon subluxation.
Tibialis posterior tendon
Occurs with ankle dorsiflexion and inversion.
Subluxation may be demonstrated by resisted plantar flexion.
Sinus tarsi syndrome
Small osseous canal anterior and inferior to the lateral malleolus.
Pain from subtalar ligament injury and fat-pad necrosis.
Diagnosis confirmed by a local anaesthetic injection into the sinus tarsi.
Other causes
Antero-inferior tibiofibular ligament
Synovitis or ATFL scar tissue produces a meniscal lesion that impinges between the lateral talus and lateral malleolus.
Post-traumatic synovitis.
Calcaneocuboid ligament sprain (a bony fleck may be seen adjacent to the cuboid).
Peroneal nerve or sural nerve injury.
Rehabilitation after ankle sprain (grade 2)
Time to return to sport is based largely on the quality of early management. Early, intermediate, and late rehabilitation objectives should be highlighted immediately after diagnosis. It is not possible to move on to the later stages of rehabilitation until all early stage goals are achieved. The athlete should be aware that progressive rehabilitation is necessary to minimize the chances of recurrence. Although rest is included in most guidelines, rehabilitation means progressive activity or optimal loading. Substituting rest in the PRICE guidelines creates the more appropriate POLICE. The anticipated time to return to sport after grade 2 injuries is 3-6 weeks. Note much of this programme is applicable for recovery after more minor, or severe injuries; however, the rate of progression will vary.
Early stage: days 1-7
Key aims
Minimize swelling.
Maintain range of movement and general ankle mobility.
Begin controlled loading—optimal loading.
Begin isometric strengthening.
Challenge balance (neuromuscular control).
Maintain upper body strength and cardiovascular fitness.
General exercises
The athlete should be encouraged to weight-bear or partially weight-bear within the limits of pain. The use of crutches may be useful, but should not be to excess. A heel-toe gait pattern should be encouraged at all times. This will prevent the development of a toe-tap gait and minimize over activity/shortening of triceps surae.
Ice, compression, and elevation can be of benefit after injury:
Applying focal compression around the malleolous may be most effective at preventing oedema accumulating around the healing ligaments.
Focal compression should be removed before cryotherapy is initiated, in order to prevent a barrier effect which can reduce the effectiveness of cooling.
Gentle mobility exercises should be encouraged as soon as pain allows. Range of movement through dorsiflexion and plantar flexion should be followed by light circling exercises.
The athlete may perform alphabet exercises—this involves using ankle movements to trace each letter of the alphabet in the air. This becomes more challenging with closed eyes and helps restore kinesthetic awareness (awareness of the foot and ankle in space) after joint injury. Kinesthetic training can also include matching or reproducing various joint angles or foot positions.
Cryokinetics is a technique that involves performing mobility exercises immediately after or during cryotherapy. The pain relieving effect of cooling can reduce muscle spasm and inhibition, facilitating rehabilitative exercises.
The athlete should begin static stretching of the triceps surae as soon as pain allows. Stretching can be performed in a non-weight bearing position initially. For example, using a towel or belt around the foot to pull the ankle into dorsiflexion. If pain allows, gentle calf stretching can be performed in standing.
In certain cases, stretching should also include the flexor hallucis longus complex; to do this, the athlete should replicate the triceps surae stretch position in bare feet, concomitantly stretching the 1st toe into extension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree