Anatomy—Biomechanics and Implant Considerations
Michael L Pearl
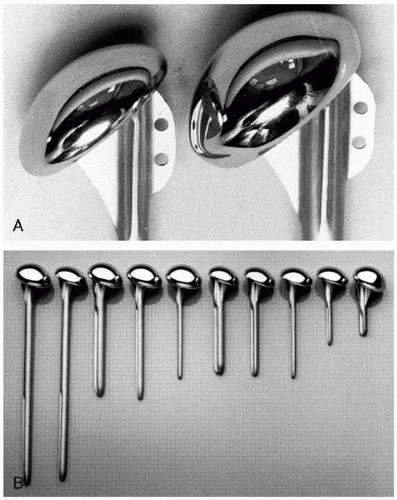
Resurfacing arthroplasty of the glenohumeral joint is now well established as a means to restore comfort and function to the shoulder for many afflictions that derange the normal anatomy. The first detailed description of shoulder arthroplasty dates back to the late 19th century when the French surgeon Jules Emile Pean implanted a device made of metal and hard rubber into a patient that refused an amputation for a chronic infection. The modern era of shoulder arthroplasty began in the mid 20th century with the first efforts to replace the proximal humerus with inert metals. Unquestionably, the single greatest pioneer of these efforts was Dr. Charles Neer, who in 1951 introduced a prosthesis made of vitallium for use in fractures. Through multiple iterations, its use in arthritic conditions became apparent. In 1973 Dr. Neer released a version made of cobalt chrome (Fig. 2-1) along with a polyethylene glenoid component. Subsequent designs over the last
three decades have incorporated more prosthetic sizes, modularity between the stem and head, and differentshaped prosthetic bodies with some made of materials such as titanium. Dr. Neer and others also explored a variety of fixed fulcrum designs, but these largely gave way to the original unconstrained design, except for more recent use in special situations (e.g., cuff tear arthropathy). Presently, we can reflect on shoulder arthroplasty from the vantage point of 50 years of accumulated clinical experience and of a modern understanding of shoulder anatomy and biomechanics.
three decades have incorporated more prosthetic sizes, modularity between the stem and head, and differentshaped prosthetic bodies with some made of materials such as titanium. Dr. Neer and others also explored a variety of fixed fulcrum designs, but these largely gave way to the original unconstrained design, except for more recent use in special situations (e.g., cuff tear arthropathy). Presently, we can reflect on shoulder arthroplasty from the vantage point of 50 years of accumulated clinical experience and of a modern understanding of shoulder anatomy and biomechanics.
GOALS OF ARTHROPLASTY
The general goal of arthroplasty is to restore comfort, motion, and function that has been lost from arthritic deformation of a joint. The goal of shoulder arthroplasty specifically is to replace the humeral and glenoid articular surfaces with prosthetic ones to achieve these more general goals. Latter but related goals include host acceptance of the prosthetic materials and implant longevity. Among those factors involved in achieving a successful shoulder arthroplasty are restoration of normal biomechanics (or the creation of normal prosthetic mechanics), surgical technique that does not further derange the anatomy, and solid fixation of durable implants. Here we primarily will concern ourselves with prosthetic design considerations and related implantation techniques that facilitate a return to functional biomechanics.
SUMMARY DESIGN HISTORY
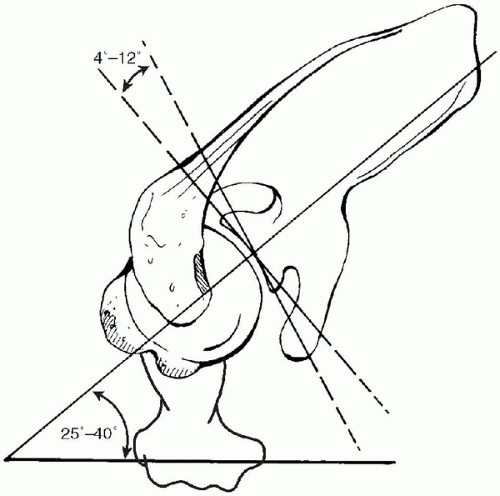
To fully appreciate the relevance of recent developments in shoulder arthroplasty, it is important to understand the historical context from which they emerged. Through the 1970s and most of the 1980s, Dr. Neer’s design and clinical experience constituted the majority of the world’s experience (1). Reports from other authors that appeared in the literature usually used the Neer II implant. Sporadic series appeared using other designs, DANA (2) and Gristina (3,4), but they were similar to the Neer implant in many respects. Toward the end of the 1980s and into the early 1990s, borrowing from developments in hip arthroplasty that aimed for more secure implant fixation, designs emerged that included longer stems, bigger prosthetic bodies, and modularity between the head and the stem. These designs are exemplified by the Biomet Biomodular prosthesis, the Intermedics Select prosthesis, the Depuy Global shoulder, and the Kirschner IIC Modular prosthesis (Fig. 2-2).
The Neer II implant is a single-pieced (nonmodular) structure. It has only a few stem sizes and two head thicknesses with the heads based on a 1-inch radius of curvature. The base of the head is inclined 50 degrees relative to the axis of the stem. At the time of its introduction, relevant anatomic data were sparse and essentially nonexistent in the literature. The modular designs that followed were based on the clinical success of the Neer II implant and aimed to improve it with contemporary thinking on implant fixation and durability. Additional benefits of modularity often were discussed, such as better fitting an individual patient by mixing and matching various stem and head sizes. With each new prosthetic system, the number
of stem and head sizes proliferated, as did the number of shoulder arthroplasties performed.
of stem and head sizes proliferated, as did the number of shoulder arthroplasties performed.
 Figure 2-2 Example of so-called second-generation prosthesis, with head suspended from collar by taper locking mechanism and one central position of head for each head-stem combination. |
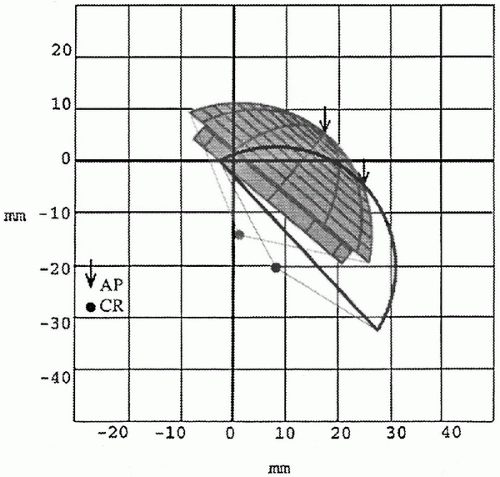 Figure 2-3 Two-dimensional plot showing mismatch between position of prosthetic head and the anatomic head as determined by computer optimization. Note how for this prosthetic construct, the collar and locking mechanism accentuate mismatch. (From Pearl ML, Kurutz S. Geometric analysis of commonly used prosthetic systems for proximal humeral replacement. J Bone Joint Surg Am 1999;81(5):660-671, with permission.) |
Rigorous study of shoulder anatomy in terms relevant to prosthetic geometry, however, did not begin until the 1990s (5, 6, 7, 8, 9, 10). It became apparent that normal anatomy was aligned somewhat differently than common prosthetic devices, and it also became clear that normal anatomy was highly variable from individual to individual. In terms of replicating normal anatomy, the simple Neer II implant with its smooth stem offered some advantages over the larger modular designs that were much more constrained with respect to their position in the canal. Most importantly, the Neer II implant placed the prosthetic head directly on the humeral osteotomy, whereas the modular systems propped it up 4 to 5 mm above the osteotomy because of the prosthetic collar and the taper lock of the modular head (Fig. 2-3). Ironically, these differences made it very difficult to restore normal anatomy using the more modern modular systems (11,12).
ANATOMIC HUMERAL RECONSTRUCTION
Emphasis on anatomic humeral reconstruction initially came primarily from Europe, most notably from France embodied in the Tornier Aequalis prosthesis. Other designs from within France and from neighboring countries followed quickly, associating the 1990s with an explosion of implant options and design features. Concomitantly, independent anatomic studies validated many of the concerns raised by proponents of anatomic replacement (5,9,11,13). Subsequent biomechanical studies have further supported many of these conclusions (14,15). New designs have continued to emerge from North America and Europe.
GLENOID LOCATION AND INCLINATION
Developments in the glenoid component unfortunately have not kept pace with those of the humeral component. This is not necessarily for lack of trying but more that new developments have not shown much superiority to the keeled implant originally offered by Dr. Neer. Metal-backed glenoids, although undergoing resurgence, often failed worse than their all-polyethylene counterparts. Pegged designs have emerged but with no definitive claim to superiority. Better techniques of implantation have been developed but none that significantly alter the reality that polyethylene glenoids wear thin and loose their fixation in the bone.
SUMMARY
This chapter aims to review current anatomic, biomechanical, and prosthetic considerations necessary for a modern understanding of shoulder arthroplasty. These considerations explain in part why prosthetic systems are designed as they are. They also may highlight strengths and weaknesses of one system over another. Prosthetic design by its nature is evolving constantly. The information covered in this chapter should offer a basis from which to evaluate new developments as they emerge. Most importantly, a basic knowledge of this information is a necessary foundation for any surgeon undertaking shoulder arthroplasty.
ANATOMIC FACTORS—HUMERUS
Retroversion
Multiple studies have shown that the retroversion of the proximal humeral articular surface is markedly variable, not only between individuals but also between the left and the right sides of the same individual (6,9,16,17). Depending on the methodology used, retroversion ranged from 0 degrees to 55 degrees. Studies differ on the reference axes used to define retroversion (Fig. 2-4). The proximal reference axis has been defined by either the plane of the articular surface, a line connecting the center of rotation and the central point of the articular surface, or a line from the greater tuberosity to the central point of the articular surface. The distal reference axis has been defined by the trochlear axis, a line between the epicondyles, or the forearm itself. For any given individual, retroversion will measure differently depending on which axes are used to make the measurement.
Head Shaft Angle
The inclination of the proximal humeral articular surface relative to the shaft (head shaft angle or HSA) is also variable, ranging from 30 degrees to 55 degrees, depending on the study (Fig. 2-5). Measurements again vary depending on methodology. The base of the articular surface can be approximated by a plane, but there clearly is room for interpretation in establishing this reference. Similarly, the proximal humeral canal is conical in shape and defining its central axis is subject to variability.
Offset
The position of the proximal humeral articular surface relative to the shaft can be characterized by the distance of its center of rotation from the central axis of the canal, the humeral offset (OS). In the coronal plane, this is the medial offset (Fig. 2-5). In the transverse plane, this is the anteroposterior offset (Fig. 2-6). Typically, the humeral head center is offset from the center of the canal in both the coronal and transverse planes. Medial offset ranges from 4 mm to 14 mm (6,8,17); posterior offset ranges from -2 mm to 10 mm (5,10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree