Acquired Vitamin D Deficiency
Pauline M. Camacho
Epidemiology
This chapter focuses on acquired vitamin D deficiency among adults. The prevalence of this condition has been reported to be as high as 30% to 54% among homebound elderly patients [1], 57% among inpatients [2], and 14% among the general population [3]. There is a seasonal variation, and latitude plays a role in the prevalence of the disease [4], with a higher prevalence in colder countries. However, it appears that even in sunny countries, it is still highly prevalent [5]. In populations of ambulatory patients referred to bone centers, the prevalence of vitamin D deficiency was not particularly higher than described in other populations, 54% when less than 30 ng/mL is used as cutoff, and 39% in another study that used less than 15 ng/mL [6,7].
Definition
The definition of vitamin D has evolved in the past few years, as the assays for 25-OHD have advanced. Vitamin D adequacy is defined as 25-OHD level above 30 ng/mL. This level was found to be the critical level, below which secondary hyperparathyroidism develops [3]. Various groups have proposed nomenclatures for stratifying patients based on 25-OHD levels. Individuals with levels below 30 but above 20 ng/mL are considered to have vitamin D inadequacy or mild vitamin D deficiency. Below 20 ng/mL but above 10 ng/mL is moderate vitamin D deficiency, and below 10 ng/mL is severe vitamin D deficiency. It is important to consider the possibility of
osteomalacia among those with moderate and severe vitamin D deficiency, as these individuals should not be candidates for antiresorptive or anabolic therapy. Severe vitamin D deficiency is usually associated with secondary hyperparathyroidism, hypocalcemia, hypophosphatemia, and in cases of osteomalacia, elevation in bone or total alkaline phosphatase. Patients with mild vitamin D deficiency, particularly those with levels in the mid or high 20s, may have normal parathyroid hormone (PTH) levels.
osteomalacia among those with moderate and severe vitamin D deficiency, as these individuals should not be candidates for antiresorptive or anabolic therapy. Severe vitamin D deficiency is usually associated with secondary hyperparathyroidism, hypocalcemia, hypophosphatemia, and in cases of osteomalacia, elevation in bone or total alkaline phosphatase. Patients with mild vitamin D deficiency, particularly those with levels in the mid or high 20s, may have normal parathyroid hormone (PTH) levels.
Vitamin D Metabolism
Vitamin D refers to either D2 or D3, two forms of the vitamin that are utilized by the human body. Vitamin D2 comes from plants and yeasts, whereas vitamin D3 is synthesized in the skin through the action of sunlight and is found in food sources such as fish and cod liver oil. The potency of vitamin D2 is approximately one-third that of vitamin D3 [8].
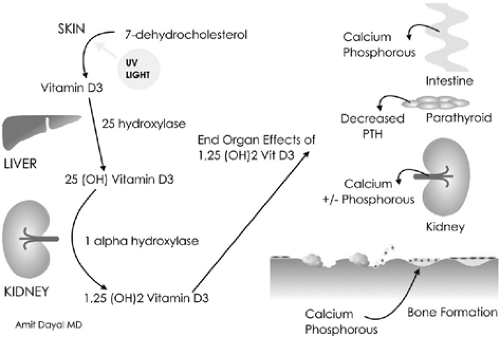
Synthesis of vitamin D starts with the conversion of cutaneous 7-dehydrocholesterol (provitamin D3) to previtamin D3 through exposure to sunlight (Fig. 7.1). Previtamin D3 is then rapidly isomerized to vitamin D3, which then travels in the circulation, bound to vitamin D–binding protein (DBP). This is transported to the liver where it undergoes 25-hydroxylation to form 25-hydroxyvitamin D (25-OHD). This is the major circulating and storage form of vitamin D in the body. An increase in the vitamin D precursors (such as with increased oral intake or sunlight exposure) quickly manifests as an
increase in 25-OHD; thus measurement of its concentration is the ideal test for vitamin D adequacy.
increase in 25-OHD; thus measurement of its concentration is the ideal test for vitamin D adequacy.
After hydroxylation in the liver, 25-OHD is then transported to the kidneys where 1α-hydroxylase converts 25-OHD to the final, and active, form, 1-25 dihydroxyvitamin D (1-25-OHD). This appears to be the major vitamin D metabolite that exerts effects on bone and calcium homeostasis.
Effects of Vitamin D Deficiency on Calcium Homeostasis
When vitamin D is deficient, gut absorption of calcium decreases, leading to diminished total body calcium stores and subsequent increase in PTH secretion. PTH increases the activity of 1α-hydroxylase, which drives the activation of 25-OHD to 1-25-OHD. Therefore, in states of vitamin D deficiency, 1-25-OHD concentrations can be low, normal, or high. With mild-to-moderate deficiency and in the absence of renal insufficiency, 1-25-OHD is high. Increased 1-25-OHD improves absorption of calcium in the gut, and to a much smaller degree, increases osteoclastic activity. This effect on intestinal calcium absorption, in conjunction with the activation of osteoclastic activity by PTH, restores calcium equilibrium. The mechanism is tightly regulated, and is the reason why only in severe states of vitamin D deficiency do we see low serum total or ionized calcium levels. Serum calcium is often normal in mild-to-moderate vitamin D deficiency. Decreased urinary calcium is one of the earlier compensatory mechanisms, and thus hypocalciuria is often seen.
Pleotropic Effects of Vitamin D
The effects of vitamin D extend beyond the skeletal system. Vitamin D receptors are found in most organ systems, such as the heart, muscles, nervous system, breast, pancreas, colon, and gonads. A correlation between vitamin D and various disease states such as autoimmune diseases—multiple sclerosis, type 1 diabetes, psoriasis, rheumatoid arthritis, inflammatory bowel disease—has been reported. In addition, vitamin D appears to influence blood pressure control through its effects on the renin-angiotensin system. Reports of correlations between vitamin D and myocardial function have also been published. The antiproliferative effects of 1-25-OHD are well known and utilized in the treatment of psoriasis.
Clinical Conditions that Cause Vitamin D Deficiency
Malabsorption
Various conditions, such as inflammatory bowel disease, celiac sprue, pancreatic insufficiency, biliary disease, and short bowel syndrome, can lead to decreased absorption of both calcium and vitamin D from the gastrointestinal tract. The biochemical manifestations include a low serum 25-OHD, high PTH, low urinary calcium excretion, low phosphorus, and in severe cases low ionized or total calcium. When the condition is not treated, osteomalacia may
result (see following discussion) and an elevation of bone-specific and total alkaline phosphatase can be seen.
result (see following discussion) and an elevation of bone-specific and total alkaline phosphatase can be seen.
Renal Insufficiency
As kidney function declines, there is decreased production of 1-25-OHD. Phosphate levels are usually in the high or high-normal range due to diminished urinary excretion. Both of these lead to secondary hyperparathyroidism. Biochemically, 25-OHD and 1-25-OHD levels are usually low, intact PTH levels high, phosphate high, and in severe cases, ionized and total calcium levels low.
Medication Use
Antiseizure medications increase the hepatic catabolism of both 25-OHD and 1-25-OHD, leading to low 25-OHD, high PTH, and sometimes biochemical evidence of osteomalacia. Glucocorticoids and rifampin affect vitamin D metabolism in a similar way.
Vitamin D Deficiency and Fractures
In the postfracture population, numerous studies from all over the world have documented high rates of vitamin D deficiency, ranging from 50% to as high as 90% [9,10,11,12,13,14,15]. Mean vitamin D levels have been consistently lower in the fracture patients in these studies. The effects of vitamin D on calcium and bone metabolism have been discussed here, but in addition, vitamin D deficiency leads to muscle weakness, which increases the risk of falls. In one study, muscle biopsies were done on individuals who suffered hip fractures. The patients were divided into two groups, vitamin D–deficient group (25-OHD >-39 nmol/L) and normal group. The mean type II fiber diameter in the deficient group (15.4 ± 4.2 μm) was significantly smaller than that in the sufficient group (38.7 ± 8.1 μm) (p < 0.0001). A significant correlation between the mean type II fiber diameter with the serum 25-OHD concentration (r = 0.714, p = 0.0011) was seen [16]. It is possible that both inactivity and vitamin D deficiency led to the severe atrophy seen in the vitamin D–deficient group.
After a comprehensive review of calcium/vitamin D trials in the literature, one paper concluded that vitamin D alone was not able to prevent vertebral and nonvertebral fractures, but a marginal effect on fracture risk was seen on hip fractures (seven trials, 10,376 participants; RR, 0.81; 95% CI, 0.68–0.96), and nonvertebral fractures (seven trials, 10,376 participants; RR, 0.87; 95% CI, 0.78–0.97); but there was no evidence showing a significant reduction in vertebral fractures with vitamin D and calcium [17]. A metaanalysis, however, showed more robust fracture reduction, a reduction of 36% in the incidence of vertebral fractures (RR, 0.63; 95% CI, 0.45–0.88; p < 0.01) and a trend toward reduced incidence of nonvertebral fractures (RR, 0.77; 95% CI, 0.57–1.04; p = 0.09) [18].
In another study conducted in Italy, in which women older than 65 years were given 400,000 IU oral vitamin D2 during the winter months of 2000 through 2002, the age-adjusted risk reduction of hip fracture during 2001
and 2002 decreased by 17% (p = 0.056) and 25% (p = 0.005), respectively [19]. A study conducted in the United States offered 1,000 mg of elemental calcium as calcium carbonate and 400 IU (10 μg) of vitamin D3 to a total of 4,957 participants (with 50% participation). A 16% reduction in fracture incidence rate (RR, 0.84; CI, 0.72–0.98; p < 0.025) was seen [20].
and 2002 decreased by 17% (p = 0.056) and 25% (p = 0.005), respectively [19]. A study conducted in the United States offered 1,000 mg of elemental calcium as calcium carbonate and 400 IU (10 μg) of vitamin D3 to a total of 4,957 participants (with 50% participation). A 16% reduction in fracture incidence rate (RR, 0.84; CI, 0.72–0.98; p < 0.025) was seen [20].
The common element among these trials is that only a small-to-moderate dose of vitamin D was administered, and it is unclear whether these amounts actually corrected the deficiency. Furthermore, we suspect that when moderate-to-severe vitamin D deficiency is treated with therapeutic doses of vitamin D, such that the 25-OHD levels are brought up to the goal of 30 ng/mL, secondary hyperparathyroidism resolves, and any baseline hypocalciuria is corrected, the effect on fracture risk will be much higher than what has been reported.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree