Acetabular Fractures: Ilioinguinal Approach
Joel M. Matta
Mark C. Reilly
Indications/Contraindications
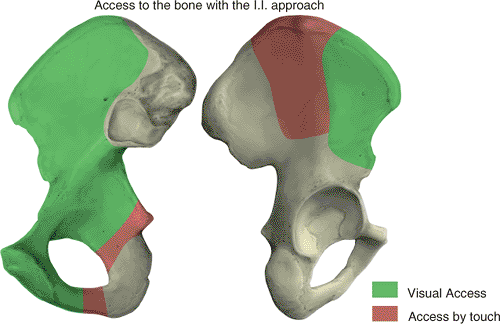
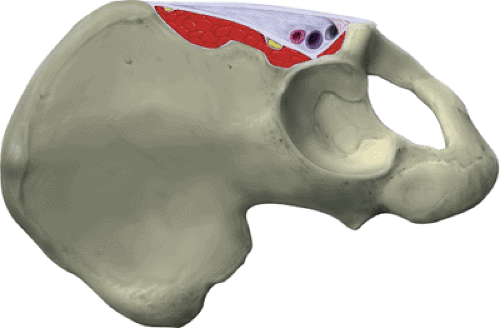
The ilioinguinal approach was developed by Letournel as an approach to the anterior column of the acetabulum and the inner aspect of the innominate bone. It allows exposure of the entire, internal, iliac fossa and pelvic brim from the anterior aspect of the sacroiliac joint to the pubic symphysis. The quadrilateral surface of the innominate bone and the superior and inferior rami are also accessible. Access to a portion of the external aspect of the ilium also is possible (Fig. 42.1).
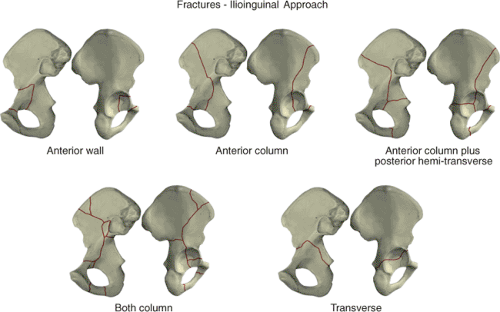
The ilioinguinal is the approach of choice for all fractures of the anterior wall and column. The majority of acute, associated, anterior-plus-posterior, hemitransverse fractures may also be managed with the ilioinguinal approach. If the fracture is older than 15 days, the ilioinguinal may still be used unless the posterior component of the fracture is significantly displaced. In this circumstance, an extended iliofemoral approach is more applicable.
The ilioinguinal approach may be used for the majority of associated both-column fractures. The presence of a fracture involving the posterior wall does not necessarily preclude the use of this approach. If the posterior-wall fragment contains a spike of ilium, the reduction may be possible through the exposure of the lateral ilium. The ilioinguinal approach is not recommended for an associated both-column fracture with small or comminuted posterior-wall fragments or those with fracture involvement of the sacroiliac joint.
Certain transverse fractures also may be managed with the ilioinguinal approach. Specifically, fractures with significant displacement at the pelvic brim but slight or no displacement posteriorly may be addressed in this manner. In addition, the ilioinguinal may be used as a subsequent approach when incomplete reduction of the anterior column portion of a T-shaped fracture has been obtained through a prior Kocher-Langenbeck approach (Fig. 42.2).
Preoperative Planning
Initial radiographic evaluation of a patient with an acetabulum fracture should include an anteroposterior (AP) pelvic radiograph and 45-degree oblique views of the pelvis. Although obtaining these views may be initially uncomfortable for the patient, they are vital to fully understand the fracture pattern. Adequate analgesia should be provided, and the physician may need to be on-site to ensure proper positioning. These films should be obtained in the radiology department rather than as portable radiographs and with the patient out of traction. A careful evaluation of the radiographs allows the fracture to be classified properly by determination of the exact fracture pattern.
Computed tomography (CT) may add important additional information regarding the fracture configuration and presence of incarcerated or impacted fragments within the acetabulum. Three-dimensional CT reconstructions also can assist in providing a better understanding of complicated fracture patterns. Drawing the fracture on a dry bone or pelvic model (or drawing the innominate bone) helps ensure that the surgeon understands the fracture configuration before embarking on surgical intervention.
The ilioinguinal approach proceeds through anatomic areas infrequently used by most orthopedic surgeons. In addition, reduction of the fracture and proper placement of fixation require a thorough understanding of the fracture pattern and the normal acetabular anatomy. Before undertaking the approach, the surgeon is strongly advised to practice on a cadaver and to assist a surgeon who is familiar with the exposure, reduction, and fixation of these difficult injuries.
Surgery
Technique of Approach
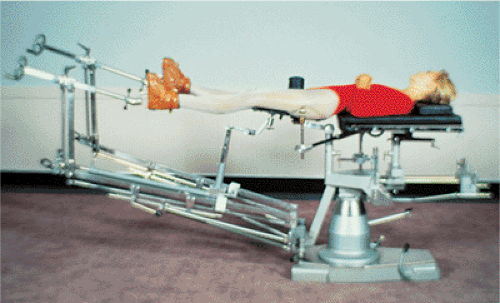
The surgery is performed under general anesthesia with the patient positioned supine on the Judet–Tasserit fracture table (Fig. 42.3). The affected leg is positioned with the hip slightly flexed to relax the iliopsoas muscle, femoral nerve, and external iliac vessels. If required during the surgery, a lateral traction device may be used through a traction screw placed into the greater trochanter. Before surgery, a Foley catheter is introduced into the bladder.
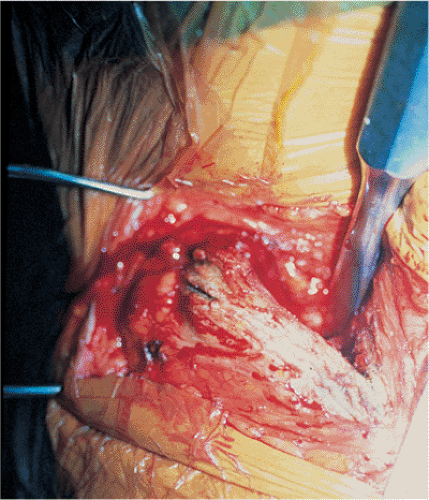 Figure 42.5. Release of the insertion of the abdominal muscles and subperiosteal dissection of the internal iliac fossa. |
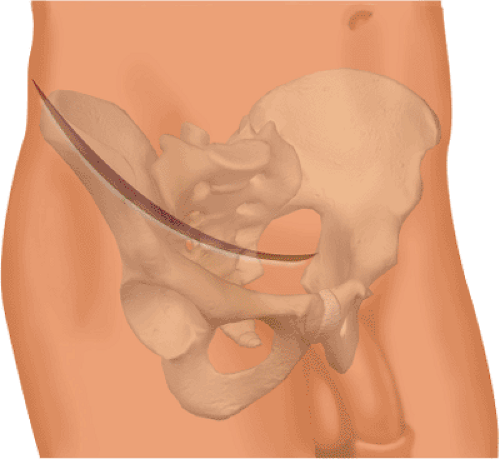
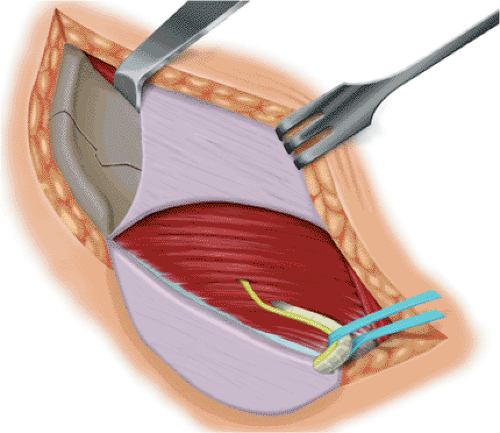
The incision begins at the midline, 3 to 4 cm proximal to the symphysis pubis. It proceeds laterally to the anterior, superior, iliac spine and then along the anterior two thirds of the iliac crest. The incision must extend beyond the most convex portion of the ilium (Fig. 42.4). The periosteum is incised along the iliac crest, and the attachment of the abdominal muscles and the origin of the iliacus are released. By subperiosteal dissection, the iliacus is elevated from the internal iliac fossa as far posterior as the sacroiliac joint and medially to the pelvic brim (Fig. 42.5). The internal iliac fossa is then packed for hemostasis. Through the lower portion of the incision, the aponeurosis of the external oblique muscle and the external rectus abdominis fascia are exposed. These structures are sharply incised in line with the cutaneous incision at least 1 cm proximal to the external inguinal ring. The aponeurosis of the external oblique muscle is then reflected distally. This unroofs the inguinal canal and exposes the inguinal ligament. The spermatic cord or round ligament is visualized at the medial aspect of the incision. A Penrose drain is then placed around the spermatic cord or round ligament and the adjacent ilioinguinal nerve. It may be used to facilitate retraction during the procedure (Fig. 42.6).
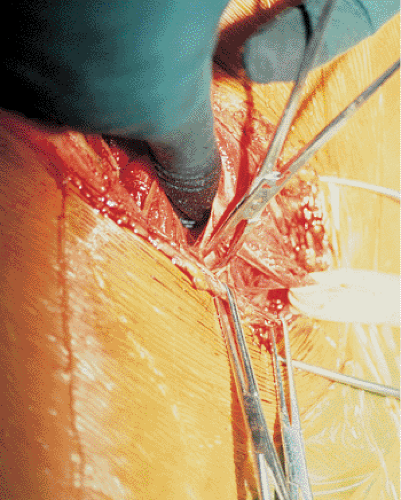
The inguinal ligament is sharply incised so that a 1- to 2-mm cuff of the ligament remains with the common origin of the internal oblique and transversus abdominis muscles and the transversalis fascia (Fig. 42.7). Great care must be taken to avoid injuring the underlying neurovascular structures. Immediately beneath the inguinal ligament, the lateral femoral-cutaneous nerve exits into the thigh. This nerve may be found adjacent to or up to 3 cm medial to the anterior, superior, iliac spine. It must be identified and protected throughout the operation. Directly beneath the midportion of the incision lie the external iliac vessels (Fig. 42.8). Medial to these vessels, the insertion of the conjoined tendon onto the pubis is incised. It may be necessary to incise a portion of the rectus abdominis tendon as well; it is incised just above its insertion onto the pubis. The retropubic space of Retzius is now accessible and is packed with moist sponges after evacuation of the fracture hematoma.
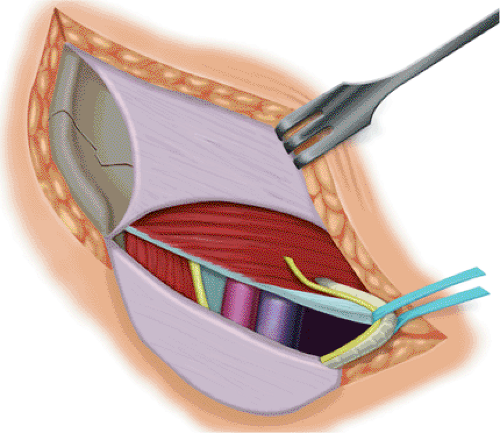
At this point, the anterior aspects of the femoral vessels and the surrounding lymphatics are exposed in the midportion of the incision within the lacuna vasorum. The more laterally situated lacuna musculorum contains the iliopsoas, the femoral nerve, and the lateral
femoral cutaneous nerve. The iliopsoas sheath, or iliopectineal fascia, separates the two lacunae (Fig. 42.9). The vessels and lymphatics are carefully dissected away and retracted from the medial aspect of the fascia, and the iliopsoas muscle and femoral nerve are retracted from the lateral aspect (Figs. 42.10 and 42.11). The iliopectineal fascia is sharply incised to the pectineal eminence (Fig. 42.12). The pulse of the external iliac artery should be palpated before this step to ensure that the vascular bundle is protected from injury. The iliopectineal fascia is sharply detached from the pelvic brim (Fig. 42.13). In certain individuals, this occasionally may be performed with finger dissection. Detaching the iliopsoas fascia allows access to the true pelvis and subsequently the quadrilateral surface and the posterior column. A second Penrose drain is placed around the iliopsoas; femoral nerve;
and lateral, femoral, cutaneous nerve for retraction purposes. A third Penrose is placed around the femoral vessels and lymphatics. Care should be taken to leave undisturbed the fatty areolar tissue surrounding the vessels, as this contains the lymphatic vessels. Disrupting the lymphatics may result in impaired postoperative lymphatic drainage and edema.
femoral cutaneous nerve. The iliopsoas sheath, or iliopectineal fascia, separates the two lacunae (Fig. 42.9). The vessels and lymphatics are carefully dissected away and retracted from the medial aspect of the fascia, and the iliopsoas muscle and femoral nerve are retracted from the lateral aspect (Figs. 42.10 and 42.11). The iliopectineal fascia is sharply incised to the pectineal eminence (Fig. 42.12). The pulse of the external iliac artery should be palpated before this step to ensure that the vascular bundle is protected from injury. The iliopectineal fascia is sharply detached from the pelvic brim (Fig. 42.13). In certain individuals, this occasionally may be performed with finger dissection. Detaching the iliopsoas fascia allows access to the true pelvis and subsequently the quadrilateral surface and the posterior column. A second Penrose drain is placed around the iliopsoas; femoral nerve;
and lateral, femoral, cutaneous nerve for retraction purposes. A third Penrose is placed around the femoral vessels and lymphatics. Care should be taken to leave undisturbed the fatty areolar tissue surrounding the vessels, as this contains the lymphatic vessels. Disrupting the lymphatics may result in impaired postoperative lymphatic drainage and edema.
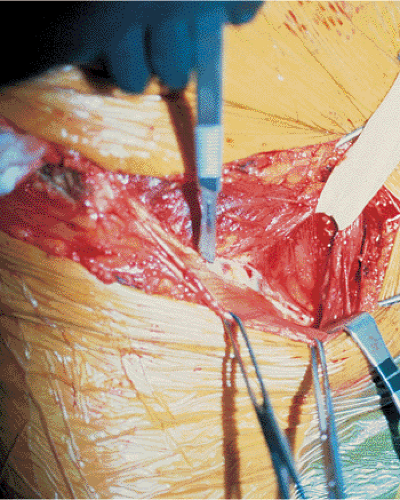 Figure 42.8. Directly beneath the inguinal ligament lie the external iliac vessels. Note how superficial the external iliac artery and vein may lie beneath the ligament. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree