This article focuses on comparing patient morbidity with harvesting bone graft for the treatment of nonunions from three different sites. Anterior iliac crest graft is the most commonly used site; however, the posterior iliac crest and intramedullary canal provide greater quantities of bone. The anterior and posterior iliac crests also have some donor site complications such as nerve injury and persistent pain. The intramedullary canal, when compared with anterior and posterior iliac crest, offers the largest quantity of bone graft with the least amount of patient donor site morbidity. The intramedullary canal also appears to be a bone graft source that can be reharvested, unlike the anterior and posterior iliac crest donor sites.
Autologous bone graft has always been the gold standard for treating nonunions secondary to the osteoinductive effect of the many bone morphogenetic proteins (BMPs) and the live osteoblasts. Traditionally, autologous bone graft for nonunions has been harvested from the anterior and posterior iliac crest. The iliac crest has many advantages including the availability of large quantities of bone without structural compromise to the extremity. The other advantage of iliac crest bone graft (ICBG), in addition to all the benefits of autologous bone graft, is its ability to be used as a tricortical structural graft. The disadvantages, however, have been well documented in the literature and include persistent donor site pain, numbness surrounding the donor site, infection, and fractures.
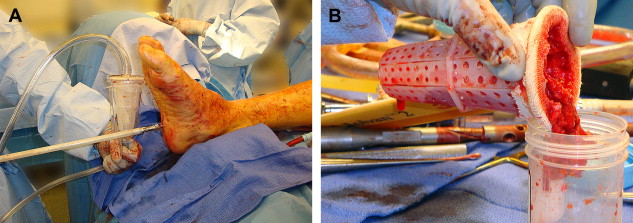
Recently, a new device, the Reamer/Irrigator/Aspirator (RIA) (Synthes, Inc, West Chester, PA), has been used to harvest autograft from the intramedullary canals of the femur and tibia. Intramedullary bone graft harvest allows for a fairly large volume of bone graft to be harvested when compared with the volume of graft obtained from the iliac crest; however, it also has the advantage of less donor site morbidity. The following article addresses in detail the advantages and disadvantages of obtaining bone graft from the iliac crest versus the intramedullary canals. Specifically, this article will discuss the volume and quality of graft obtained, harvest time, blood loss, postoperative pain, functional impairment, major and minor complications, and the potential for repeat harvesting.
Bone graft volume
Graft volume is a critical consideration when choosing a donor site for autograft. Larger bone graft volumes are needed for segmental defects, and each donor site has a limited supply. Also, regardless of donor site, the bone quality of the patient has a significant impact on the amount of bone graft available with a larger amount of bone available in a young, healthy patient. Some studies have suggested that when a larger volume of graft is harvested from the anterior or posterior iliac crest, the donor site morbidity increases.
Anterior ICBG volume has been reported to range from an average of 5.3 cm 3 (Bruno and colleagues) to 72 cm 3 (Marx and Morales). Five studies have been published on anterior iliac crest bone graft volume that focus on nonspine usage. Hall and colleagues reported the average volume of compressed cancellous bone was 12.87 cm 3 (range, 6.6–18.6 cm 3 ) in elderly cadaveric specimens. Kessler and colleagues measured cancellous bone harvested from between the anterior iliac tables and reported an average volume of 9 cm 3 (range, 5–12 cm 3 ) with an average patient age of 44 years (range, 8–80 years). Ahlmann and colleagues reported an average volume of 54.3 cm 3 (no range reported), but they included the use of the outer cortical table, which was then converted into chips and measured using a medicine cup and syringe. The average age in their study was 46.2 years (range, 12–77 years). The addition of cortical bone graft from the outer table significantly increased the volume obtained. Marx and Morales harvested anterior ICBG for large jaw defects from patients who were 18 to 75 years old. The mean noncompressed volume was 72 cm 3 .
