Abstract
Objective
By proposing a new terminology (acquired deforming hypertonia or ADH) and a new definition for contractures, the main objective of this study was to establish their prevalence among institutionalized elderly patients. Secondary objectives were to analyze the negative impact of ADH and collect the opinions of clinicians on the possible treatments available.
Methodology
A multicenter cross-sectional study was conducted among residents of 39 geriatric institutions (29 EHPAD and 10 USLD). All subjects presenting at least one ADH were surveyed over a one-week period.
Results
Among 3145 observed patients (mean age 88.9 ± 9.7 years) 22% ( n = 692) presented at least one ADH. In average, each patient presented 4.4 ± 3.2 ADHs. Negative consequences on self-care, nursing and difficulties in getting dressed were most frequently observed. Only 25.4% of clinicians considered the ADH to be potentially reversible. Physical therapy was the therapeutic option most frequently chosen over medication and surgery.
Conclusion
This study confirms the important prevalence of ADH among elderly institutionalized patients. Consequences on the level of dependence were significant. It seems relevant to elaborate hierarchical therapeutic strategies in order to counter these disorders and the fatalism that ensues.
Résumé
Objectif
En proposant une nouvelle terminologie (hypertonie déformante acquise ou HDA) et une nouvelle définition des rétractions tendineuses, l’objectif principal de cette étude était de déterminer leur prévalence dans une population de sujets âgés institutionnalisés. Les objectifs secondaires étaient d’analyser leur retentissement et de recueillir l’avis des médecins sur les traitements envisageables.
Méthode
Une enquête observationnelle transversale multicentrique a été réalisée auprès des résidents de 39 institutions gériatriques (29 EHPAD et 10 USLD). Tous les sujets présentant au moins une HDA ont été recensé de manière exhaustive, sur une semaine donnée.
Résultats
Parmi les 3145 personnes examinées (âge moyen : 88,9 ± 9,7 ans), 22 % ( n = 692) présentaient au moins une HDA. En moyenne, chaque patient présentait 4,4 ± 3,2 HDA. Le retentissement négatif sur les soins d’hygiène, le nursing et les difficultés d’habillage étaient les plus souvent rapportés. Seulement 25,4 % des médecins estimaient que les HDA observées étaient réversibles. Comme moyen thérapeutique, les traitements physiques étaient le plus souvent évoqués devant les traitements médicamenteux et la chirurgie.
Conclusion
Cette étude confirme la forte prévalence des HDA chez les patients âgés institutionnalisés. Les conséquences sur niveau de dépendance sont importantes. L’établissement d’une stratégie thérapeutique hiérarchisée paraît nécessaire pour lutter efficacement contre ces troubles.
1
English version
The rise in life expectancy in industrialized countries induces a considerable increase in the population of older people, including the most elderly ones. In France, about 10% of older persons aged 75 and over, i.e. more than 550,000 persons, live in an institution (mostly EHPAD: nursing homes for dependent elderly populations and USLD: long-term care units).
Social/family isolation and loss of independence in daily living activities (DLA) are the main reasons leading to institutionalization.
Loss of independence is caused by several factors and associates the effects of physiological aging to concomitant pathologies further limiting DLA. Alzheimer’s disease and its associated disorders, ischemic and hemorrhagic stroke, extrapyramidal diseases, degenerative pathologies of the locomotor system, diabetes and its vascular and neurological complications are the main pathologies increasing a person’s dependence level. In the French HID study conducted between 1998 and 1999, the number of dependent elderly subjects confined to a bed or a wheelchair was 225,000 out of those 120,000 lived in an institution. In 2007, more than half of the residents in French geriatric institutions were considered highly dependent [Iso-Resource Groups (IRG) 1 or 2] .
In this population, loss of autonomy is ineluctably associated to decreased mobility, which is at the same time the cause and consequence of functional degeneration. The latter combined to motor, joint or periarticular disorders promote the development of abnormal postures or joint deformities affecting the upper and lower limbs. These disorders will progressively set-in in the absence of proper care. The terms “contractures” or “tendon retractions” have often been used to describe this phenomenon. However, no standard definition has validated these terms . Even though the decrease in joint range of motion (ROM) remains the most commonly reported clinical characteristic, histopathological mechanisms behind the various definitions are quite heterogeneous. For some authors, the origin of contractures can be linked to disorders of the intra-articular or extra-articular tissues , whereas for others, contractures are necessarily the result of changes in periarticular structures especially in myotendinous junctions . Katalinic et al. added another clinical characteristic to decreased joint ROM: increased resistance to passive movements, without identifying its origin.
Usually, the functional impact of these contractures is not accounted for in the proposed definitions . However, this impact is often quite important and represents a source of daily concern for healthcare professionals in geriatric institutions. These contractures are often the cause of spontaneous pain, or pain triggered by daily nursing care acts. They can also be responsible for skin complications (macerations, mycoses, wounds and pressure ulcers) that provide additional pain and discomfort. Joint contractions can aggravate limitations in all daily living activities (ADL). Contractures to the lower limbs can prevent elderly subjects from sitting in a chair and thus they end up confined to a bed, which is often fatal in this population. Finally, the subsequent increased level of care triggers additional healthcare costs for these dependent patients.
Thus, the lack of definition and nosological framework for contractures and deformities in elderly subjects explains the high variability of epidemiological, therapeutic or preventive data available on this subject .
By proposing a new definition for these disorders, grouped under the term acquired deforming hypertonia (ADH), the main objective of this study was to determine its prevalence in elderly populations living in institutions.
Secondary objectives were to analyze the impact of ADH and collect the opinion of evaluating clinicians on the reversible nature of these deformities and the different therapeutic options available.
1.1
Methods
1.1.1
Study type
This was a national, observational, multicenter cross-sectional study.
1.1.2
Population
All residents of 39 geriatric institutions (29 EHPAD and 10 USLD) spread out over 6 French regions (Aquitaine, Île-de-France, Languedoc-Roussillon, Nord Pas-de-Calais, Provence-Alpes-Côte d’Azur, Rhône-Alpes) were included in this study.
1.1.3
Data collection
After explaining the project and delivering a quick training to define the parameters of ADH, the clinician coordinators from the various participating institutions were invited, in partnership with the healthcare staff, to identify in an exhaustive manner, all patients presenting one or more ADH locations, this over a 1-week period.
ADH was defined as any joint deformity with decreased ROM and increased resistance to passive movements, regardless of its cause, which promotes functional impairments, discomfort or any other limitation in activities of daily living.
The ADH cases analyzed in this study only concerned the limbs and were described in observational notebooks and associated to pictures ( Fig. 1 ).
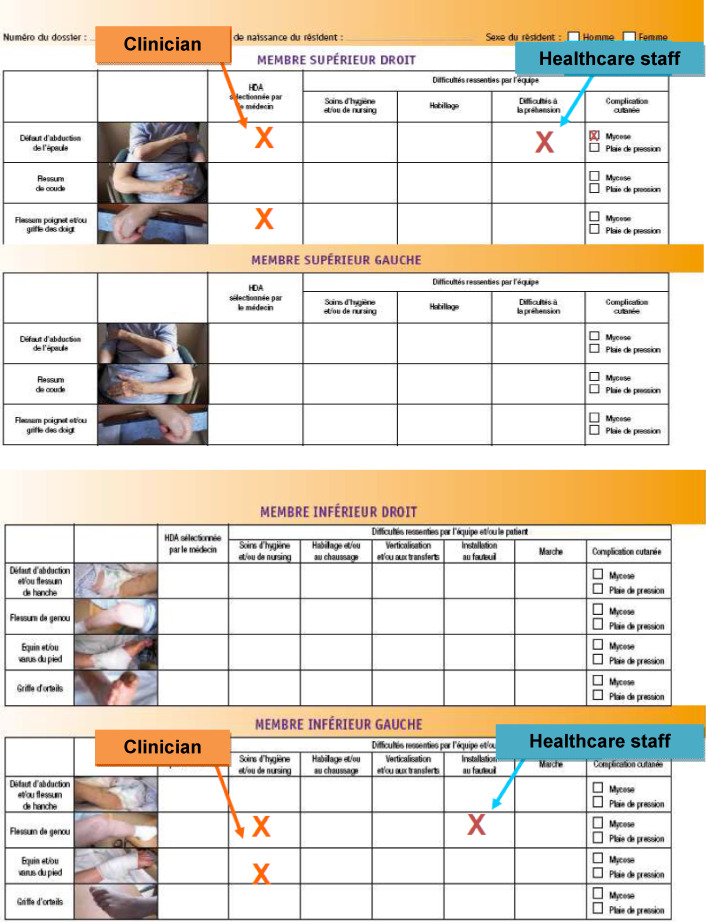
For the upper limbs, ADH cases consisted in: contractures of shoulder adductors, elbow flexion contracture and claw fingers. For lower limbs, the cases were: defect in hip abduction, hip flexion contracture, knee flexion contracture, equinus and varus deformities of the foot and claw toes. The staff also recorded the number of ADH cases, locations as well as their unilateral or bilateral nature. Furthermore, the team had to appreciate the impact of these ADHs. For the upper limbs, the staff noted the presence of grasping difficulties directly related to the ADHs, difficulties in self-care and nursing, in getting dressed as well as skin complications (mycoses, pressure ulcers). For the lower limbs, they recorded: the presence of gait and/or transfer difficulties directly related to ADH, difficulties in self-care and nursing, in getting dressed or putting on shoes, transferring from bed into a chair as well as skin complications (mycoses, pressure ulcers).
The residents’ age and gender were also collected at the time of the study as well as the GMP (weighted average IRG) of each institution. The latter is useful to appreciate the mean level of dependence of the residents for each institution. The higher the level of dependence the higher the GMP was (maximum 1000).
Finally, clinicians had to indicate for each patient if they thought that the diagnosed ADH was reversible or not and if a physical (e.g. physical therapy, occupational therapy, orthoses), medical or surgical treatment could be proposed.
1.1.4
Statistical analyses
A descriptive analysis (according to the different parameters: distribution, mean and standard deviations) was conducted. The Student t -test was used to compare the means of quantitative variables (age, mean GMP of the institutions). Pearson’s r coefficient was computed to analyze the correlation level between the number of ADHs and the number of difficulties reported by the healthcare teams. All these statistics were computed with the SPPS software version 10.
1.2
Results
Among the 3145 patients observed in the study, 692 of them (22%) presented at least one ADH. Mean age of this population was 88.9 years (± 9.7 years). Women represented 75.2% of all cases.
Residents in USLD had more ADHs than those in EHPAD (25.6% vs. 20.2% respectively; P < 0.001). Mean age for patients with ADH did not differ according to the type of institution (89.5 ± 11 years for patients in USLD setting vs. 88.6 ± 8.9 years for patients in EHPAD setting; P = 0.24). The mean level of dependence, assessed by the GMP, was significantly higher in USLD than EHPAD settings (854.1 ± 26.2 vs. 709.2 ± 91.6, respectively; P < 0.001). Among these 692 patients, only 14.2% of them ( n = 98) had one single ADH. On average, each patient had 4.4 ± 3.2 different ADHs (median: 4) at the time of the study.
Over one-third of patients (34.6%) had more than 5 ADH locations. In 68.5% of cases, at least one of the upper limbs was affected and in more than 80% of cases at least one of the lower limbs was affected ( Table 1 ).
| Unilateral | Bilateral | Total % ( n = 692) | |
|---|---|---|---|
| Affections of the upper limbs (overall) | 30.6 (212) | 37.9 (262) | 68.5 (474) |
| Defect in shoulder abduction | 15.5 (107) | 23.8 (165) | 39.3 (272) |
| Elbow flessum | 21.1 (146) | 25.0 (173) | 46.1 (319) |
| Wrist flessum or claw fingers | 21 (145) | 19.9 (138) | 40.9 (283) |
| Affections of the lower limbs (overall) | 24.6 (170) | 55.5 (384) | 80.1 (554) |
| Defect in hip abduction and/or hip flessum | 11 (76) | 29.1 (201) | 40.0 (277) |
| Knee flessum | 19 (131) | 36.1 (250) | 55.1 (381) |
| Equinus and/or varus deformity of the foot | 17.6 (122) | 19.7 (136) | 37.3 (258) |
| Claw toes | 5.9 (41) | 10.3 (71) | 16.2 (112) |
In 67.3% of cases the patients presented bilateral ADHs (regardless of the affected limb) and for 187 patients (27%) the four limbs were affected.
ADH types were quite homogenously distributed for the upper limbs ( Table 1 ). For the lower limbs, ADH of the knee flexors was most frequently reported and concerned more than half the patients, whereas claw toe was the least frequently reported (16.2%). This deformity of the toes was associated with equinus and/or varus deformities of the foot in more than 53% of cases.
Regarding the impact of ADH, evaluated by the healthcare teams, the presence of one or more deformities was the cause of at least one of the difficulties listed, in 82.7% of cases when the affection concerned the upper limbs and in 83% of cases when it concerned the lower limbs.
For the upper limbs, the negative impact on self-care, nursing and getting dressed was most often noted ( Table 2 ). Regarding the lower limbs, difficulties in getting dressed and putting on shoes as well as getting up preceded the negative impact on self-care and nursing expect for contractures to hip adductors, where difficulties in self-care were the most reported consequences. Overall, skin complications (pressure ulcers, mycoses) were less frequent for the upper and lower limbs. Nevertheless, skin complications were more reported for distal locations (contractures of the wrist flexors, claw fingers or toes) than proximal ones (contractures of the hip or shoulder adductors). The proximal contractures were noted as triggering difficulties in self-care, nursing or getting dressed.
| Shoulder adductum ( n = 272) | Elbow flessum ( n = 319) | Wrist flessum/claw fingers ( n = 283) | |
|---|---|---|---|
| Type of negative consequence | |||
| Self-care and/or nursing | 78.3 (213) | 67.7 (216) | 70.7 (200) |
| Getting dressed | 83.5 (227) | 76.5 (244) | 68.2 (193) |
| Grasping difficulties | 58.8 (160) | 58.6 (187) | 73.5 (208) |
| Skin complications | 12.5 (34) | 14.1 (45) | 19.8 (56) |
| Mycoses | 8.8 (24) | 10.7 (34) | 14.5 (41) |
| Pressure ulcer | 4.4 (12) | 4.4 (14) | 6.4 (18) |
| Hip adductum flessum ( n = 277) | Knee flessum ( n = 381) | Foot equinus varus ( n = 258) | Claw toes ( n = 112) | |
|---|---|---|---|---|
| Type of negative consequence | ||||
| Self-care and/or nursing | 72.9 (202) | 59.3 (226) | 48.5 (125) | 44.6 (50) |
| Getting dressed/putting on shoes | 70.4 (195) | 60.1 (229) | 69.0 (178) | 77.7 (87) |
| Verticalization and/or transfers | 67.9 (188) | 64.0 (244) | 60.1 (155) | 53.6 (60) |
| Settling into a chair | 57.0 (158) | 49.3 (188) | 46.1 (119) | 40.2 (45) |
| Gait difficulties | 55.6 (154) | 52.2 (199) | 50.0 (129) | 43.8 (49) |
| Skin complications | 18.8 (52) | 14.4 (55) | 17.8 (46) | 27.7 (31) |
| Mycoses | 7.9 (22) | 5.5 (21) | 3.9 (10) | 6.3 (7) |
| Pressure ulcer | 12.3 (34) | 10.0 (38) | 14.7 (38) | 21.4 (24) |
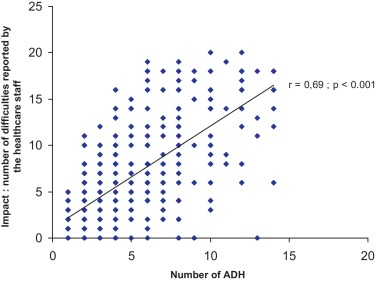
A positive correlation ( r = 0.69; P < 0.001) was found between the number of ADH locations and the number of difficulties noted by the teams ( Fig. 2 ). Among the coordinating clinicians, 25.4% thought that the observed ADHs were potentially reversible. Among the treatments that could be proposed to these patients, physical therapy came first (65.7% of clinicians interviewed), followed by medications (28.9% of clinicians) and surgery (8.8% of answers).
1.3
Discussion
The lack of a standard definition for affections, which are commonly called “contractures”, explains the varying prevalence reported in the literature. According to the different authors and criteria selected, 20 to 75% of elderly institutionalized subjects would present at least one contracture on a limb . This lack of standardized definition is quite harmful since the presence or absence of contractures has sometimes been considered as an indicator of quality of care for persons living in institutions .
In our study, the expert committee made of geriatricians, PM&R physicians and orthopedic surgeons suggested a new term “acquired deforming hypertonia” or ADH to describe this type of deformity.
The definition of ADH ( see Methods ) takes into account not only its common clinical characteristics but also its consequences (impact).
Among the common clinical characteristics, decreased ROM remains a central element for the diagnosis as underlined in the previous definitions . However, this reduction in joint ROM is not mandatory to bring up the diagnosis of ADH. The notion of hypertonia, which is not unequivocal in elderly subjects, is associated to this definition. The latter translates the increased resistance of the concerned joints to passive movements. This hypertonia can have a neurogenic component caused by pyramidal (stroke, myelopathy) or extrapyramidal (striatal hand deformities ) affections.
An oppositional behavioral component is frequently associated to increased resistance, especially in patients with frontal syndrome.
The increased resistance to passive movements can also be linked to non-neurogenic factors such as changes in joint, periarticular, muscle or tegument structures.
Altered structures of the extracellular matrix and changes in the mechanical properties of collagen fibers, for the tendons or joint capsule, have been described in animals, after joint immobilization and in the absence of nervous system lesions . For muscles, histological and biomechanical changes observed during immobilization (amyotrophy, reduction and changes in the repartition of the different fibers, reduction in the number of sarcomeres) are involved in the ADH process. These changes, which appear early on, were specifically described for paretic muscles immobilized in a shortened position .
Furthermore, we wanted this definition of ADH to be practical and applicable to all healthcare professionals in order to help them to determine therapeutic objectives. The notion of consequences (impact) in terms of discomfort, pain or functional limitations was integrated into the definition. Thus, a simple decrease in joint ROM, without any clinical or functional consequences should not be defined as ADH. This element differentiates our definition from the ones previously proposed . In fact, according to our proposed definition and evaluation criteria, ADH prevalence was estimated at 22% in the population of elderly subjects in this study. Compared to the literature, the prevalence reported here is located in the lower bracket of the estimates seen in the literature. The more restrictive nature of the definition and the evaluation criteria used can partly explain this result.
Nevertheless, the reported prevalence can validate the great frequency of ADHs. More than one patient out of five living in a geriatric institution is affected (i.e. more than 110,000 persons in France). But ADH is not just limited to elderly patients in institutions and the number of older persons concerned by this affection is certainly much greater. According to Bergström et al. who conducted a prevalence study in ordinary settings, 20% of patients presented at least one ADH at the knee level. Other studies would be necessary to refine the prevalence of ADH in elderly patients living at home.
In our work we did not evaluate the prevalence of ADH for the trunk or cervical area. This component would merit to be studied individually, even if in clinical practice these axial deformities observed in elderly subjects are most often associated to cases of peripheral ADH of the limbs.
At the time of the study, less than 15% of patients exhibited only one ADH whereas over one-third of patients had more than 5 ADHs. The cross-sectional nature of our study prevented us from apprehending the temporal sequence behind the onset of one or more ADHs in a given individual. Nevertheless, this sequence is certainly influenced by the number and type of associated pathologies specifically of the locomotor system and central nervous system . The restricted mobility and loss of autonomy triggered by these associated pathologies represent a major factor for the development of these ADHs. However, the environment remains determinant. Insufficient or absent solicitations of a person’s residual capacities generate additional functional impairments increasing the risk of developing ADH . Restorative nursing care programs, which are intended to fully use the potential of institutionalized elderly persons in their daily living activities – “doing along with the person rather than discharging the person” – have shown their effectiveness. They enable patients to maintain a sufficient level of functional mobility to reduce the risk of developing ADH . These programs prevent the permanent set-in of a vicious circle associating loss of autonomy, functional and gesture deterioration and onset of ADH. Nevertheless, implementing these programs requires enough healthcare professionals trained for this type of care.
Regarding ADH impact evaluated by healthcare teams, the most reported difficulties were the ones with a direct impact on care management (nursing, self-care, getting dressed). However, the consequences on more functional components such as gait pattern or grasping capacities were less frequently reported. This may in fact underline that the functional consequences of ADH are underestimated in highly dependent patients who already need third-party assistance for most ADL. The residual functional capacities of these patients can sometimes be deemed too poor to be affected by the development of one or more ADH locations.
Data collection on the opinion of patients and family caregivers, which was not done in this study, could have brought different additional elements to appreciate the impact of ADH. In about 17% of cases, for upper and lower limbs, the consequences of ADH did not fit with the pre-established list of consequences. Furthermore, the existence of isolated, spontaneous or provoked pain was not clearly indicated in the data collection form as a potential ADH consequence (see Fig. 1 ). The proposed list would need to be completed in order to set therapeutic objectives for ADH care management in routine clinical practice.
Regarding therapeutic options, the analysis of clinicians’ answers underlined a certain fatality, as 75% of them judged these ADH irreversible. On the other hand, more than two-third of clinicians thought that physical therapy could be useful whereas less than one-third deemed medications or surgery to be relevant for these patients. These results can seem quite paradoxical and do unveil physicians’ lack of knowledge on potential therapies for ADH care management. Besides preventive strategies, some local treatments (injections of Botulinum Toxin A or chemical neurolysis with phenol or ethyl alcohol) or surgical techniques (percutaneous tenotomy) can be proposed to fight these hypertonic deformities. However in this indication the lack of a consensus on the use of these different strategies or techniques, their restricted availability as well as the lack of a standardized decision tree, can explain why elderly patients have such a limited access to these treatments.
Further studies should be conducted to refine and harmonize therapeutic procedures for ADH if we aim to improve care management for these patients. A multidisciplinary approach involving surgeons, PM&R physicians, geriatricians and healthcare professionals is the basis for improving care management.
Even though our work was based on a large number of centers and residents, some limits must be acknowledged. The cross-sectional and observational nature of this study, prevented us from giving an estimate on the number of subjects who already had one or more ADH upon admission, or identifying the determining factors related to the onset of ADH. Furthermore, as they were not part of the initial objectives for this study data on history, associated pathologies as well as the person’s level of dependence were not recorded. Thus, the necessary pathological conditions common to the development of ADH were not analyzed in this work. We only collected data for patients who presented at least one ADH. There was no control group of healthy subjects, which limits the interpretation of some results. Thus, the mean age of patients with ADH is most probably higher than the mean age of other residents even if our study cannot confirm this. In fact, according to the DREES study, the mean age of patients living in EHPAD structures in 2009 was 84 years and 9 months .
In spite of its limits, this study helped validating on a large cohort the strong prevalence of ADH in elderly subjects living in EHPAD or USLD institutions. Consequences in terms of increased dependence and reduced quality of life seem particularly important. Besides preventive actions, several therapeutic options could and should be envisioned for this pathology. However, additional studies need to be conducted to establish a hierarchical care management strategy adapted to this population of elderly and frail subjects. Today, fatality should not be the only option when faced with ADH in elderly populations.
Disclosure of interest
P. Dehail, A.L. Godard, N. Faucher, Y. Coulomb, A. Schnitzler, P. Denormandie, C. Jeandel are consultants for Allergan.
Acknowledgements
The authors wish to thank: all clinicians and centers involved in this project: Dr. Alavoine – 83418 Hyères, Dr. Navarre – 30129 Manduel, Dr. Sarfati – 48600 Grandrieu, Dr. Françoise – 75000 Paris, Dr. Amberny – 84200 Carpentras, Dr. Chol – 42055 Saint-Étienne, Dr. Demier – 75000 Paris, Dr. Garigue – 75000 Paris, Dr. Scemama – 78280 Guyancourt, Dr. Wolmark – 75000 Paris, Dr. Raoilijaona – 30450 Ponteils, Dr. Fassin – 75000 Paris, Dr. Sibrik – 75000 Paris, Dr. Durand – 42270 Saint-Priest-en-Jarez, Dr. Chanelière-Sauvant – 42000 Saint-Étienne, Dr. Benhamou – 75885 Paris, Dr. Terrat – 42000 Saint-Étienne, Dr. Fargier – 42000 Saint-Étienne, Dr Blanchon – 42000 Saint-Étienne, Dr. Teyssier – 34290 Abeilhan, Dr. Cressot – 33000 Bordeaux, Dr. Jenn – 33000 Bordeaux, Dr. Bourdin – 33000 Bordeaux, Dr. Paries – 33550 Langoiran, Dr. Ducos – 33000 Bordeaux, Dr. Dupart – 33170 Gradignan, Dr. Thomas – 33120 Arcachon, Dr. Pardessus – 59037 Lille, Dr. Rwabihama – 91211 Draveil, Dr. Ranovona – 91750 Champcueil.
ALLERGAN France, for its logistics support for this study (expert meetings for the design and implementation of this project and financing the observation notebooks).
The research unit from the KORIAN group for its work on database entry from the observation notebooks and control support.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








