Fig. 2.1
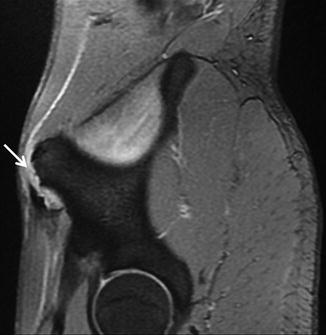
Fig. 2.2

Fig. 2.3
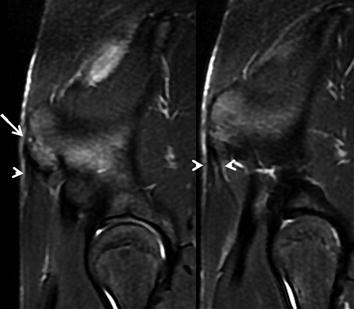
Fig. 2.4
A 17-year-old male soccer player complained of sudden pain and loss of function when running while training.
Comments
Avulsion fractures of the anterior superior iliac spine are rare injuries. However, they commonly affect the growing apophyses in adolescents undergoing vigorous activity.
In the immature skeleton, the apophysis (a cartilaginous growth center where a tendon attaches to bone) remains weaker than the attached musculotendinous unit until it fuses at the time of skeletal maturity and thus is more prone to fracture when the musculotendinous unit is suddenly and vigorously contracted.
The anterior superior iliac spine, which develops from an iliac crest’s anterior apophysis, not normally fused until aged 20–25, is an insertion point for the sartorius muscle and part of the tensor fasciae latae. An avulsion fracture of the anterior superior iliac spine is most commonly due to forceful contraction or sudden repetitive actions of these muscles, as occurs when running or kicking a ball. Sprint athletes, soccer players, and gymnasts are the most frequently affected athletes due to the range of movements performed and sudden changes in direction required.
Plain radiographs are useful and the cheapest technique to diagnose this injury even though muscle insertions are not seen. MRI, CT, and sonography enable a more accurate diagnosis. MRI and sonography are a better choice than CT as they do not emit ionizing radiation.
The treatment of choice for this injury remains conservative: rest, analgesia, anti-inflammatories, and physical therapy; however, surgical treatment has been used depending on the degree of fracture displacement and the individual’s rehabilitation requirements.
Patients frequently take long periods of time to recover. This particular soccer player took 61 days to return to competition.
Radiological Findings
Axial fat-suppressed T2-weighted FSE MR image (Fig. 2.1) shows the incomplete anterior superior iliac spine (ASIS) fracture, with the internal cortex still attached to the iliac crest (arrow). Subcutaneous edema (open arrow) and surrounding hematoma (slightly more hyperintense than muscle) are clearly appreciated. The gap at the fracture (arrow) is nicely seen in this sagittal fast gradient-recalled weighted MR image (Fig. 2.2).
Oblique fast T2-weighted MR image (Fig. 2.3) from the fracture’s inner side clearly shows the integrity of the internal cortex (arrow). Sartorius and fascia latae tendon insertions (arrowheads) are seen attached to the avulsed apophysis.
The two continuous oblique fat-suppressed proton density-weighted MR images (Fig. 2.4) 4 months later show healing of the ASIS avulsion (arrow) with both tendon insertions (arrowheads) attached to it.
Case 2.2: Acute Avulsion Fracture of the Anterior Inferior Iliac Spine

Fig. 2.5
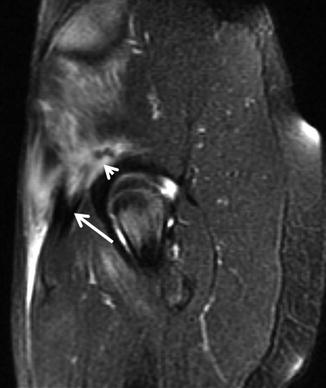
Fig. 2.6
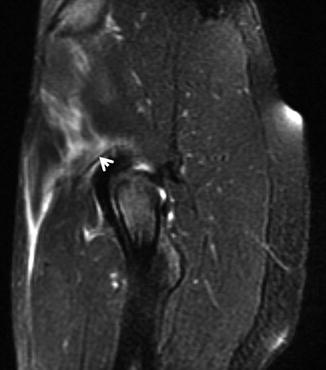
Fig. 2.7

Fig. 2.8
A 15-year-old soccer player suffered a sudden groin pain when sprinting during preseason training on the beach. On examination, there was pain and loss of function on hip flexion.
Comments
Rectus femoris (RF) avulsion is not as common as its myotendinous junction injury which is commonly reported among adolescent athletes involved in kicking sports.
The anterior inferior iliac spine’s apophysis (AIIS) begins to ossify between years 13 and 14 and it is not complete until years 16–18; therefore, this unfused apophysis in immature athletes is the weakest link in the muscle-tendon-bone chain.
The rectus femoris muscle has two proximal tendinous insertions above the hip: the direct (straight) head, arising from the anterior inferior iliac spine (AIIS), and the indirect (reflected) head, arising more inferiorly and posteriorly from the superior acetabular ring and hip joint capsule. Both heads form a conjoined tendon a few centimeters below their origins.
The apophysis’ avulsion is an acute injury that typically occurs due to a single episode of violent eccentric contraction of the RF, as hip extends and knee is flexed (as happens in a case of an “empty kick”). Generally, displacement of the fragment is no more than 1.5 cm, and the lesion usually has a good outcome with conservative treatment alone but requires long periods of rest (this player took 83 days to return to competition). The indirect tendon can remain attached to its insertion during AIIS avulsion injury.
The typical crescent-shaped avulsed AIIS fragment is seen in plain radiograph, CT, sonography, and MRI, but the indirect tendon insertion is only seen on MRI, making it the technique of choice for this injury.
Imaging Findings
Fracture line with a mild displacement of the apophysis and direct tendon (open arrow) with edema and hemorrhage in surrounding tissues are seen in the first (Fig. 2.5) of these oblique sagittal fast T2-weighted MR images (parallel to the iliac wing). The hyperintense appearance of the apophysis cartilaginous compound (arrow) accounts for the loss of demarcation in this sequence.
Both the conjoined tendon (arrow) [showing integrity of myotendinous junction] and the partial disruption of the indirect tendon insertion (arrowhead) are seen in a contiguous external slice (Fig. 2.6). Fibers of this indirect tendon still attached to its insertion (arrow) are seen in the next contiguous external slice (Fig. 2.7).
In the sagittal proton density-weighted image (Fig. 2.8) taken 4 months later, the avulsed fragment is seen attached to the iliac crest with fibrous and ossified tissue. A retracted and mildly atrophic proximal rectus femoris muscle is also appreciated as the result of the injury.
Case 2.3: Anterior Inferior Iliac Spine Apophysitis Evolution
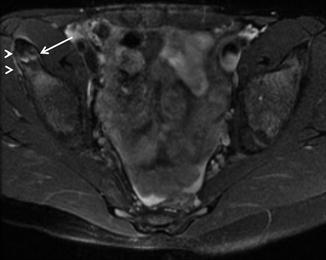
Fig. 2.9
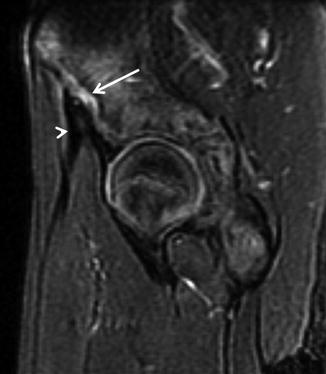
Fig. 2.10
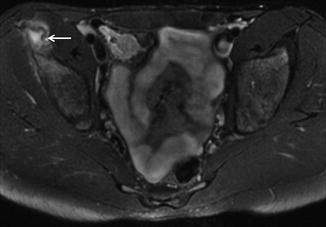
Fig. 2.11
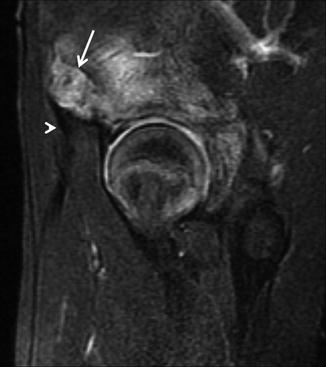
Fig. 2.12
A 13-year-old soccer player complained of groin pain when kicking right at the beginning of the season. After resting for 2 months, he gradually returned to play with no pain. A month later, he developed acute groin pain and loss of function during competition.
Comments
Anterior inferior iliac spine (AIIS) apophysitis is a chronic injury caused by repetitive microtrauma secondary to rectus femoris (RF) tendon traction from the apophyseal insertion. With more adolescents participating in highly competitive athletic activities, it has increased in prevalence over the past several decades.
The apophysis is a secondary ossification center that contributes to the size and shape of the bone, but not to its length. It is connected to the parent bone through an associated physis. Apophyses have also been termed “traction epiphyses.” Distraction from chronic and repetitive musculotendinous pull is thought to stimulate chondrocyte proliferation or inflammatory cell hypertrophy at the physis, resulting in the apparent physeal widening and adjacent muscle edema seen on MRI, thus the term “apophysitis.” The physis’ hyaline cartilage adjacent to the apophysis is the site of less resistance until the apophysis is fused (age 16–18), so it is prone to be injured in adolescents overusing the rectus femoris muscle, such as soccer players and athletes.
Patients complain of vague pain over a period of time, not related to a specific episode of violent contraction. Aggravation of the apophysitis or avulsion of the anterior inferior iliac spine (AIIS) can occur with a sudden and vigorous contraction of the rectus femoris muscle, as was the case in this occasion.
Ultrasound is a better choice than plain radiography to detect this injury since it is capable of detecting non-ossification centers. Apophysitis is seen in MRI usually as a mild physeal widening of about 3–5 mm (as in this patient’s initial episode) with hyperintensity on water-sensitive sequences, bone marrow edema, and, frequently, peripheral muscle edema.
The treatment usually consists of anti-inflammatory medication, activity modification, and rehabilitation. In this particular case, a complicated progress meant the patient required 9 months to return to practice.
Radiological Findings
The axial fat-suppressed T2-weighted image (Fig. 2.9) at the right AIIS shows a faint physeal widening (arrow) without displacement. Minimal edema (arrowheads) is seen surrounding the physis without bone marrow edema. The sagittal fat-suppressed T2-weighted image (Fig. 2.10) clearly shows the minimal widening of the physis and the direct rectus femoris tendon attached to the apophysis (arrowhead).
The same soccer player complained of pain 2 months later after vigorous contraction of the RF during competition. A wider apophyseal detachment (arrow) with marrow edema is clearly seen in the axial (Fig. 2.11) and sagittal (Fig. 2.12) fat-suppressed T2-weighted images. The tendon remains attached to the apophysis (arrowhead).
Case 2.4: Avulsion Injury of the Ischial Tuberosity

Fig. 2.13

Fig. 2.14
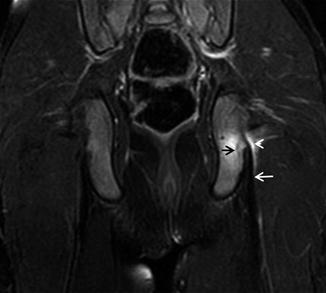
Fig. 2.15
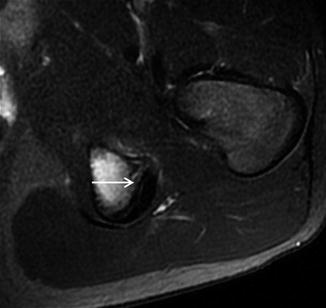
Fig. 2.16
A 14-year-old soccer player complained of sudden gluteal pain and difficulty in walking while competing.
Comments
Avulsion injuries of the ischial tuberosity are relatively common in adolescents and are commonly due to excessive eccentric contraction applied from the hamstring (HMS) muscles (long head of the biceps femoris, the semitendinosus, and the semimembranosus) that arise from it. These avulsions occur before the close of the ischial apophysis which is not completely fused until aged 20–25.
Patients usually complain of pain of sudden onset in the posterior gluteal or thigh region while the muscle is undergoing voluntary or involuntary eccentric contraction with the hip flexed and knee in extension. These injuries are common in soccer players, gymnasts, and dancers, among others.
With a mild (minor) apophyseal displacement, radiography sometimes does not provide conclusive information even though an elongated bony fragment (similar to the curve of the ischium) can occasionally be seen in oblique views (anteroposterior with 25–30º caudocranial beam inclination). MRI can be used to diagnose mild apophyseal displacement, but ultrasound can be more accurate for small cortical avulsions. If the displaced ossicle remains in close contact with the apophyseal cartilage, it can be completely reabsorbed inside the apophysis during the bone maturation process.
In larger lesions (avulsion greater than 2 cm), the apophyseal fragment tends to be displaced caudally, far away from the ischium, and can be transformed into a permanent ossicle with a spherical or oval shape with a thin cortical cover. Hypertrophied callus at ischium level and adjacent heterotopic bone should not be confused with major lesions.
Minor apophyseal displacements, as seen in this particular case, are treated with rest, icing, simple analgesics, protective weight bearing, and rehabilitation. This soccer player took 125 days to return to play. Surgical repair is indicated for either failed conservative treatment or for displacement greater than 2.5 cm.
Radiological Findings
The axial fat-suppressed T2-weighted image (Fig. 2.13) shows an elongated tiny bony fragment (white arrow) displaced from the left ischial tuberosity (asterisk) with extensive physeal (black arrow), ischial, and soft tissue edema (arrowhead). The avulsed fragment (white arrow) and periosteal stripping at the inner attachment (arrow) are clearly seen in a closer axial FSE proton density view (Fig. 2.14).
The coronal fat-suppressed T2-weighted image (Fig. 2.15) shows normal hamstring tendons (white arrow) with physeal (black arrow), ischial tuberosity, and soft tissue edema (arrowhead). Decreased bone marrow and soft tissue edema are seen in the axial fat-suppressed T2-weighted image (Fig. 2.16) taken 4 months later. The physis is undergoing fibrotic changes with no hyperintensity signal (arrow), while the avulsed fragment is not clearly defined.
Case 2.5: Avulsion Injury of the Tibial Tuberosity

Fig. 2.17
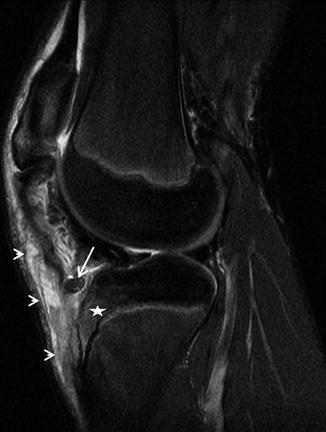
Fig. 2.18

Fig. 2.19

Fig. 2.20
A 17-year-old soccer player felt a pop below the knee after jumping to clear a ball and bouncing on the pitch. In previous weeks he had reported insidious pain over the anterior tibial tuberosity area secondary to probable Osgood-Schlatter disease.
Comments
Anterior tibial apophysis injuries in adolescents are uncommon. They are more frequent in males approaching skeletal maturity with well-developed quadriceps and in athletes with preexisting Osgood-Schlatter disease.
The tibial tuberosity develops from an ossification center appearing at ages 8–12 in girls and 9–14 years in boys. Fusion between the ossified tuberosity and tibial metaphysis is usually completed by ages 15 in girls and 17 in boys.
Avulsion fractures of the tibial tuberosity are classified by Watson-Jones into three types: Type I, the fracture line passes through the distal part of the tuberosity’s physis lifting the ossification nucleus upwards; Type II, the fracture line is longer and involves the ossification nucleus and the proximal tibial physis, but does not enter the joint; and Type III, the fracture extends into the joint.
Types I and II are more common in younger athletes (12–14), type III occurs in older ones (15–17). This classification was modified by Ogden et al. to include displacement and comminution. Other types (IV and V) have been proposed.
These injuries are sustained during athletic activity involving jumping (basketball and high jump). Two possible mechanisms of injury are involved: violent knee flexion against a tightly contracting quadriceps (as in landing from a jump) or violent quadriceps contraction against a fixed foot (as in jumping). Patients complain of immediate pain and swelling with significant disability for standing and walking, as they cannot straighten the knee.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








