Acute Fractures, Malunions, and Nonunions of the Clavicle
David Ring
Jesse B. Jupiter
D. Ring: Department of Orthopaedic Surgery, Massachusetts General Hospital, Cambridge, Massachusetts.
J. B. Jupiter: Department of Orthopaedic Surgery, Massachusetts General Hospital, Cambridge, Massachusetts.
INTRODUCTION
Recent observations emphasize that nonunion of the clavicle is more common than previously recognized79,175,208,209 and that malunion with shortening can be associated with shoulder dysfunction.15,28,55,56,122,161,209 As a result, primary operative treatment is becoming more commonplace. The indications and techniques of operative treatment are evolving. The operative treatment of nonunion and malunion can also be effective.
PATHOLOGY
Anatomy
The clavicle and scapula link the upper limb with the axial skeleton. The clavicle is linked to the scapula through the strong coracoclavicular and acromioclavicular ligaments. Although it was once believed that the clavicle rotated with respect to the scapula,81,82 experiments involving the insertion of Kirschner wires into awake volunteers have demonstrated that these two bones are tightly linked.61,178 Elevation-depression, protraction-retraction, and rotation of the clavicle through the sternoclavicular articulation are associated with corresponding movements of the scapula with respect to the thorax.
Animals that bear weight on their forelimbs do not have clavicles.10,30,44,110,155,156 The absence of a clavicle improves running and agility on four limbs. In such animals, the scapula is stabilized to the thorax by numerous powerful muscles. Clavicles are present in brachiating animals and apparently serve to help hold the upper limb away from the trunk to enhance more global positioning and use of the limb.
The clavicle has been considered by some to be an expendable bone.73 Although children with congenital absence of the clavicle adapt suprisingly well,58,116 and patients with tumors or infections treated with clavicular resections sometimes function adequately,34,52,72,73,193,212 both have difficulty with overhead activities requiring strength or dexterity. Patients with clavicular resection may also have brachial plexus irritation related to instability of the clavicular fragments. Patients with a trapezius
palsy do particularly poorly without a clavicle.212 The authors believe that the evolutionary process has determined an important function for the clavicle and therefore always strive to preserve its length and alignment.
palsy do particularly poorly without a clavicle.212 The authors believe that the evolutionary process has determined an important function for the clavicle and therefore always strive to preserve its length and alignment.
The clavicle is named for its S-shaped curvature with an apex anterior medially and an apex posterior laterally, resembling the musical symbol clavicula127 (Fig. 19-1). The larger medial curvature widens the space for passage of neurovascular structures from the neck into the upper extremity through the costoclavicular interval. The transition from medial to lateral curvature occurs at approximately two-thirds the length of the bone as measured from its sternal end, a site that corresponds approximately to both the medial limit of attachment of the coracoclavicular ligaments and the entrance point of the main nutrient artery of the clavicle.151
The clavicle is made up of very dense trabecular bone lacking a well-defined medullary canal. In cross-section, the clavicle changes gradually between a flat lateral aspect, a tubular midportion, and an expanded prismatic medial end.6
The clavicle is subcutaneous throughout its length and makes a prominent aesthetic contribution to the contour of the neck and upper chest. The supraclavicular nerves run obliquely across the clavicle just superior to the platysma muscle, and the authors suggest identifying and protecting them during operative exposure to offset the development of hyperesthesia or dysesthesia over the chest wall (Fig. 19-2).
It is not surprising that the middle third is the most common site of clavicular fracture considering that the midportion (1) is the thinnest and narrowest portion of the bone, (2) represents a transitional region of the bone, both in curvature and in cross-sectional anatomy, making it a mechanically weak area, and (3) is the only area of the clavicle that is not supported by ligamentous or muscular attachments. It is possible that this circumstance was selected during evolution because clavicular fracture protects the brachial plexus during difficult births (shoulder dystocia).153
 Figure 19-1 The clavicle is named for its resemblance to the musical symbol, clavicula. This S-curvature and change from flat lateral to round medial shape make internal fixation more difficult. |
The intimate relation of the clavicle to the brachial plexus, to the subclavian artery and vein, and to the apex of the lung, belies the fact that injury to these structures in association with fracture of the clavicle is so uncommon. Brachial plexus palsy may develop weeks or years after injury as a result of hypertrophic callus with or without malalignment of the fracture fragments, leading to compromise of the costoclavicular space.53,80,88,93,119,124,170,182,204,214 Narrowing of the costoclavicular space as a result of malunion or nonunion can also lead to a dynamic narrowing of the thoracic outlet.5,9,20,31,59,11,126,162,195
Shoulder Suspensory Complex
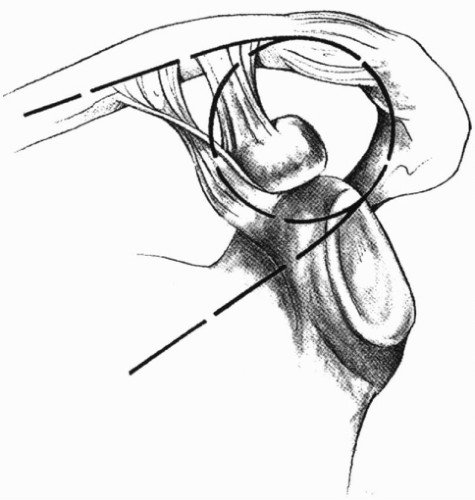
Although the effective treatment of most isolated fractures of the clavicle and scapula is relatively straightforward, combined injuries are regarded as more troublesome and are more readily considered for operative treatment.68,76,108 An anatomic concept that facilitates understanding of these issues is the superior shoulder suspensory complex.68 The complex consists of two struts (the clavicle and the lateral portion of the scapular body) linked by a combined bony and soft tissue ring (Fig. 19-3). The ring is composed of the coracoid process, coracoclavicular ligaments, distal clavicle, acromioclavicular ligaments, acromion, and glenoid process. Disruption of this complex at two sites can be far more problematic than disruption at one site. Common examples of double disruptions include complete acromioclavicular dislocation (e.g., disruption of the coracoclavicular and acromioclavicular ligaments), displaced fracture of the lateral clavicle (i.e., coraclavicular ligament injury and fracture of the distal clavicle), and fracture of the clavicle associated with fracture of the glenoid neck or scapulothoracic
dislocation. Although the role of operative treatment for these injuries is debated, each poses a more substantial risk to shoulder function than injuries that only disrupt one aspect of the shoulder suspensory complex.
dislocation. Although the role of operative treatment for these injuries is debated, each poses a more substantial risk to shoulder function than injuries that only disrupt one aspect of the shoulder suspensory complex.
Consequences of Fracture Malalignment
Some studies suggest a relationship between shortening of the clavicle and shoulder dysfunction.55,56,122,152 Eskola and associates55 evaluated 89 patients 2 years after clavicle fracture injury. Twenty-four (27%) had either slight pain on exercise or restricted shoulder movement, and four had major functional problems. Both primary fracture displacement of more than 15 mm and shortening greater than 15 mm at final follow-up were significantly associated with pain on exercise. It is possible that the shoulder dysfunction is related to the higher energy of the injury rather than the residual malalignment.
In contrast, Nordqvist and colleagues147 evaluated 16 patients with 15 mm or greater shortening of the clavicle and found no measurable effect on mobility, strength, or Constant score. Oroko and colleagues154a found 3 of 13 adults with healed clavicle fractures with 15 mm or greater shortening had diminished Constant scores, but in each case the disability was explained by factors other than the shortening.
The authors believe that shortening of the clavicle may affect shoulder function in ways that are difficult to quantify and is probably only important in patients who place substantial demands on their shoulders.
Classification and Epidemiology
The traditional division of the clavicle into thirds1,136,137,180 seems arbitrary given that most fractures occur near the junction of the middle and distal thirds.198 Other authors have suggested division of the clavicle into fifths with the middle three-fifths representing midclavicular fractures and the lateral one-fifth representing distal clavicular fractures.175 The use of fractional divisions may not adequately distinguish fractures from injury to the coraclavicular ligaments.
Neer136 defined fractures of the lateral clavicle as lateral to the medial limit of the trapezoid ligament. He distinguished fractures of the distal clavicle with intact coracoclavicular ligaments (type 1) from those associated with tearing of these ligaments with wide displacement of the fracture fragments (type 2).136 The wide displacement and instability of type 2 fractures place them at greater risk of nonunion. Intra-articular fractures (type 3) are rarely diagnosed acutely and were introduced into the classification in an attempt to explain later arthrosis or osteolysis.36,135, 136 and 137
Rockwood’s176,177 distinction of distal third fractures with intact (type IIA) or disrupted (type IIB) coracoclavicular ligaments is confusing because there is no clear distinction between type IIA fractures and more distal midclavicle fractures.
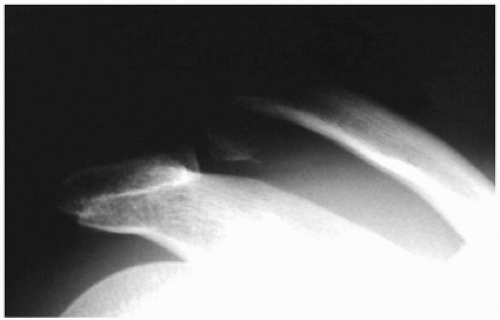
It may be most useful to restrict the term “lateral clavicle fracture” to very far lateral fractures. These are essentially an alternative to an acromioclavicular dislocation in which the coracoclavicular ligaments tear but the acromioclavicular ligaments remain intact, the failure occurring through the distal clavicle instead (Fig. 19-4).
In unusual instances, fractures of the distal clavicle may be unstable in the absence of ligamentous injury. This occurs when both of the coracoclavicular ligaments remain attached to an inferior fracture fragment that lacks attachment to either of the primary medial or lateral fragments.158
Fractures of the medial end of the clavicle are uncommon and almost without exception are treated symptomatically. Craig36 subdivided these as minimally displaced (type I), displaced (type II), intra-articular (type III), physeal separation (type IV), and comminuted (type V) fractures. Fractures in this region of the clavicle are so uncommon that the patterns of medial clavicular injury have rarely been described and studied, and it remains unclear how different fracture patterns influence treatment and prognosis.
Robinson175 reviewed 1,000 fractures of the clavicle treated at the Royal Infirmary of Edinburgh over a 6-year period. He divided the clavicle into fifths, labeling the medial one-fifth as type I or medial clavicle fractures, the lateral one-fifth as type 3 or lateral clavicle fractures, and the middle three-fifths as midclavicular fractures (type 2). For midclavicular fractures he applied subclassifications that distinguished displacement greater than the width of the bone and segmental comminution of the fracture fragments. For medial and lateral clavicle fractures he distinguished displacement and articular involvement. He reported the following interesting facts: the incidence of medial clavicle fractures was 1 per 100,000 per year compared with 20 for midclavicular and 8 for lateral clavicular fractures; the midclavicular fractures were more often displaced than not by a ratio of 2.7 to 1; and the lateral clavicle fractures were more often nondisplaced by a ratio of approximately 2 to 1. Ten percent of displaced midclavicular fractures had delayed or arrested healing, and 6% were treated operatively. None of the nondisplaced fractures had healing problems. Segmental comminution of the fracture was also a risk factor for nonunion with 5% of noncomminuted fractures failing to heal, compared with 11.5% of comminuted fractures. Forty-four percent of displaced lateral clavicle fractures had healing problems, and 14% were treated operatively.
Other recent studies of the epidemiology of clavicle fractures found an incidence closer to 50 per 100,000 per year and suggest that lateral clavicle fractures are increasingly common among the elderly who have a simple fall from a standing height.143,149,175 In another study, two-thirds of patients with a lateral clavicle fracture were alcoholics.144
Mechanism
In adolescents and adults, clavicle fractures in all regions typically result from moderate or high-energy traumatic impacts, such as those caused by a fall from a height, a motor vehicle accident, a sports injury, a blow to the point of the shoulder, or, rarely, a direct injury to the clavicle.143,149,175 In elderly persons, clavicle fractures usually result from low-energy trauma such as a simple fall.
It has become clear that the clavicle fails most commonly in compression.11,63,186,194 Failure in compression is seen after falls onto the shoulder and direct blows to the point of the shoulder. A direct blow to the clavicle, which can occur in sports in which sticks are wielded (e.g., lacrosse191), may also fracture the clavicle. Although a fall onto the outstretched hand has traditionally been considered a common mechanism of midclavicular fracture,1 recent observations question this assumption.194
Stanley and colleagues194 studied 122 of 150 consecutive patients with fractured clavicles who presented to two hospitals in Sheffield and provided detailed accounts of their injury. Eighty-seven percent resulted from a fall onto the shoulder, 7% resulted from a direct blow to the point of the shoulder, and 6% resulted from a fall onto an outstretched hand. A fall on the outstretched hand was the apparent mechanism of 5 (6.3%) of 79 midclavicular fractures and 2 (5.9%) of 34 distal clavicular fractures, suggesting that a direct injury to the shoulder is the most common mechanism of clavicular fracture at all sites. These authors hypothesized that even those patients who recall their injury as a fall onto the outstretched hand may have fallen secondarily onto the shoulder. This second impact may have been the injuring force, and an isolated fall onto the outstretched hand may actually be an unusual mechanism of injury.194
EVALUATION
Clinical Evaluation
Diagnosis is usually straightforward based on the mechanism of injury, the location of swelling and ecchymosis, and the examination for deformity, tenderness, and crepitation. Open clavicle fractures are uncommon, even after high-energy traumatic injury, and usually the result of a direct blow to the clavicle. Tenting of the skin by one of the major fracture fragments or by an intervening fragment of comminuted bone is not uncommon, but a true threat to the integrity of the skin is unusual.169,175
Neurovascular injury,80 pneumothorax,42,112,123,214 and hemothorax180 have been reported in association with fracture of the clavicle but are uncommon. In contrast with late dysfunction of the brachial plexus after clavicular fracture, in which medial cord structures are typically involved, acute injury to the brachial plexus at the time of clavicular fracture usually takes the form of a traction injury to the upper cervical roots. Such root traction injuries usually occur in the setting of high-energy trauma and have a relatively poor prognosis.8,106,189
The prevalence of pneumothorax in association with fracture of the clavicle is 3%, based on Rowe’s study of more than 600 fractures at Massachusetts General Hospital.180 In that study, Rowe did not distinguish between moderate and high-energy injuries, nor did he distinguish isolated fractures from those injuries associated with ipsilateral scapular fracture or dissociation from the thorax or with ipsilateral upper rib injuries. The presence of these associated injuries indicates an injury mechanism of
extremely high energy.45,47,76,102,108,172,207 Pneumothorax and hemothorax are more common in this situation and more likely to result from a generalized chest wall injury than from a direct injury to the apical pleura by the fractured clavicle.42,112,123,214 Nonetheless, evaluation for possible pneumothorax by physical examination and close inspection of an upright film that includes the ipsilateral upper lung field is important.
extremely high energy.45,47,76,102,108,172,207 Pneumothorax and hemothorax are more common in this situation and more likely to result from a generalized chest wall injury than from a direct injury to the apical pleura by the fractured clavicle.42,112,123,214 Nonetheless, evaluation for possible pneumothorax by physical examination and close inspection of an upright film that includes the ipsilateral upper lung field is important.
When a clavicle fracture occurs because of a high-energy traumatic injury (e.g., motor vehicle accident or fall from a height), then the evaluation of life-threatening lesions takes precedence. Major vascular disruption can occur in association with fracture of the clavicle, but it is extremely rare.35,40,41,43,71,80,84,118,120,133,148,159,196 Injury to the thoracic duct has also been reported. Death after a tear of the subclavian vein with resultant pseudoaneurysm was recorded in the famous case of the death of Sir Robert Peel.41,101 Arterial thrombosis may occur after intimal injury.83,105,202 Most vascular injuries associated with clavicle fractures occur in combination with a scapulothoracic dissociation, which has been compared with a closed forequarter amputation.45,47,102,154,181
Evaluation of the vascular status of the upper extremity should include an assessment of relative temperature and color compared with the uninvolved extremity. Because of the extensive collateral blood supply to the upper extremity, these factors may appear normal despite the presence of a major vascular injury. A difference in peripheral pulses or blood pressure between injured and uninjured upper extremities may be the only clue that a vascular injury is present. If the limb is threatened or there is persistent unexplained hemorrhage, angiography can help to detect and localize any vascular injury and thereby assist with definitive management.
Radiographic Evaluation
An anteroposterior (AP) view of the clavicle identifies and localizes most clavicular fractures, and it should differentiate displaced from nondisplaced or minimally displaced fractures. The radiographic film should be large enough to evaluate both the acromioclavicular and the sternoclavicular joints as well as the remainder of the shoulder girdle and upper lung fields.180 Oblique views can be used to further gauge the degree and direction of displacement.180,167 Quesada recommended 45-degree caudad and cephalad views, which he believed would facilitate evaluation by providing orthogonal projection.167 In practice, a single 20- to 60-degree cephalad-tilted view provides an adequate second view, because interference with thoracic structures is minimized. Medial clavicular fractures may be difficult to characterize on this view, and computed tomography is often necessary.
Evaluation of distal clavicular fracture displacement in the AP plane requires a different set of radiographs, because cephalad-tilted and caudad-tilted views are hindered by overlap of the bones of the shoulder and overexposure of the distal clavicle and often fail to accurately depict the degree of displacement. Neer135 suggested a stress view (with 10 lb of weight in each hand) to evaluate the integrity of the coracoclavicular ligaments and 45-degree anterior and posterior oblique views to gauge displacement.
A combination of both AP and cephalad-caudad obliquity has been advocated in the evaluation of midclavicular fractures.171,206 The so-called apical oblique view (tilted 45 degrees anterior and 20 degrees cephalad) may facilitate the diagnosis of minimally displaced fractures (e.g., birth fractures and fractures in children).206 Ultrasound is also a sensitive diagnostic tool in the evaluation of birth fractures.91
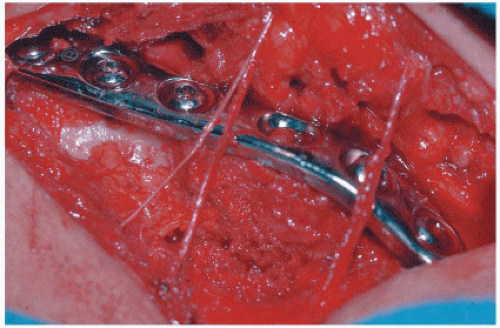
The abduction lordotic view, taken with the shoulder abducted above 135 degrees and the central ray angled 25 degrees cephalad, is useful in evaluating the clavicle after internal fixation.171 The abduction of the shoulder results in rotation of the clavicle on its longitudinal axis, which causes the plate to rotate superiorly and thereby expose the shaft of the clavicle and the fracture site under the plate.
ACUTE FRACTURES
Nonoperative Treatment
Closed reduction of clavicle fractures is rarely attempted because the reduction is usually unstable and there are no reliable means for providing external support. The reduction maneuvers described resemble those used for sternoclavicular joint dislocations.21,33,157,168,201
Of the many appliances that have been devised in an attempt to effect or maintain closed reduction and thereby minimize the deformity associated with fracture of the clavicle, most have proved to be cumbersome, painful, and even dangerous.142 Dupuytren in 183143 and Malgaigne in 1859113 argued that deformity of the clavicle was inevitable and emphasized the use of the simplest and most comfortable method of treatment; for Dupuytren, this consisted of placing the arm on a pillow until healing occurred.43
Nonetheless, devices intended for the maintenance of reduction and immobilization of clavicle fractures have remained popular and commonly take the form of either a figure-of-eight bandage, with or without a sling and, on rare occasions, a figure-of-eight plaster (Billington yoke13) or a shoulder spica cast.1,157,168,180 Those who agree with Dupuytren and Malgaigne, that accurate reduction and immobilization of clavicular fractures is, as stated by Mullick, “neither essential nor possible,”63,64,103,107,130,187 advocate the use of a simple sling for comfort, forgoing any attempts at reduction.
The advantage of the figure-of-eight bandage is that the arm remains free and can be used to a limited degree.
Disadvantages include the following: increased discomfort2,63,64; the need for frequent readjustment and repeat office visits2,121; the potential for complications, including axillary pressure sores121,163 and other skin problems2; upper extremity edema and venous congestion2,121,130; brachial plexus palsy186; worsening of deformity63,121,130; and perhaps an increased risk of nonunion.210
Disadvantages include the following: increased discomfort2,63,64; the need for frequent readjustment and repeat office visits2,121; the potential for complications, including axillary pressure sores121,163 and other skin problems2; upper extremity edema and venous congestion2,121,130; brachial plexus palsy186; worsening of deformity63,121,130; and perhaps an increased risk of nonunion.210
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree