Traumatic brain injury (TBI) continues to be a major public health problem. Proposed treatments have not withstood testing in clinical trials because of failure to account for different types of TBI and other weaknesses in trial design. Management goals continue to be prevention and prompt treatment of secondary insults (hypotension, hypoxia, and other physiologic derangements). This goal is best accomplished by careful attention to airway, breathing, circulation, and basic principles of intensive care unit management. Attempts to intervene prophylactically to prevent intracranial hypertension or other complications have not been beneficial and may even have deleterious effects.
Key points
- •
Neurocritical care management of traumatic brain injury (TBI) patients focuses on prevention and prompt treatment of secondary insults.
- •
The acutely injured brain is highly vulnerable to brief deviations from normal physiologic values that would normally be well-tolerated.
- •
Treatments administered prophylactically against intracranial hypertension or other harmful sequelae have not been shown to be beneficial in clinical trials and have sometimes produced undesirable effects.
- •
Future advances in the management of TBI require treatments tailored to specific subtypes of patients, such as those with diffuse injury or with surgically evacuated traumatic hematomas.
Introduction
Traumatic brain injury (TBI) has long been a major public health problem. Commonly cited statistics indicate that 1,365,000 Americans visit emergency departments every year because of TBI. It is likely that many more suffer TBI but receive other types of medical care (such as from their primary care physicians) or no care at all. In the United States, TBI causes 275,000 hospitalizations and 52,000 deaths every year, and it is a contributing factor in more than 30% of all injury-related deaths. The number of Americans living with the sequelae of TBI is as high as 5.3 million.
TBI represents a leading cause of death and disability not just in the United States, but across the globe. Many low- and middle-income countries are burdened by a sharp increase in the numbers of motor vehicle-related injuries, a situation often aggravated by poor roads, inadequate enforcement of traffic laws, and underdeveloped prehospital emergency care systems.
TBI is often classified as mild, moderate, or severe based on the Glasgow Coma Scale (GCS; Tables 1 and 2 ). It has frequently been stated that 80% of TBI cases are mild, 10% moderate, and 10% severe. More recently, the proportion of mild cases seems to have increased, possibly because of greater awareness and recognition of concussion and other forms of mild TBI, which are discussed elsewhere in this volume.
| Score | Eye Opening (E) | Verbal (V) | Motor (M) |
|---|---|---|---|
| 6 | — | — | Obeys commands |
| 5 | — | Oriented | Localizes stimulus |
| 4 | Spontaneous | Confused | Withdraws from noxious stimulus |
| 3 | To voice | Inappropriate words | Abnormal flexion |
| 2 | To pain | Incomprehensible sounds | Extension |
| 1 | No eye opening | No sounds | No response |
| Severity | Glasgow Coma Scale Score |
|---|---|
| Mild | 13–15 |
| Moderate | 9–12 |
| Severe | 3–8 |
Classically, the stereotypical TBI patient is a male in his late teens or early twenties. Fortunately, the incidence of interpersonal violence and motor vehicle crashes, which disproportionately affect males in this age group, has decreased in recent years. However, the number of falls among the elderly has increased dramatically as that segment of the population has grown in number. Many of these patients also take newer antiplatelet or anticoagulant medications, which can increase the likelihood and severity of intracranial hemorrhage after a fall.
Research and clinical care in TBI have been held back by persistent use of categorization based on physical examination instead of on underlying pathophysiology. No one would base a huge infrastructure of research, acute care, and rehabilitation on something as nebulous as “abdominal pain” because that term is so broad as to be almost meaningless. Abdominal pain can be caused by gastric ulcer, appendicitis, ischemic bowel, diverticulitis, pancreatitis, and a host of other diseases, which all have their own causes and treatments. A single medication or other treatment cannot be expected to be effective against such a variety of conditions. But the term “TBI” is used to describe any mechanically induced alteration of neurologic function, regardless of the underlying pathophysiologic cause, such as enlarging extraaxial hematoma, diffuse swelling, ischemia, blossoming contusion, and so on. Applying the same uniform approach to these different conditions makes as little sense as applying a single intervention to all patients with abdominal pain. It is no surprise that clinical trials in TBI, which have adopted this approach to patient enrollment, have failed to demonstrate improved outcome from any proposed intervention.
Both the public health burden of this severe and common disease and the exasperating stubbornness with which it has resisted attempts to develop effective treatments illustrate the magnitude of the challenges posed by TBI. This article focuses on the management of adults with moderate and severe closed brain injuries sustained in a civilian setting. The basic principles of management of severe TBI apply to children as much as to adults, but specific goals and parameters may differ. Also, pediatric TBI is characterized by a lower incidence of traumatic mass lesions than seen in adults. Of course, the possibility of intentionally inflicted injury must always be considered in children, just as it is in elderly and other vulnerable patients. Penetrating brain injuries may present interesting challenges in terms of surgical approaches and techniques, but nonsurgical management has much in common with that of closed TBI patients. Similarly, military TBI is often caused by blast injury, which may produce massive brain swelling and cerebral vasospasm. However, other tenets of management are the same as those for nonblast injuries.
Introduction
Traumatic brain injury (TBI) has long been a major public health problem. Commonly cited statistics indicate that 1,365,000 Americans visit emergency departments every year because of TBI. It is likely that many more suffer TBI but receive other types of medical care (such as from their primary care physicians) or no care at all. In the United States, TBI causes 275,000 hospitalizations and 52,000 deaths every year, and it is a contributing factor in more than 30% of all injury-related deaths. The number of Americans living with the sequelae of TBI is as high as 5.3 million.
TBI represents a leading cause of death and disability not just in the United States, but across the globe. Many low- and middle-income countries are burdened by a sharp increase in the numbers of motor vehicle-related injuries, a situation often aggravated by poor roads, inadequate enforcement of traffic laws, and underdeveloped prehospital emergency care systems.
TBI is often classified as mild, moderate, or severe based on the Glasgow Coma Scale (GCS; Tables 1 and 2 ). It has frequently been stated that 80% of TBI cases are mild, 10% moderate, and 10% severe. More recently, the proportion of mild cases seems to have increased, possibly because of greater awareness and recognition of concussion and other forms of mild TBI, which are discussed elsewhere in this volume.
| Score | Eye Opening (E) | Verbal (V) | Motor (M) |
|---|---|---|---|
| 6 | — | — | Obeys commands |
| 5 | — | Oriented | Localizes stimulus |
| 4 | Spontaneous | Confused | Withdraws from noxious stimulus |
| 3 | To voice | Inappropriate words | Abnormal flexion |
| 2 | To pain | Incomprehensible sounds | Extension |
| 1 | No eye opening | No sounds | No response |
| Severity | Glasgow Coma Scale Score |
|---|---|
| Mild | 13–15 |
| Moderate | 9–12 |
| Severe | 3–8 |
Classically, the stereotypical TBI patient is a male in his late teens or early twenties. Fortunately, the incidence of interpersonal violence and motor vehicle crashes, which disproportionately affect males in this age group, has decreased in recent years. However, the number of falls among the elderly has increased dramatically as that segment of the population has grown in number. Many of these patients also take newer antiplatelet or anticoagulant medications, which can increase the likelihood and severity of intracranial hemorrhage after a fall.
Research and clinical care in TBI have been held back by persistent use of categorization based on physical examination instead of on underlying pathophysiology. No one would base a huge infrastructure of research, acute care, and rehabilitation on something as nebulous as “abdominal pain” because that term is so broad as to be almost meaningless. Abdominal pain can be caused by gastric ulcer, appendicitis, ischemic bowel, diverticulitis, pancreatitis, and a host of other diseases, which all have their own causes and treatments. A single medication or other treatment cannot be expected to be effective against such a variety of conditions. But the term “TBI” is used to describe any mechanically induced alteration of neurologic function, regardless of the underlying pathophysiologic cause, such as enlarging extraaxial hematoma, diffuse swelling, ischemia, blossoming contusion, and so on. Applying the same uniform approach to these different conditions makes as little sense as applying a single intervention to all patients with abdominal pain. It is no surprise that clinical trials in TBI, which have adopted this approach to patient enrollment, have failed to demonstrate improved outcome from any proposed intervention.
Both the public health burden of this severe and common disease and the exasperating stubbornness with which it has resisted attempts to develop effective treatments illustrate the magnitude of the challenges posed by TBI. This article focuses on the management of adults with moderate and severe closed brain injuries sustained in a civilian setting. The basic principles of management of severe TBI apply to children as much as to adults, but specific goals and parameters may differ. Also, pediatric TBI is characterized by a lower incidence of traumatic mass lesions than seen in adults. Of course, the possibility of intentionally inflicted injury must always be considered in children, just as it is in elderly and other vulnerable patients. Penetrating brain injuries may present interesting challenges in terms of surgical approaches and techniques, but nonsurgical management has much in common with that of closed TBI patients. Similarly, military TBI is often caused by blast injury, which may produce massive brain swelling and cerebral vasospasm. However, other tenets of management are the same as those for nonblast injuries.
Patient evaluation and management overview
The acute management of moderate and severe TBI is similar and varies primarily in degree of intervention, with the sickest patients requiring and receiving the most aggressive care.
History
Patient evaluation begins with a brief determination of the events surrounding the injury. Although such information is often incomplete and contradictory in the first minutes and hours after injury, it may prove useful for guiding initial management.
Physical Examination
The core of the evaluation is the physical examination. For TBI, as well as other neurologic emergencies, the initial assessment is usually based on the GCS (see Table 1 ).
- •
The 3 components of the GCS are eye opening, verbal function, and motor examination. The score for each component should be listed separately and not lumped into a single overall score.
- •
For the eye opening and motor assessments, the right and left sides should be listed separately.
- •
If a patient’s responses vary during a particular assessment, the highest level of function (best score) should be recorded.
Pupil size and reactivity are also important and should be noted for each eye.
- •
Dilatation and loss of reactivity may indicate that the pupil-constricting nerve fibers on the periphery of the third cranial nerve are significantly compressed by edematous or displaced brain tissue.
- •
Ischemia of the midbrain (where the third nerve arises from the Edinger-Westphal nucleus) may also be a cause.
- •
In a significant percentage of cases, local ocular trauma may be responsible.
- •
Pupillary dilatation and loss of reactivity resulting from extensive intracranial metabolic derangement is an ominous sign.
Completion of even this straightforward neurologic assessment may be impossible if patients have received sedation or paralytics, if one or both eyes are swollen shut, if the arms have sustained orthopedic or vascular injury, or for other reasons. The only recourse in such situations may be to document those parts of the examination that can be performed and to rely on others’ reports (if available) of what the patient was doing initially. A more detailed neurologic assessment can be conducted after more pressing assessments and interventions have been carried out.
Careful initial assessment serves as the baseline against which subsequent improvement or deterioration in neurologic examination will be gauged.
Along with the neurologic assessment, a careful systematic examination is necessary to optimize treatment of non–nervous system injuries and, if necessary, to help balance different treatment priorities.
Prevention of Secondary Insults
Management of TBI patients, especially those at the severe end of the spectrum, is focused on preventing secondary cerebral injury. This fundamental concept is based on the preclinical and clinical observation that the acutely traumatized brain is exquisitely sensitive to even mild deviations from normal homeostasis that would be well-tolerated in the absence of acute injury.
The clinical outcome can be adversely affected by secondary insults. Among the most common are hypotension and hypoxia. Because management of blood pressure and oxygenation is often performed by other specialists besides neurosurgeons, many different types of providers can intervene to prevent and treat these potentially devastating secondary insults.
Another common secondary insult is increased intracranial pressure (ICP). Potential interventions are discussed below. Etiologies can include the following:
- •
Impaired autoregulation with elevated cerebral blood volume (CBV)
- •
Presence or expansion of a large hematoma or contusion
- •
Edema around a cerebral contusion
- •
Hydrocephalus
- •
Diffuse brain swelling with reduced cerebral compliance
- •
Combinations of these and other causes
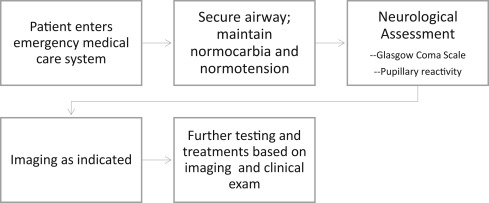
ABCs
As in any medical emergency, the first priority is assessment and stabilization of the ABCs (airway, breathing, and circulation; Fig. 1 ). Counterintuitively, endotracheal intubation has been reported to worsen the outcome in many published series. Many first responders do not perform endotracheal intubation sufficiently often to maintain their skill level in this technique, especially in prehospital environments that often pose a challenge to successful endotracheal intubation. Patients may become hypoxic during prolonged attempts at securing endotracheal access.
For breathing, the goals are simple: provide adequate oxygen to the injured brain and ensure sufficient ventilation to keep arterial carbon dioxide levels within a normal range because an increase in Pa co 2 can lead to dilatation of cerebral arteries, with the consequent increase in CBV leading to an increased ICP. Regardless of whether an endotracheal tube is in place, care must be taken to avoid hyperventilation because hypocarbia can promote cerebral vasoconstriction and subsequent decrease in blood flow to an injured brain, potentially contributing to neuronal death from ischemia.
Deliberate elevation of cerebral perfusion pressure (CPP, derived by subtracting the ICP from the mean arterial pressure) to supranormal levels has been demonstrated not to improve outcomes in severe TBI patients. However, widespread recognition of the deleterious effects of hypotension in TBI patients has caused considerable attention to be placed on maintenance of normal blood pressure and avoidance of hypotension, the goal being not to worsen cerebral hypoperfusion and ischemia. Simply put, there is a floor below which the CPP is generally not allowed to fall, but deliberate elevation of CPP above this level is not beneficial. The Brain Trauma Foundation’s Guidelines for the Management of Severe Traumatic Brain Injury, 3rd edition , specifies that this floor for CPP is 50 mm Hg for most patients, with a target of 50 to 70 mm Hg. In North America, this recommendation is frequently simplified to target a minimum CPP of 60 mm Hg.
Monitoring
All intensive care unit (ICU) patients undergo detailed metabolic monitoring. Unique to neurocritical care is monitoring of parameters reflecting neurologic function. This is most commonly manifest as monitoring of ICP. For several decades, it was recommended widely that certain TBI patients undergo ICP monitoring, including most of those with severe TBI and some with less severe injuries. However, it was widely perceived that ICP monitoring was not being practiced as widely as one might expect. A review of the National Trauma Data Bank found that ICP monitoring was performed in fewer than one-half of patients who met Brain Trauma Foundation guidelines for such monitoring. Moreover, ICP monitoring was associated with a 45% reduction in survival.
A prospective trial to investigate the effect of ICP monitoring on outcome was carried out in several South American countries. The presence of intracranial hypertension in 2 groups of patients was determined either by invasive monitoring or by inference from findings on imaging and clinical examination. The 2 groups did not differ in outcome. This study has been criticized for several reasons, including the less-advanced prehospital emergency medical systems in the locations of the study hospitals when compared with those in high-income countries. Nevertheless, this study has been helpful for questioning a long-held dogma and for opening a discussion about the optimal use of ICP monitoring in TBI patients.
Many other neurologic monitoring technologies are available commercially, both invasive and noninvasive. Although adverse values for the specific parameters measured by these devices have been linked to worse outcomes, it has not been shown that intervention to treat those parameters can improve outcomes. One technology that is further along than most on the pathway toward demonstration of clinical efficacy is brain tissue oxygen monitoring. A phase II trial has suggested some benefit from intervening to correct low brain tissue oxygen levels, and a phase III trial is in the planning stages.
Initial Imaging
After the ABCs have been addressed and an initial evaluation for associated injuries has been completed, patients are usually taken for immediate computed tomography (CT) scanning. Typically, CT scans are obtained of the head, cervical spine, and chest, abdomen, and pelvis, including the thoracic and lumbar spines. Although MRI scanning may provide more detail about the brain parenchyma, it requires much more time than a CT scan. Also, CT scanning is highly sensitive for detecting acute blood, skull fractures, mass effect, and other traumatic pathologies that may require immediate intervention. CT scanning also puts few restrictions on access to an acutely injured patient, unlike MRI scanning. Finally, MRI scanning is not compatible with the ferromagnetic monitoring and therapeutic equipment that often accompanies trauma patients from the emergency department to the CT scanner.
Of note, CT scanning has become so rapid that, even if the head CT demonstrates a large hematoma requiring immediate evacuation, the remainder of the scan (cervical spine and chest, abdomen, and pelvis) can be completed while the operating room makes hurried preparations for an emergency craniotomy. This is time well-spent because the identification of other injuries may affect positioning or other preparations for the craniotomy, or may even require concurrent treatment while the intracranial hematoma is being evacuated.
Although many neurosurgeons have long favored clinically based classification systems like the GCS, it is also possible to classify TBI according to imaging features. Marshall and colleagues used the Traumatic Coma Data Bank to develop a CT-based scheme ( Table 3 ). Maas and colleagues used a large clinical trial database to construct a prognostic scheme in which selected CT features are used to calculate a CT score ( Table 4 ). The trauma surgery community often uses the Abbreviated Injury Scale to classify the severity of TBI, and it is possible to translate Abbreviated Injury Scale data into the appropriate Marshall classification.







