Medial Patellofemoral Ligament Reconstruction
Hany Elrashidy
Joseph Carney
Najeeb Khan
Donald C. Fithian
DEFINITION
Stability of the patellofemoral joint (PFJ) is multifactorial as it depends on limb alignment, interaction of the surrounding muscles, the osseous architecture of the patella and the trochlea, and the integrity of the medial soft tissue constraints of which the medial patellofemoral ligament (MPFL) is the main component.
Of the many factors contributing to PFJ stability, the MPFL is the primary ligamentous restraint against lateral patellar displacement, with the MPFL reported to provide between 50% and 60% of the medial soft tissue resistance to lateral dislocation of the patella.4,21
Consequently, patellar dislocation often results in injury to the medial retinacular ligaments, including the MPFL, leading to increased lateral patellar mobility.
Competency of the MPFL is both necessary and sufficient to restore lateral patellar mobility to a normal range; consequently, surgical treatment should aim for restoration of a functional MPFL.
ANATOMY
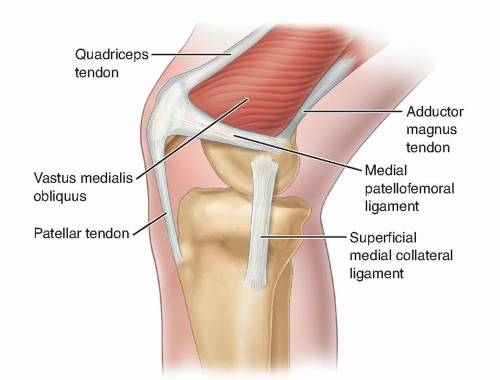
The MPFL is an extra-articular ligament that lies in layer 2, between the medial retinaculum superficially and the joint capsule on its deep surface. The vastus medialis obliquus (VMO) tendon lies superficially anteriorly and inserts onto the anterior third of the MPFL.
In a cadaveric study, the MPFL was moderately or well developed in 17 of 20 (85%) specimens and poorly developed in 3 of 20 (15%).20
The MPFL is approximately 58 mm in length, with a width and thickness of 12 mm and 0.44 mm, respectively, at its midpoint.20
The MPFL fans out anteriorly, inserting on the proximal two-thirds of the patella.
The femoral attachment of the MPFL is posterosuperior to the medial femoral epicondyle and just distal to the adductor tubercle with the knee fully extended. The center of the anterior edge of the femoral attachment is located 9.5 mm proximal and 5.0 mm posterior to the center of the medial femoral epicondyle (FIG 1).20
In children with open physes, the femoral attachment of the MPFL has been reported to be 6.4 mm (2.9 to 8.5 mm) distal to the femoral physis.15
PATHOGENESIS
Patellar dislocations typically occur when the foot is planted, the knee is partially flexed, and the body pivots abruptly, resulting in internal rotation of the femur. Patients may or may not have sustained a direct blow.
Patients may report that something “popped out” medially, as the uncovered medial femoral condyle becomes prominent.
The knee usually gives way secondary to pain inhibition of the quadriceps and disruption of the mechanical advantage of the extensor mechanism, and the patient falls down.
If the knee remains flexed, the patella may remain dislocated over the lateral femoral condyle.
The history of injury may be unclear, especially if the patella rapidly and spontaneously reduced.
In one cohort of 189 patients, 61% of first-time dislocations occurred during sports activity.3
Individuals with trochlear dysplasia are typically more vulnerable to patella dislocation as the PFJ geometry is less suited to resist lateral translation of the patella, thereby shifting even more responsibility on the MPFL to restrain the patella.
Individuals with patella alta are also more vulnerable to patella dislocation as the degree of flexion at which the patella engages in the trochlea is higher than that in a normal knee. This reduced ability of PFJ geometry to resist lateral translation in the partially flexed knee shifts even more load onto the MPFL to restrain the patella.
NATURAL HISTORY
Fithian et al10 reported a 17% incidence of redislocation in a cohort of first-time dislocators followed over 2 to 5 years.
On the other hand, patients presenting with recurrent patellar instability are much more likely to continue experiencing additional dislocations than patients who present with their first dislocation.
The risk of a repeat dislocation in patients presenting with a history of prior patellar dislocation is about 50% over a 2- to 5-year period.10
The strongest risk factor for recurrent patellar instability is a history of prior patellar subluxation or dislocation.10
It is unclear whether patellar dislocation leads to premature arthritis.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient should be asked about mechanical symptoms such as locking or catching. Osteochondral loose bodies off the medial patellar facet or lateral trochlea (kissing lesion), impaction fracture of the lateral femoral condyle, or avulsion fragments off the medial patella may occur after patellar dislocation.
Physical examination should include the following:
Lateral-medial patellar translation. Increased laxity is signified by more than two quadrants of translation, 10 mm or more of lateral translation, or the absence of an end point.
Apprehension sign. Inability to fully translate the patella laterally because of patient guarding may lead to a falsenegative result.
J sign. The patella abruptly translates laterally as the knee is fully extended, moving in an upside-down “J”pattern.
Checkrein sign. A positive test (no end point) signifies MPFL laxity (analogous to a Lachman test).
Patellar facet palpation. Tenderness may indicate an osteochondral or avulsion injury.
Medial retinacular palpation. Tenderness may indicate retinacular injury. A palpable defect may be felt in the retinaculum or near the VMO.
Effusion. A tense effusion or hemarthrosis on aspiration after acute dislocation should raise suspicion for an osteochondral fracture. Magnetic resonance imaging (MRI) or arthroscopy should be considered.
