Amputation/Prosthetics
EPIDEMIOLOGY, ETIOLOGY, AND LEVELS OF AMPUTATION
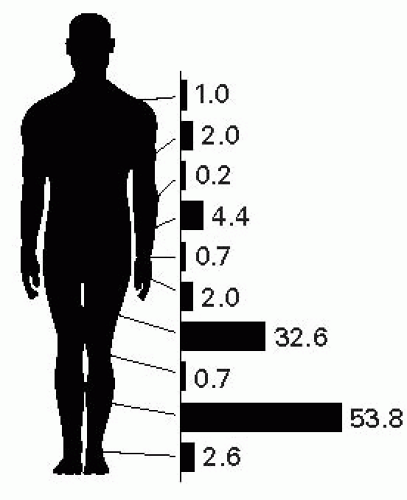
In the United States, an estimated 185,000 people undergo an amputation of an upper or lower limb each year. It is estimated that 1.2 million people are living with the loss of a limb.1 Amputation due to dysvascular disease accounts for 54% of cases, and of these, two-thirds have a diagnosis of DM. Trauma accounts for 45% of cases and cancer for the remaining less than 2%.
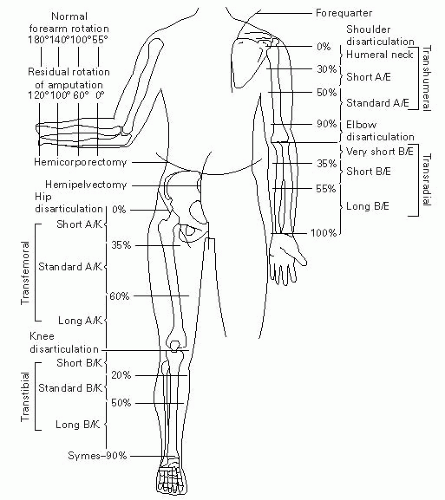
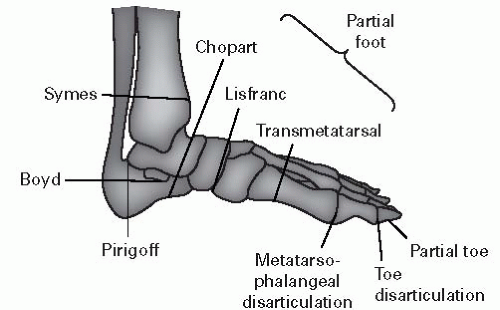
Over the next 45 years, the number of persons living with loss of a limb is predicted to more than double. Figures 4-1, 4-2, and 4-3 illustrate some of these data.
Preferred Mature Residual Limb Length and Shape
Transhumeral – Cylindrical appendage with retention of the deltoid tuberosity. Generally, the longer the better (up to 90% of normal length).
Transradial – Ideal shape follows the contours of the natural limb. Longer appendages provide better lever arms and more pronation/supination and are optimal for body-powered prostheses and heavy labor. Retention of the brachioradialis improves elbow flexion. Medium length limbs are optimal for externally powered prostheses.
Transfemoral – Ideal shape is conical. Longer residual limbs improve seating balance and tolerance. For shorter limbs, maintaining the greater trochanter and its attachment to the hip abductors is key.
Transtibial – Ideal shape and length is a cylindrical appendage about one-third the original tibial length, with retention of the patellar tendon attachment to the tibial tuberosity. The fibula should be shorter than the tibia. In vascular disease, longer limbs may not have adequate circulatory supply and fitting of the below-knee socket may be problematic. The ideal length recommended from medial tibial plateau to bony end is 5″ to 7″.
BASIC LEX POSTAMPUTATION PREPROSTHETIC CARE
Wound Care – Keep limb clean and protected and debride any nonviable tissue.2
Edema Control
Elastic wraps: Most commonly Ace bandages. Must use figure-of-8 elastic wrapping, which should begin immediately after surgery and should ideally be rewrapped qid. May be time consuming.
Elastic socks: Alternative to wraps. Not expensive and easy to apply.
Rigid dressings: Protective. Allow for weight bearing to desensitize the limb. Examples include the immediate postoperative-fitting prosthesis, which is not removable and therefore inhibits ability to check and desensitize the skin. The removable rigid dressing is custom made and allows for wound inspection and desensitization.
Scar mobilization massage should be instituted as soon as tolerated to help prevent adherence of the scar to the underlying soft tissues and bone. Once the sutures are removed, the massage can be performed more aggressively.
Anticontracture Management – Due to muscle imbalance. AKA commonly develop HF, hip abduction, and hip external rotation contractures. In addition, BKA develop KF contractures. Prevent with a firm mattress, prone lying 15 minute tid, and promoting knee extension while resting. A posterior splint to maintain knee extension can be considered for patients at higher risk.
Preprosthetic and Prosthetic Training – Hip AROM and strengthening exercises are key. A good test to determine cardiovascular tolerance for prosthesis use is ambulation with a walker (without a prosthesis). Prosthetic gait training should begin with parallel bars and progress to walkers or canes. Crutches should be avoided since they promote poor gait patterns. The definitive prosthesis is usually created at 3 to 6 months.
TRANSTIBIAL PROSTHETICS
Socket Designs
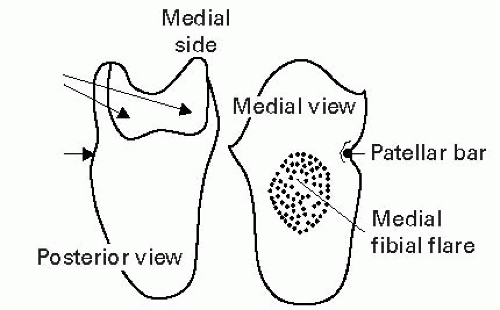
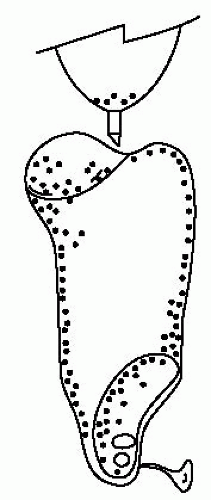
The socket connects the residual limb to the rest of the prosthesis and plays an important role in the transfer of body weight to the ground (Fig. 4-4).
The PTB socket is an old term for the total contact socket. The patellar tendon actually only bears a moderate load. Weight is distributed over many areas (see “pressure-tolerant areas” in Fig. 4-5), but not over the bony prominences.
For any socket, soft inserts made of polyethylene foam or silicone gel provide extra protection, e.g., for cases of PVD or extensive scarring. The inserts, however, reduce the intimacy of contact between the limb and prosthesis, which is important for proprioception. A soft foam distal end discourages verrucous hyperplasia formation.
Selected Suspension Options
Differential Pressure (Silicone Suction with Shuttle Lock) – A flexible, molded silicone liner is rolled directly onto the residual limb and secured to the socket with a pin. This provides optimal suspension and proprioception, but requires stable limb volumes and good hand dexterity for donning/doffing.
Anatomic – A brim suspension is an extension of the socket over the femoral epicondyles. This design is easy to don/doff, provides mediolateral knee stability, and is useful for short limb lengths.
The supracondylar cuff clips on above the epicondyles and is a common suspension option. This design is not indicated in patients with very short residual limbs or with mediolateral knee instability. A supracondylar cuff with fork strap and waist belt suspension provides additional stability for very active patients, e.g., manual laborers.
Sleeve – An elastic sleeve can serve as a primary or secondary suspension via longitudinal tension and negative pressure during swing phase. It can provide additional security for short residual limbs, when mediolateral knee stability is questionable, or when hyperextension control is required (Fig. 4-6).
