Adult traumatic brachial plexus injury involves injury of the C5-T1 spinal nerves. Common patterns of injury include “upper arm” and “total arm” types. The specific signs of preganglionic avulsion injury infer a poor prognosis for spontaneous recovery and surgery may be needed. Detailed preoperative evaluation is recommended for localization of the lesions. The treatment of upper arm type injury comprises restoration of elbow flexion and shoulder control. Good functional results may be achieved after multiple nerve transfers. The treatment of total arm type includes hand function reconstruction, in addition to shoulder and elbow treatment. Current options for hand function reconstruction include functioning free muscle transfers and nerve transfers.
Key points
- •
Brachial plexus injury involves damage to the C5-T1 spinal nerves. Common injury patterns include “upper arm type” (C5-6 ± C7) and “total arm type” (C5-T1).
- •
Preganglionic avulsion injury is suspected when the following observations are noted: Horner syndrome, winged scapula, absence of Tinel sign over the neck, hemidiaphragm paralysis, and pseudomeningocele. This type of injury infers poor potential for spontaneous recovery.
- •
The treatment of upper arm type injury involves the restoration of elbow flexion and shoulder control. Good results can be achieved by using nerve transfer surgery.
- •
The treatment of total arm type injury involves the re-establishment of shoulder, elbow, and hand function. The use of functioning free muscle transfers or nerve transfers may restore hand function.
Introduction
Traumatic brachial plexus injury (BPI) is regarded as one of the most devastating injuries of the upper extremity. Patients typically lose sensation, motor power, and may experience disabling neuropathic pain. Several decades ago, combined arm amputation, shoulder arthrodesis, and prosthetic replacement was a viable treatment option for patients with a flail arm, because this protocol resulted in superior functional results compared with other reconstructive procedures at that time, which included tenodesis, bone block, and arthrodesis. However, advances in peripheral nerve surgery over the last few decades have significantly changed the image and outcomes of brachial plexus treatment. Today, one can expect good to excellent functional results in patients with upper arm deficits. Although there remains much room for optimizing the functional results in patients with a flail arm, today’s outcomes following reconstructive surgery have improved to a degree that renders amputation as an antiquated treatment option.
The treatment of BPI is based on a combination of evidence-based principles, practical feasibility, and the personal philosophy of the surgeon. In many instances, dogmatic practices flourish because of differences in the surgeon’s approach, the patient’s injuries and expectations, and the cultural environment. Over the past few decades, there has been a fair amount of trial and error in BPI surgery and some techniques have developed a reputation for consistent and encouraging results, whereas others have become of historical interest. This article provides an overview of the anatomy, diagnosis, and treatment of posttraumatic adult BPI. In addition, some of the controversial topics surrounding the management of this complex injury are addressed.
Introduction
Traumatic brachial plexus injury (BPI) is regarded as one of the most devastating injuries of the upper extremity. Patients typically lose sensation, motor power, and may experience disabling neuropathic pain. Several decades ago, combined arm amputation, shoulder arthrodesis, and prosthetic replacement was a viable treatment option for patients with a flail arm, because this protocol resulted in superior functional results compared with other reconstructive procedures at that time, which included tenodesis, bone block, and arthrodesis. However, advances in peripheral nerve surgery over the last few decades have significantly changed the image and outcomes of brachial plexus treatment. Today, one can expect good to excellent functional results in patients with upper arm deficits. Although there remains much room for optimizing the functional results in patients with a flail arm, today’s outcomes following reconstructive surgery have improved to a degree that renders amputation as an antiquated treatment option.
The treatment of BPI is based on a combination of evidence-based principles, practical feasibility, and the personal philosophy of the surgeon. In many instances, dogmatic practices flourish because of differences in the surgeon’s approach, the patient’s injuries and expectations, and the cultural environment. Over the past few decades, there has been a fair amount of trial and error in BPI surgery and some techniques have developed a reputation for consistent and encouraging results, whereas others have become of historical interest. This article provides an overview of the anatomy, diagnosis, and treatment of posttraumatic adult BPI. In addition, some of the controversial topics surrounding the management of this complex injury are addressed.
Anatomy, function, and localization of lesions
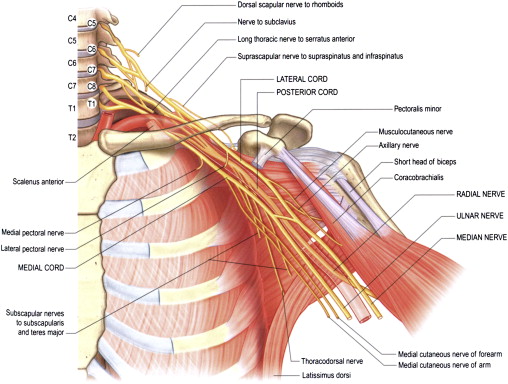
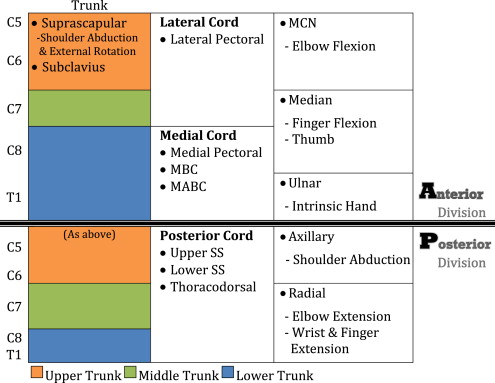
The brachial plexus is usually formed by the ventral rami of five spinal nerves (C5-T1), although some variations exist, which involve contributions from the C4 (prefixed) or T2 levels (postfixed). The small dorsal rami, which are not part of the plexus, supply the paraspinal muscles and skin of the posterior neck. After once the spinal nerves pass through the spinal foramina, they form the brachial plexus between the scalenus anterior and the scalenus medius muscles. The anatomy of the brachial plexus is normally divided into five segments: (1) spinal nerves or roots, (2) trunks, (3) divisions, (4) cords, and (5) terminal branches ( Figs. 1 and 2 ).
Spinal Nerves
Two terminal nerves emerge at the level of the spinal roots: the dorsal scapular nerve (C4-5), which supplies the levator scapulae and rhomboid muscles; and the long thoracic nerve (C5-7), which supplies the serratus anterior muscle. Injury to this nerve results in scapular winging.
The phrenic nerve (C3-5), considered an extraplexal nerve, lies on the scalenus anterior muscle. Therefore, plexus injury at the root level may cause paralysis and subsequent elevation of the diaphragm.
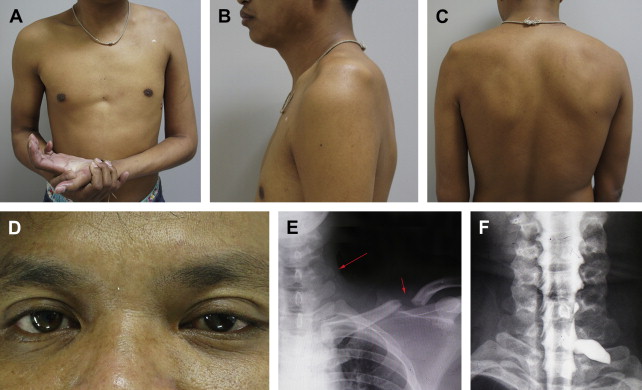
The sympathetic ganglion lies in close proximity to the brachial plexus at the T1 root level. Therefore, injury to the lower root may be associated with Horner syndrome, which consists of miosis, enophthalmos, ptosis, and anhydrosis ( Fig. 3 ).
Trunks
Two terminal nerves emerge at the level of the trunks: the suprascapular (SSC) nerve (C5-6), which supplies the supraspinatus and infraspinatus muscles, arises from the superolateral aspect of the upper trunk, at a location referred to as Erb’s point; and the nerve to the subclavius muscle (C5-6), which is smaller than its aforementioned counterpart and arises from the medial side of the upper trunk.
Divisions
The division level could be conceptualized as the equator of the brachial plexus. The all roots form the trunks that travel posterior to the clavicle and then split into anterior and posterior divisions that supply the flexor and extensor muscles respectively (see Fig. 2 ).
Cords
After the brachial plexus has traveled distal to the clavicle, or has become infraclavicular, it becomes invested by the axillary sheath. The anterior divisions of the upper and middle trunks form lateral cord, and lower trunk becomes medial cord. The posterior divisions of every trunk form the posterior cord by contributing various proportions of spinal nerve roots. These cords are named in reference to their anatomic relationship to the second part of the axillary artery, which is located posterior to the pectoralis minor muscle.
It should be noted that the aforementioned anatomic description characterizes an uninjured brachial plexus. During surgical exploration of BPI, however, the anatomy becomes more distorted and complicated because there is usually nerve retraction and associated fibrotic scar formation. Often, the chronically avulsed plexus is found to be retracted distally and located posterior to the clavicle. In addition, anatomic variations within the brachial plexus are not uncommon, and serve to further complicate anatomic exploration.
Classification, mechanism, and patterns of the injury
Previous reports have classified BPI according to a combination of injury mechanism, degree of nerve injury, location, and level of injury.
Mechanism of Injury
An understanding of the mechanism of injury may help predict the type of brachial plexus lesion. Closed BPIs are usually associated with a traction mechanism where the arm and shoulder are forcefully distracted away from the neck or trunk. This mechanism mostly results in root avulsion lesions and 70% to 80% of these injuries have been found to occur in motorcycle accidents. In these cases, spontaneous recovery rarely occurs. Other less common mechanisms include crush or compression caused by various mechanisms, such as compression of the clavicle against the rib cage secondary to seatbelt restraint, anterior shoulder dislocation, or iatrogenic surgical positioning. Crush or compression injury mechanisms tend to involve the infraclavicular part of the plexus, such as the cords or terminal braches, which may have some recovery potential.
Open BPI is usually a result of stab wounds, gunshot wounds, and sometimes open fractures of the shoulder girdle. In patients with gunshot wounds, the initial neurologic deficit is often extensive; however, one report showed that only 12% to 15% of patients sustained transected nerve lesions. Open fractures of the shoulder girdle usually occur after high-energy injuries, in which the combination of nerve root avulsion and major vessel injury should be suspected ( Fig. 4 ).
Degree of the Nerve Injury
The classification systems of peripheral nerve injury into neurapraxia, axonotmesis, and neurotmesis by Seddon and first- to fifth-degree injury by Sunderland are generally used to describe BPI. Neurapraxia, or Sunderland’s first-degree injury, refers to localized myelin damage and conduction deficiencies. Complete recovery could be expected in 4 to 12 weeks. Axonotmesis or second-degree injury refers to a disruption of the nerve cell’s axon, followed by wallerian degeneration. Complete axonal regeneration could be expected to occur at a rate of approximately 1 to 3 mm/day from the injury site to the target muscle. During third-degree injury, internal derangement of the endoneurium and intrafascicular fibrosis precludes complete regeneration and results in partial recovery. In fourth-degree injury, owing to perineurial and fascicular disruption, neuroma in-continuity forms and spontaneous recovery is not expected. Neurotmesis, or fifth-degree injury, refers to complete nerve transection and the need for surgical intervention. MacKinnon and Dellon added a sixth-degree injury as a combination of first- to fifth-degree fascicular injuries within the same nerve. This injury results in variable recovery and prognosis.
Location and Level of the Injury
Several terms and classification systems have been used to categorize the location and level of BPI. In our experience, sometimes it is difficult to define the exact location of injury. Therefore, we prefer to use a simple and practical classification scheme that divides injury location into two groups: supraclavicular or infraclavicular lesions. Supraclavicular lesions imply injury at the spinal nerve and trunks levels. Similar to other authors, we have found that further subdivision into preganglionic and postganglionic lesions is beneficial during treatment planning and is of prognostic value. The signs that suggest a preganglionic injury are presented in Table 1 . Infraclavicular lesions mostly occur at the cord and terminal branch levels (see Fig. 4 ). In Narakas’ series, approximately 10% of patients had combined supraclavicular and infraclavicular lesions. The common neurologic deficit patterns according to the level of the injury are presented in Table 2 .
| Signs and Findings | Implications |
|---|---|
| Horner syndrome | Sympathetic ganglion injury (T1 level) |
| Winged scapula | Long thoracic nerve injury (C5-7) |
| Atrophy of parascapular muscle | Dorsal scapular nerve injury (C4-5) |
| Cervical paraspinal muscle weakness and loss of posterior neck sensation | Dorsal rami of cervical spinal nerve roots injury |
| Hemidiaphragm paralysis | Phrenic nerve injury (C3-5) |
| Absence of Tinel sign in neck area | Absence of proximal spinal nerve stump |
| Pseudomeningocele on myelogram | Development of meningeal diverticulum after healing of torn nerve root sleeve |
| Intact sensory nerve action potentials in the area of sensory deficit | Imply no wallerian degeneration of the sensory axons because the attached nerve cells reside in the dorsal root ganglion |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