A comprehensive physical examination of the knee is vital to evaluate for associated injuries such as cruciate or collateral ligament disruption.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Recommended plain radiographs include a standing anteroposterior view, a true lateral view with the knee flexed 30 degrees, and a standard axial patellar view at 30 or 45 degrees flexion.
On the lateral radiograph, patellar height is measured according to the method of Caton and Deschamps (ie, the ratio between the distance from the lower edge of the patellar articular surface to the upper edge of the tibial plateau and the length of the patellar articular surface).3
A ratio of 1.2 or greater indicates patella alta, which predisposes to patellar instability due to late engagement of the patella in the trochlea as the knee flexes.
If present, a tibial tubercle osteotomy and distalization should be considered.
Trochlear morphology can be assessed on a true lateral radiograph (the posterior borders of both femoral condyles are strictly superimposed).
Trochlear dysplasia is evident when the floor of the trochlea crosses the anterior border of both femoral condyles (crossing sign)6 (FIG 2A).
Alternatively, the positive trochlear prominence (ie, the sagittal distance between the trochlear groove and the anterior femoral cortex) on the lateral view has been shown to correlate well with trochlear dysplasia6,7 (FIG 2B). A trochlear groove prominence of 3 mm indicates trochlear dysplasia (FIG 2C).
The axial patellar view may demonstrate lateral patellar subluxation or even frank dislocation. It may demonstrate medial patellar avulsion fractures, although these can be missed on plain x-rays.
Stress radiography has been advocated to demonstrate abnormal patellar mobility.
With the knee flexed to 30 degrees, an axial patellar view is taken with a laterally directed force applied to the medial side of the patella.
Measurements are made on both the symptomatic and asymptomatic knees.
A side-to-side increase of 3.7 mm or more of lateral translation on the symptomatic versus asymptomatic side is considered abnormal.27
MRI identifies osteochondral injuries on the patella and femur as well as loose bodies that may be missed on plain radiographs.
A tense effusion should be aspirated. Presence of gross hemarthrosis on joint aspiration is an indication for MRI to assess for osteochondral fracture and loose body.
The TT-TG offset is the transverse distance between the anterior tibial tuberosity (TT) and the center of the trochlear groove (TG).6
It can be measured on axial computed tomography (CT) or MRI (FIG 2D), although some argue that these imaging modalities are not interchangeable as MRI has been reported to underestimate the TT-TG offset when compared with CT.2
Lateral offset of 20 mm or more should be corrected with medialization of the tibial tubercle.
MRI is also useful in identifying the location and degree of medial soft tissue injury preoperatively and has been reported to be even more accurate than arthroscopy in identifying MPFL injuries.1
MPFL injuries occur commonly in the form of tears near the femoral attachment or avulsions off the femur but may also occur as midsubstance tears or avulsions off the patella (FIG 2E,F). Injuries to multiple sites in the medial ligamentous complex occur.7
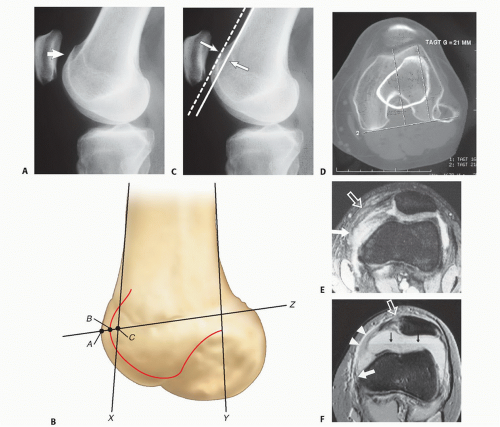 FIG 2 • A. On a true lateral radiograph, trochlear dysplasia is evident when the floor of the trochlea crosses the anterior borders of both femoral condyles (ie, the “crossing” sign). B. Measurement of the trochlear prominence on the lateral view according to Dejour et al6 X and Y are lines tangential to the anterior and posterior cortices of the distal femoral metaphysis, respectively. Line Z crosses the most prominent point of the line of the trochlear groove (point B) and the upper aspect of the posterior border of the condyles. Line Z crosses the anterior aspect of the lateral condyle (point A) and line X (point C). The distance BC (in mm) is the trochlear prominence. C. Lateral radiograph demonstrating a knee with positive trochlear prominence. Note that the floor of the trochlea lies anterior to the line tangential to the anterior cortex of the distal femur. D. Measurement of the tibial tuberosity-trochlear groove (TT-TG) offset, the transverse distance between the apex of the anterior tibial tuberosity and the center of the trochlear groove. Measurements are made on superimposed axial CT or MRI images. E,F. MPFL injury appearance on MRI. E. Transverse gradient echo image of the knee obtained at the level of the insertion of the adductor magnus tendon 3 weeks after lateral patellar dislocation demonstrates a complete tear of the femoral origin of the MPFL, with MPFL fibers retracted anteriorly (solid arrow). Partial injury, with surrounding edema, to the midsubstance of the patellar retinaculum (open arrow) also is seen. F. Transverse gradient echo image of the knee in a different patient 2 days after lateral patellar dislocation showing partial injury to the femoral origin of the MPFL. The MPFL fibers (solid white arrow) are wavy and show longitudinal split, and there is extensive surrounding edema. A complete tear (open arrow) is seen in the patellar insertion of the medial patellar retinaculum. A large joint effusion with layering (black arrows) is present, consistent with hemarthrosis. Note also the inferior fibers of the VMO (arrowheads).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|