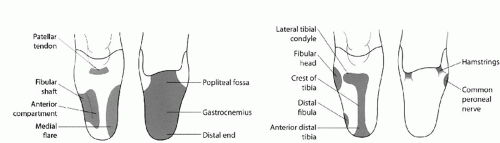 Figure 4-5 Pressure-tolerant/sensitive areas in the transtibial total contact socket. From Braddom RL. Physical Medicine & Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2011, with permission. |
Selected Foot-Ankle Assembly Options
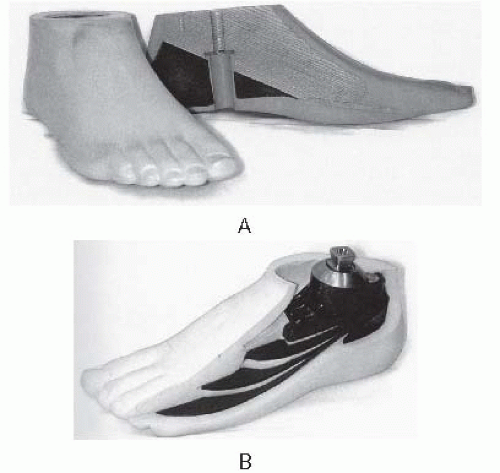
Solid Ankle Cushioned Heel Foot – SACH feet are light, durable, inexpensive, and stable. The soft heel simulates PF during heel strike (Fig. 4-7A).
Single-Axis Foot – These feet are heavier but less durable than the SACH feet. They are most commonly used for TF amputees, i.e., when knee stability is desired (a quick foot flat improves knee stability). Only sagittal axis movement is allowed.
Multiaxis Foot (Greissinger, Endolite Multiflex, SAFE II, TruStep) – The multiaxis foot allows PF/DF, inversion/eversion, and rotation, which improve balance and coordination. It provides good shock absorption and is good for uneven ground, but is heavy, costly, and needs relatively frequent adjustments or repairs.
DER Foot (Seattle Light, Carbon Copy II, Quantum Foot, Flex-Foot, SpringLite) – These feet were formerly called “energy-storing feet,” but they have not demonstrated a reduction in the energy cost or rate of energy expenditure during level walking, compared with the SACH foot.3 They may, however, be more efficient than other feet at higher speeds. Geriatric amputees benefit from the light weight of these feet (Fig. 4-7B).
TF PROSTHETICS
Traditional Socket Designs
TF sockets are often fitted in slight (5°) flexion and adduction to stretch the hip extensors and abductors and give them a mechanical advantage.
QUADRILATERAL DESIGN
This ischial-gluteal weight-bearing, narrow anteroposterior design was originally designed by Inman and Eberhart at UC Berkeley in the 1950s. It has four sides and four corners. It is easy to make and fit but less stable for shorter residual limbs and less comfortable when sitting than the ischial containment design (Fig. 4-8A).
ISCHIAL CONTAINMENT DESIGN
A “bony lock” incorporates the ischial tuberosity, pubic ramus, and greater trochanter. The posterior rim provides ischial-gluteal weight bearing and is contoured for the ischial tuberosity and gluteal muscles. These features improve stability, particularly for shorter residual limbs. The narrow mediolateral design also provides a more efficient energy cost of ambulation than the narrow anteroposterior design at high speeds (Fig. 4-8B).
Selected Suspension Options
Suction – Subatmospheric socket pressure maintains prosthetic attachment during swing phase. The sock bandage is pulled through a one-way valve hole. Its use is indicated in active amputees with well-shaped, nonfluctuating residual limbs.
Silesian Belt or Bandage – A belt that attaches from the socket at the greater trochanter and wraps around the opposite iliac crest (Fig. 4-9A).
Total Elastic Suspension (Belt) – Wraps around the proximal prosthesis and waist, enhancing rotational control. It retains body heat and has limited durability (Fig. 4-9B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree