Fig. 3.1

Fig. 3.2

Fig. 3.3
Fig. 3.4
An 11-year-old male roller hockey player fell onto his outstretched hand and complained of wrist pain.
Comments
Scaphoid fractures are rare in children and adolescents. The large amount of cartilage present in the scaphoid during development makes it less susceptible to fractures. Their incidence has increased, probably due to sports and leisure activity changes in the younger population.
Nonunion of pediatric scaphoid fractures are extremely uncommon. Although investigators have attributed this complication to missed or wrong diagnosis, nonunion may develop even in appropriately managed scaphoid fractures.
Clinical signs are swelling, painfully limited wrist motion, tenderness over the anatomical snuffbox, and pain with axial loading of the first ray.
Plain films are the initial radiological study of choice: posteroanterior, lateral, oblique, and posteroanterior with ulnar deviation views should be obtained.
If a scaphoid fracture is undetected on the initial radiographs, treatment should include immobilization in a short-arm thumb cast, followed by radiological reassessment after 2 weeks. MRI and CT could be useful in selected patients.
There is no agreement about the standard treatment method. Extended conservative treatment may be an alternative in the youngest adolescents, but most authors recommend internal fixation with iliac crest bone grafting.
Imaging Findings
The initial plain film was normal (Fig. 3.1). After a 2-week cast immobilization, a new radiograph was obtained and was also reported as normal (Fig. 3.2). Despite the patient being asymptomatic, his treating physician ordered a new radiograph after two further weeks. For unknown reasons, he did not return for follow-up until 6 months later. Radiograph (Fig. 3.3) showed nonunion of the scaphoid’s waist (arrow).
Coronal fat-suppressed T1-weighted image after intravenous gadolinium administration (Fig. 3.4) showed normal contrast enhancement in both fragments. Screw fixation with iliac crest bone grafting was performed with very good results.
Case 3.2: Early Closure of the Distal Tibial Physis Secondary to Epiphysiolysis Grade I

Fig. 3.5

Fig. 3.6

Fig. 3.7

Fig. 3.8
An 11-year-old football player suffered a right ankle sprain pain. The clinical examination showed pain, swelling, and a slight deformity. Sensitivity and pulses were preserved.
Comments
Epiphysiodesis (premature epiphysis/diaphysis union, resulting in growth cessation) is a rare complication of epiphysiolysis. Usually seen in Salter-Harris type IV and exceptionally in type I fractures (as in our case).
Epiphysiodesis can be central, peripheral, or longitudinal. It requires surgical intervention when the physeal bridge gives cause to a shortening greater than 2 cm affecting less than 50 % the size of the physis.
Imaging Findings
A right ankle radiograph (Fig. 3.5) showed a type I epiphysiolysis (arrows).
It was treated with a splint for 6 weeks. After removal, the patient presented good mobility with a slight ankle edema but no other symptoms.
Two weeks later, the patient returned, limping with pain and showing mild edema in his ankle.
A CT (Figs. 3.6 and 3.7) of the right ankle showed a concentric periosteal reaction at the distal tibial metaphysis, accompanied by sclerosis and bony bridge formation in the physis center (arrows).
As the patient was asymptomatic when the CT was performed, the treatment was conservative.
Two years later, a plain radiograph (Fig. 3.8) showed early closure of the right tibial metaphysis (as compared with the contralateral side) and 1 cm of dysmetria of the lower extremities. The patient was asymptomatic.
Case 3.3: Proximal Femur Epiphysiolysis

Fig. 3.9

Fig. 3.10
Fig. 3.11

Fig. 3.12
A 10-year-old female practicing rhythmic gymnastics presented with a history of limping for 1 month, which had worsened in the previous week and was accompanied by significant functional impairment. There was no clear history of trauma.
Comments
Epiphysiolysis, or slipped upper femoral epiphysis, is rare and is the result of chronic repetitive trauma to the proximal femoral growth plate.
The radiographic changes may be subtle. Frog-leg lateral views of the hip demonstrate displacement better than standard anteroposterior views.
Malalignment of the femoral neck and epiphysis could be difficult to detect in ultrasound although effusion fluid can be seen around the metaphysis.
Magnetic resonance imaging depicts the typical features with widening of the growth plate associated with high signal on STIR sequences.
Imaging Findings
Anteroposterior view of the pelvis was normal (Fig. 3.9), and although frog-leg views demonstrated a slipped capital upper femoral epiphysis (arrow) in the left hip (Fig. 3.10), it was reported as normal.
Due to persistent pain, new radiographs of the knee and hip were performed, which were also reported as normal.
The patient returned to the emergency room with persisting pain. On clinical examination, she described the fluctuating hip, outer thigh, and knee pain to have had a spontaneous onset without prior trauma or extra efforts. The pain increased at the beginning of activity. It decreased as the activity progressed, with rest and while sitting. There was no fever in this period. Patient’s pain showed moderate improvement with ibuprofen. She showed no other symptoms.
An ultrasound study (Fig. 3.11) detected a hip joint effusion (arrow).
With the suspicion of early Perthes disease, an MRI (T1-weighted coronal MR image) was performed (Fig. 3.12) showing widening of the left femoral physis (arrow), with minimal displacement, bone edema, and a joint effusion. A definitive diagnosis of proximal femur epiphysiolysis was made.
She underwent osteosynthesis with cannulated screws.
Case 3.4: Proximal Tibia Epiphysiolysis with Posterior Metaphyseal Fracture (Salter-Harris Type II)
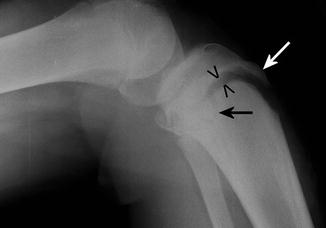
Fig. 3.13

Fig. 3.14

Fig. 3.15

Fig. 3.16
A 16-year-old basketball player complained of acute knee pain and movement restriction after jumping.
Comments
Proximal tibial fractures are not common in children. Proximal tibial conform about 1 % of all epiphysiolyses. Physeal fractures and tibial spine or tibial tubercle (TT) avulsions are more common in older children and adolescents and, in developed countries, are usually related to sports activity. The epiphyseal plate consists of several layers: reserve, immature, and mature proliferative-germinal layers and hypertrophic and calcification layers. The germinal layers are more attached to the epiphyseal bone; therefore, the physis rupture is easier at the metaphysical side and carries a lesser risk of growth disturbance (Salter-Harris types I and II). The proximal tibial epiphyseal plate closure is asymmetric, from posterior to anterior. Thus, in adolescents, the anterior part is weaker than the posterior one (more calcified). In basketball players, hurdlers, high jumpers, or gymnasts, for example, a quadriceps femoris sharp contraction to boost the jump may cause the anterior tibial epiphysiolysis (including anterior tibial tubercle). The patient failing to keep knee extension and landing with a flexed knee can cause the posterior metaphyseal fracture (Salter-Harris type II): Böhler’s injury mechanism “leap with a bad landing.” Another possible mechanism of injury is related to forced flexion against actively contracting quadriceps on landing after jumping. Patients present with pain, swelling, and deformity at the anteroinferior part of the knee, proximal patellar displacement, and quadriceps spasm. They are unable to move the knee or walk. The first author who classified the TT avulsion fracture by the fragment’s size was Watson Jones. Ogden described subtypes regarding intra-articular extension and TT comminution. However, Ryu in 1985 was the first to describe its association with a posterior metaphyseal fracture (type IV) (as seen in this case). Displaced fractures or intra-articular extension merit prompts referral to assess the need for osteosynthesis (Ogden IB, II, III). Little or undisplaced TT fractures (Ogden IA) can be treated nonsurgically: reduction and knee immobilization with a long-leg cast, as was this patient. Patients should be advised against returning to full sporting activity until they have regained 80–90 % of the quadriceps strength of the unaffected side.
Imaging Findings
Lateral radiograph (Fig. 3.13) shows proximal tibial anterior epiphysiolysis (arrowheads), with tibial tubercle (white arrow) extension. The posterior metaphyseal fracture (black arrow) is hardly seen. The flexed position is due to the patient’s inability for extending the knee.
Sagittal T2 spin-echo-weighted image shows good reduction of the epiphysiolysis and tibial tubercle avulsion with some residual edema (hyperintense signal) (arrows). No patella tendon tear (arrowhead) (Fig. 3.14) is seen.
Sagittal proton density spin-echo-weighted image shows the undisplaced thin posterior metaphyseal fracture (arrowheads) and the reduced anterior epiphysiolysis (arrow). No meniscus tear (Fig. 3.15) is seen.
Final sagittal T2 spin-echo-weighted image shows complete consolidation of the tibial tubercle (arrow) epiphysiolysis (arrowheads) without growth bone complication (Fig. 3.16).
Case 3.5: Traumatic Distal Femoral Bone Infarct

Fig. 3.17

Fig. 3.18
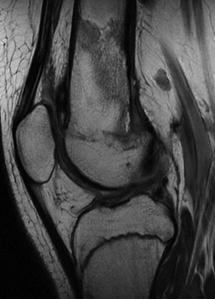
Fig. 3.19
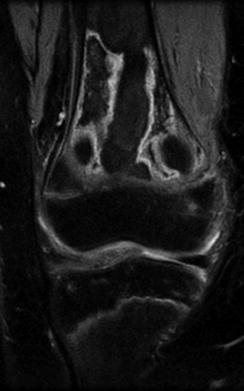
Fig. 3.20
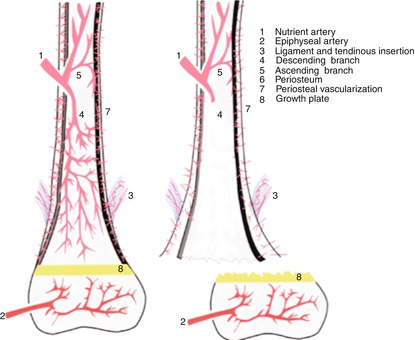
Fig. 3.21
A 14-year-old boy suffered a motocross accident. Physical examination showed significant right knee deformity and swelling, without distal neurovascular involvement.
Comments
Bone infarcts are due to vascular disorders. They are usually seen in the long bones’ metaphyseal regions, associated to underlying systemic conditions, such as sickle cell disease, lupus erythematosus, acute lymphocytic leukemia, non-Hodgkin lymphoma, and renal transplantation. Nevertheless, they can also be seen in the absence of related medical disease. Although rare, they can be found after a high-energy injury.
A suspected bone infarct diagnosis is not difficult on plain radiographs on the basis of its characteristic serpiginous appearance. However, diagnostic confirmation is not so easy, and differentiation with osteomyelitis and malignancy is mandatory.
MR findings of bone infarct are very characteristic, with a serpentine rim that corresponds to the reactive sclerosis seen on plain radiographs. In acute and subacute stages, the central infarct is equal to normal medullar fat signal and corresponds to avascular bone tissue. On MRI, both T1- and T2-weighted sequences show a thin, low-signal rim with a typical serpentine border. All these medullary changes are not seen on plain films, probably due to circumferential periosteal thickening. The reactive osteoblastic tissue implicated in peripheral bone consolidation and remodelation is responsible for this low T1 signal. T2-weighted fat-suppression images show peripherically bright serpiginous lesions due to edema. This set of characteristic MR findings can lead to the bone infarct diagnosis.
Long bones have three arterial inputs: (1) nutrient artery, (2) periosteal arteries, and (3) epiphyseal arteries (Fig. 3.21). Their main supply is through the nutrient artery.
Anastomoses between the nutrient and periosteal system can develop in response to injury. Damage to both nutrient and metaphyseal supply of the growing distal femur can result in marrow necrosis.
Long vascular anatomy in children differs from that in adults. The epiphyseal and metaphyseal vascular supply are independent of each other between ages 1 and 16. Distal metaphyseal trabecular bone vascularization depends on terminal branches from the nutrient artery and metaphyseal circulation. Epiphyseal supply, however, depends just on the epiphyseal artery. The barrier between both vascularization systems is the growth plate. Growth plate closure at about age 16 allows continuity between both systems.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