Posterior ICBG has been traditionally used when larger volumes of bone graft are necessary. Kessler and colleagues reported an average cancellous bone graft volume of 25.5 cm 3 (range, 17–29 cm 3 ) from the posterior iliac crest. Kessler and colleagues harvested an average of only 9 cm 3 from the anterior iliac crest, which gives the posterior crest a distinct volume advantage. Hall and colleagues reported a similar volume of compressed cancellous bone graft with an average of 30.31 cm 3 (range, 27.1–34 cm 3 ). The average posterior ICBG volume in the Ahlmann and colleagues study was 55.12 cm 3 ; however, this also included cortical strips, which significantly increased the available graft volume. Marx and Morales reported an average posterior ICBG harvest of 88 cm 3 . The posterior ICBG harvest contained significantly more bone than the anterior ICBG harvest (mean, 72 cm 3 ) ( P <.05).
Belthur and colleagues reported an average intramedullary femoral bone graft volume of 41.1 cm 3 (range, 25–75 cm 3 ) with an average patient age of 44.9 years (range, 15–78 years). Scharfenberger and Weber reported an average femoral intramedullary graft volume of 68 cm 3 (range, 40–90 cm 3 ) with a much younger average patient age of 34 years (range, 16–53 years). Belthur and colleagues also reported an average tibial graft volume of 32.5 cm 3 (range, 25–50 cm 3 ) ( Fig. 1 ). Graft volume in femoral and tibial cases is directly dependent on the size of the reamer head chosen for the harvest as well as the patient age. Larger volumes can be harvested with larger reamer heads, but the torsional stability of the canal is compromised if more than the inner 2 mm of cortical bone is resected.
On average, intramedullary bone graft has more graft volume than anterior ICBG and has at least similar bone graft volumes when compared with posterior ICBG ( Table 1 ). In the younger population, intramedullary bone graft might provide larger volumes than posterior ICBG.
| Anterior Iliac Crest Harvest Site | Posterior Iliac Crest Harvest Site | Intramedullary Canal Harvest Site | |
|---|---|---|---|
| Volume of graft obtained | 5–72 cm 3 | 25–88 cm 3 | 25–90 cm 3 |
| Time to harvest | 35 min | 40 min + 20 min for repositioning | 30 min |
| Volume of blood loss | Greater than posterior | Less than anterior | Unknown |
| Acute and chronic pain | Greatest | Intermediate | Least amount of pain |
| Duration of gait abnormalities | 3–4 weeks | 2 weeks | 1 week |
| Rate of major complications | Highest rate | Intermediate rate | Lowest rate |
| Rate of minor complications | Highest rate | Intermediate rate | Lowest rate |
| Advantages of harvest site | Tricortical support; no repositioning | Tricortical support; good bone graft volume | Large concentration of growth factors; good bone graft volume; minimal complications |
| Disadvantages of harvest site | Small volume; pain; greatest number of complications | Increased intraoperative time with repositioning | Nonstructural bone graft |
Bone graft quality
Few studies have compared graft “quality” or the presence of viable cells and growth factors. Frölke and colleagues determined that there are live osteoblasts in cortical reamings of sheep femora. Schmidmaier and colleagues compared the quantity of BMPs in the crest graft versus the intramedullary graft. They reported significantly elevated levels of fibroblast growth factor-alpha (FGFa), platelet-derived growth factor (PDGF), insulin-like growth factor 1 (IGF-1), transforming growth factor beta 1 (TGF-B1), and BMP-2 in the reamings of the intramedullary femoral canal when compared with bone graft from the iliac crest. These studies are encouraging with respect to the quality of the intramedullary graft harvested; however, more research is required to see if these advantages are of clinical significance.
Bone graft quality
Few studies have compared graft “quality” or the presence of viable cells and growth factors. Frölke and colleagues determined that there are live osteoblasts in cortical reamings of sheep femora. Schmidmaier and colleagues compared the quantity of BMPs in the crest graft versus the intramedullary graft. They reported significantly elevated levels of fibroblast growth factor-alpha (FGFa), platelet-derived growth factor (PDGF), insulin-like growth factor 1 (IGF-1), transforming growth factor beta 1 (TGF-B1), and BMP-2 in the reamings of the intramedullary femoral canal when compared with bone graft from the iliac crest. These studies are encouraging with respect to the quality of the intramedullary graft harvested; however, more research is required to see if these advantages are of clinical significance.
Harvest time
Harvest time is a significant factor when choosing an autograft donor site because the bone graft harvest is just one portion of the procedure. Consideration must be given to the location of the recipient site and the additional time necessary for reprepping and draping if the patient needs to be repositioned after the harvest. Kessler and colleagues recorded the average time for harvesting anterior and posterior ICBG. The average anterior iliac crest harvest time was 35 minutes (range, 22–48 minutes), and the average posterior iliac crest harvest time was 40 minutes (range, 32–55 minutes) with an additional average repositioning time of 20 minutes (range, 14–27 minutes). Marx and Morales compared anterior harvest times to posterior harvest times. The average posterior harvest time was 106 minutes versus 134 minutes for the anterior harvest time ( P <.08). There was no mention as to whether repositioning time was included in the posterior harvest.
No formally published studies have recorded the harvest time for the intramedullary femoral graft; however, Belthur and colleagues reported the average intramedullary graft harvest time as 30 minutes (no range reported). The additional advantage of the intramedullary harvest is that even if the contralateral side is harvested, there is no reprep-ping and repositioning necessary as long as the surgical procedure is performed in the supine position. Nichols and colleagues reported a case of intramedullary bone graft harvest for posterior lumbar fusion in which the intramedullary harvest was performed in the prone position, thus eliminating the need for additional reprepping and draping in these cases.
Intramedullary harvest had the shortest harvest time followed by the anterior iliac crest (see Table 1 ). It is difficult to use the data from the Marx and Morales study because there was no mention of repositioning the patient after the posterior crest harvest. This repositioning would be a necessary part of their procedure because they were using the large posterior graft harvests for large jaw defects.
Blood loss
Two studies have reported the estimated blood loss after ICBG harvest. Ahlmann and colleagues reported the average intraoperative blood loss from posterior ICBG harvest as 75 mL with the total blood loss including the postoperative drain as 169.14 mL. Anterior ICBG harvest intraoperative blood loss was also 75 mL, but when the drain output was added, the total blood loss was 232.47 mL. In this study, the posterior iliac crest harvest had significantly less blood loss ( P ≤.018). Marx and Morales also compared posterior ICBG harvest blood loss with anterior ICBG harvest blood loss. This blood loss estimate included the sponge weights, suction canister volume, and drain output. Posterior crest blood loss averaged 306 mL versus 474 mL for the anterior crest blood loss ( P <.001).
With respect to intramedullary bone graft harvest, Scharfenberger and Weber used hemoglobin and hematocrit to estimate blood loss after intramedullary harvest in 11 patients. The average hemoglobin drop was 4.3 g/dL (range, 2.3–8.0 g/dL) and the average hematocrit drop was 11% (range, 6%–22%). These data might be altered by the recipient site bleeding and the dilutional effect that the intravenous fluids have on the measurement of hematocrit and hemoglobin. At present, it is difficult to quantify the blood loss after the use of the intramedullary harvesting device and should be the subject of further study.
Postoperative pain
Multiple studies have documented postoperative pain after anterior and posterior iliac crest graft harvest. Many of these studies are in conjunction with spine surgery ; however, this section will concentrate on indications other than spine when possible. Donor site pain is underappreciated by the surgeon as shown in a study by Heary and colleagues. Heary and colleagues reported on surgeon perception of persistent donor site pain versus patient perception of persistent donor site pain after spinal surgery. Neurosurgeons appreciated donor site pain only 8% of the time as opposed to the actual incidence of donor site pain reported by patients as 34%.
With respect to acute pain (ie, immediately postoperative or within 1 to 2 months following surgery), a large number of authors report limited activity secondary to pain. According to DeOrio and Farber who studied pain after harvest from the anterior iliac crest, the acute pain on a 10-point visual analog scale (VAS) averaged 3.8 points (range, 0–10 points) with 108 (84%) of 128 patients limiting their activity because of pain for 4 weeks or less. Belthur and colleagues also reported acute anterior iliac crest pain using a visual analog scale for frequency and intensity for a maximum total pain score of 20 points. The immediate postoperative pain score obtained at less than 48 hours averaged 12.13 points (range, 9–18 points), and the postoperative pain score obtained less than 3 months after surgery averaged 8.61 (range, 3–15 points). The scores from patients who underwent anterior ICBG harvest were all significantly higher when compared with the intramedullary harvest groups during the same time intervals ( P <.001). Marx and Morales compared anterior ICBG harvest with posterior ICBG harvest in the acute (day 1 and day 10) postoperative period and showed that the anterior crest donor site was more acutely painful. On postoperative day 1, the mean pain score (on a 10-point VAS) for the anterior harvest was an average of 7.2 ± 1.6 versus an average of 3.1 ± 0.7 for the posterior harvest ( P <.005). On postoperative day 10, the average score anteriorly was 4.4 ± 0.5 versus an average of 0.3 ± 0.3 posteriorly ( P <.005).
Most authors also reported some encouraging statistics with respect to resolving acute pain. Three studies found that 70.0% to 92.2% of acute pain symptoms from anterior ICBG harvest resolved within 4 weeks. DeOrio and Farber reported that 118 of 128 patients had total resolution of their pain at 8 weeks. Weatherby and colleagues reported acute donor site pain following intramedullary graft harvest for nonunion lasting 40 days in only 5 (23%) of 24 patients.
Chronic pain (ie, pain lasting longer than 3 months) is a problem for a small percentage of patients after harvest from the anterior iliac crest. Cricchio and Lundgren reported that 8 (11%) of 70 patients had pain after 2 years and DeOrio and Farber reported that 4 of 128 patients had pain for more than 7 months. Silber and colleagues reported anterior donor site pain after a one-level anterior cervical discectomy and fusion. Thirty-five of 134 patients had chronic pain at the donor site with a mean VAS score of 3.8 points. Fifteen of 134 patients in this study used pain medication for their donor site, and 7 of 134 patients had chronic discomfort with their clothing. Belthur and colleagues also found that chronic pain scores using a VAS for frequency and intensity were significantly higher in the anterior iliac crest group after 3 months with an average of 1.30 points (range, 0–10 points) versus 0.10 points (range, 0–4 points) for the intramedullary harvest group ( P <.001).
With respect to acute pain following posterior ICBG harvest, Kessler and colleagues reported that 15 (33%) of 46 patients had acute pain that resolved during the following month. No patients in the Kessler and colleagues study experienced chronic pain. Mirovsky and Neuwirth documented postoperative pain using two different methods of posterior iliac crest harvesting. One group (Group A) had bone harvested from the outer table with underlying cancellous bone, and one group (Group B) had cancellous bone harvested from between the tables. Fourteen (56%) of 25 patients in Group A and 12 (52%) of 23 patients in Group B had acute pain during the first week. This number gradually declined during the following 12 months to 6 (24%) of 25 patients in Group A and 4 (17%) of 23 patients in Group B. Chronic pain at 24 months was present in 5 (20%) of 25 patients in Group A and 4 (17%) of 23 patients in Group B.
To summarize the pain data, the anterior iliac crest harvest had more acute pain when compared with posterior iliac crest and intramedullary bone graft harvest (see Table 1 ). No study exists in the literature that compares posterior crest graft with intramedullary graft, so it is difficult to say which one of these sites is less painful. In my opinion, the intramedullary harvest is ultimately less painful secondary to the very small (1–2 cm) incision required for harvest and the ability to harvest bone without any muscle dissection off of the bone as in the posterior crest harvest. It is interesting to note that in the Belthur and colleagues study, six patients underwent anterior ICBG harvest and intramedullary harvest at two different points in time. All six patients said that the intramedullary graft harvest was much less painful in all time periods when compared with their previous anterior ICBG harvest. With respect to the chronic pain data, intramedullary donor site has the least amount of chronic pain followed by the posterior iliac crest and then anterior iliac crest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







