A Biopsychosocial Perspective on Motor Vehicle Collisions: Beyond Forces, Flexion, and Fractures
Dennis C. Turk
James P. Robinson
Over 6.7 million police-reported motor vehicle collisions (MVC) occur each year in the United States [40]. A significant minority of these result in deaths (approximately 42,000) and injuries (3.4 million). Although some of these injuries are relatively minor and resolve within a few days or weeks, up to 50% of those injured report ongoing symptoms at long-term follow-up [6, 29]. The most common type of injury sustained in an MVC is whiplash [44]. The term “whiplash” (WL) has been used variously to refer to a process (the head of the passenger or driver is subject to acceleration/deceleration forces that hyperextend and hyperflex the neck [22], to the resulting injury (i.e., WL), and to the syndrome of symptoms following such an injury (whiplash syndrome) [1, 37]. The Quebec Task Force on Whiplash-Associated Disorders (WADs) [53] created a grading system of WADs caused by MVCs. This distinguishes individuals with neck pain but no physical findings (Grade I) from ones with pain as well as musculoskeletal findings such as reduced cervical range of motion (Grade II), neurological injury (Grade III), or major skeletal injury such as a fracture (Grade IV). The present chapter focuses on people with Grade I or II WADs; they comprise more than 90% of all WADs [53].
Although acute WAD symptoms are distinctly unpleasant, WAD becomes an important health issue when it becomes chronic. Estimates of the percentage of people with acute WADs who go on to develop chronic symptoms range widely from 13% to 64% [1, 12, 43]. The wide variation is likely due to the method of recruiting participants in studies (e.g., emergency department, newspapers, referred to specialist), time since MVC (hours to months), and criteria used to define WADs. Once WADs become chronic, they are extremely resistant to treatment. In this chapter, we focus on biological, psychological, and social factors that lead to chronic WADs.
The data reviewed above raise a fundamental question then: Why do some people who appear to sustain relatively minor injuries recover quickly, whereas others who have been involved in what are apparently comparable MVCs and who sustain indistinguishable physical pathology develop a diverse set of chronic symptoms, most prominently pain and significant disability? A number of potential contributors to the discrepancies have been noted and investigated (see Table 11-1). Each of the contributors has its proponents and evidential base, depending on expertise, interest, and specialty of advocates for them.
The biopsychosocial model focuses on both disease and illness, with illness being viewed as the complex interaction of biological, psychological, social, and contextual factors [19]. The model presumes some form of physical pathology, or at least physical changes in the muscles, joints, or nerves that generate sensory input transmitted to the brain. At the periphery, nociceptive fibers transmit sensations that may or may not be interpreted as “pain.” Such sensations are not yet considered pain until subjected to higher order psychological and mental processing that integrates sensory information with prior learning history, appraisals, and emotional factors to create the perception of pain. Appraisal processes are central to the perception of pain. They involve the meaning that is attributed to sensations as well as an individual’s expectations and beliefs about coping strategies to ameliorate the pain
and return to normal functioning. A person may choose to ignore the pain and continue engaging in previous levels of activity such as working or household activities, or may choose to refrain from all activity and assume the sick role and accompanying disability.
and return to normal functioning. A person may choose to ignore the pain and continue engaging in previous levels of activity such as working or household activities, or may choose to refrain from all activity and assume the sick role and accompanying disability.
TABLE 11-1 Potential Contributors to the Development of Chronic Pain and Disability among WAD Patients | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Flor and Turk [19] describe multiple ways in which a person’s appraisals affect his or her processing of external or internal stimuli related to the experience of stress and pain. These include increased perception, preoccupation with and overinterpretation of physical symptoms, or inadequate perception of internal stimuli such as muscle tension levels. Moreover, they suggest that the nature of the coping response— active avoidance, passive tolerance, or depressive withdrawal—may determine the type of problem that develops, as well as the course of the illness. Flor and Turk further propose that subsequent maladaptive physiological responding, such as increased and persistent sympathetic
arousal and increased and persistent muscular reactivity, as well as sensitization of central structures including the cortex, may induce or exacerbate pain episodes. Thus, they suggest that learning processes in the form of respondent conditioning of fear of activity (including social, motor, and cognitive activities), social learning, and operant learning of pain behaviors make a contribution to the chronicity of pain. They also point out that the responses of a person with a painful condition will be shaped by the behaviors of significant others. These may promote either healthy or maladaptive beliefs and responses.
arousal and increased and persistent muscular reactivity, as well as sensitization of central structures including the cortex, may induce or exacerbate pain episodes. Thus, they suggest that learning processes in the form of respondent conditioning of fear of activity (including social, motor, and cognitive activities), social learning, and operant learning of pain behaviors make a contribution to the chronicity of pain. They also point out that the responses of a person with a painful condition will be shaped by the behaviors of significant others. These may promote either healthy or maladaptive beliefs and responses.
In the biopsychosocial model, emphasis is shifted from the pathophysiology that may have been involved in the initiation of nociception to the patient’s thoughts and feelings, and conditioned responses that influence his or her subsequent behavior and pain experiences. From this perspective, assessment of, and consequently treatment of, the patient with persistent pain requires a broad strategy that examines and addresses a wide range of psychosocial and behavioral factors, in addition to, but not to the exclusion of, biomedical ones.
Fig. 11-1 presents a schematic representation of the biopsychosocial model, depicting the overlapping sets of biological, psychological,
and social factors that affect the experience of chronic WADs, with the MVC serving as the precipitating event [see also 18, 38]. It is important to recognize that when WADs become chronic, the interplay of physical, psychosocial, behavioral, and economic factors evolves over time. Thus, none of these factors should be viewed as static.
and social factors that affect the experience of chronic WADs, with the MVC serving as the precipitating event [see also 18, 38]. It is important to recognize that when WADs become chronic, the interplay of physical, psychosocial, behavioral, and economic factors evolves over time. Thus, none of these factors should be viewed as static.
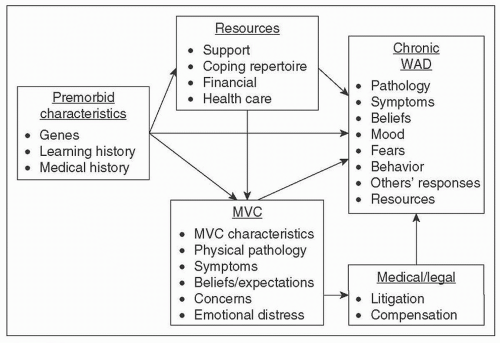 FIGURE 11-1 Biopsychosocial perspective on whiplash-associated disorders. MVC, motor vehicle collision; WAD, whiplash-associated disorder. |
Sociodemographic Factors
Sociodemographic factors such as sex, age, marital status, and educational levels are construed as predisposing factors in the biopsychosocial model. These factors have been studied extensively in relation to WADs. Research on the role of various sociodemographic factors has yielded inconsistent results. One recent systematic review and meta-analysis indicated that female sex and no education beyond secondary school were significant, though modest, risk factors for persistence of problems following WL injury [63]. However, another systematic review published at about the same time reported that sociodemographic factors were not related to poorer outcomes following an MVC [29]. Thus, at this point, no conclusive comments can be made as to the role of any sociodemographic variables in the development of chronicity following a WAD sustained in an MVC.
Vehicle and Crash-related Factors
Research on vehicle and crash-related factors can be conceptualized as addressing the biomechanical stimuli (e.g., loads, forces, energy) that induce WADs. Individual cohort studies have implicated a range of crash-related factors in poor recovery [47]. However, a more recent review found that the only significant vehicle or collision factor that had any significant predictive power was not wearing a seat belt [63], and a recent systematic review and meta-analysis concluded that crash-related (i.e., direction, speed of impact, severity of the collision) and vehicle factors (e.g., head rest, seating position, seat belt use) did not have consistent predictive value [29].
Physical Pathology
Research on structural and physiological abnormalities among WAD patients can be construed as addressing the biomechanical responses of individuals to the strains created by MVCs. Various authors have implicated a wide range of structures in the pathophysiology of WADs— including bones, facet joints, intervertebral disks, ligaments, muscles, and neural structures. Despite decades of research, it has been difficult to identify the structural or physiological abnormalities that underlie WADs. In particular, radiological studies designed to identify structural abnormalities in WAD patients have generally failed to do so [6]. The disappointing results of radiological studies have led some investigators to assert that in more than 90% of WL claims, no organic pathology can be detected [17].
In interpreting studies on the structural/physiological substrates of WAD, several issues need to be considered. First, although it is logical to assume that radiological studies should be able to detect structural abnormalities created by the forces generated during MVCs, and that such abnormalities should permit pathoanatomic diagnoses to be given to WAD patients, some investigators reject the primacy of imaging studies in the diagnosis of these patients. In particular, Lord and colleagues [33, 34] have asserted that responses of patients to local anesthetic blocks represent the best method of diagnosing structural/physiological abnormalities. On the basis of patients’ responses to local anesthetic blocks and subsequent facet neurotomies, these and other investigators have concluded that a substantial proportion of WAD patients have abnormalities in their cervical facet joints [34, 35]. For purposes of this chapter, the broad point is that statements about the frequency of biological abnormalities in WAD patients are uninterpretable unless there is agreement on the criteria for diagnosing these abnormalities.
Another problem is that research on the structural basis of WAD assumes that a pain generator in the cervical spine (e.g., an inflamed facet joint) leads in a straightforward way to WAD symptoms. Thus, it is assumed that the nervous system of a WAD patient responds to tissue damage in an uncomplicated way, and is “veridical” in the sense that
the pain experiences of a patient accurately reflect this damage [49]. This assumption is challenged by a growing body of research indicating that persistent WAD is often mediated by sensitization of the central nervous system [11, 28, 61]. As an example of problems in this area, Turk et al. [60] found that 46% of a cohort of people with WADs with no known other injuries met the tender point criterion for a diagnosis of fibromyalgia—they reported tenderness in at least 11 of the 18 sites designated by the American College of Rheumatology for the diagnosis [65]. The significance of this widespread hyperalgesia is not entirely clear, but it certainly suggests that the pain experienced by many people with WADs is not reducible to a single structural abnormality. To the extent that persistent WAD pain is mediated by altered nervous system responsivity rather than by ongoing nociceptive input from the neck, there is no reason to expect a one-to-one relation between WAD symptoms and a definable structural lesion in the neck.
the pain experiences of a patient accurately reflect this damage [49]. This assumption is challenged by a growing body of research indicating that persistent WAD is often mediated by sensitization of the central nervous system [11, 28, 61]. As an example of problems in this area, Turk et al. [60] found that 46% of a cohort of people with WADs with no known other injuries met the tender point criterion for a diagnosis of fibromyalgia—they reported tenderness in at least 11 of the 18 sites designated by the American College of Rheumatology for the diagnosis [65]. The significance of this widespread hyperalgesia is not entirely clear, but it certainly suggests that the pain experienced by many people with WADs is not reducible to a single structural abnormality. To the extent that persistent WAD pain is mediated by altered nervous system responsivity rather than by ongoing nociceptive input from the neck, there is no reason to expect a one-to-one relation between WAD symptoms and a definable structural lesion in the neck.
A third issue is that even when diagnoses of structural pathology in the cervical spines of WAD patients can be made, the diagnoses are qualitative and thus do not provide insight into why some WAD patients report prolonged pain and demonstrate severe disability, whereas others complain of only mild, transitory symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


