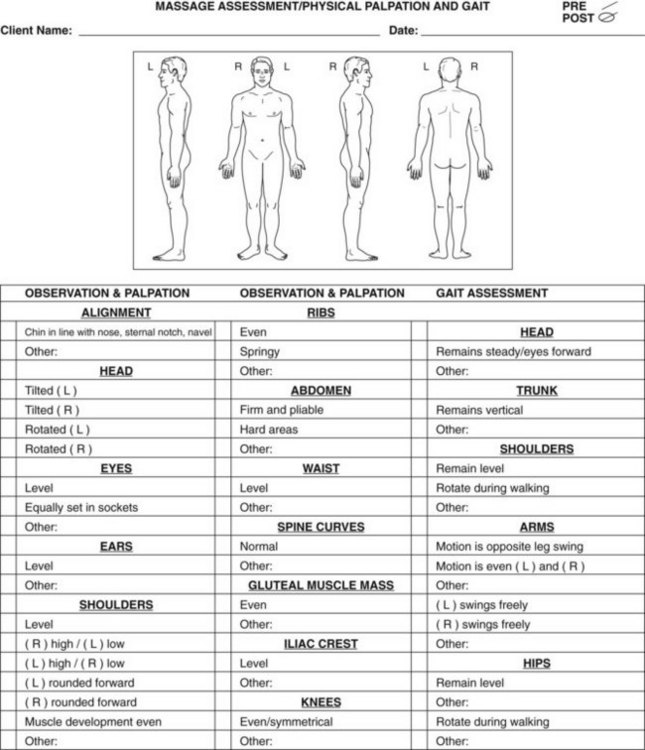
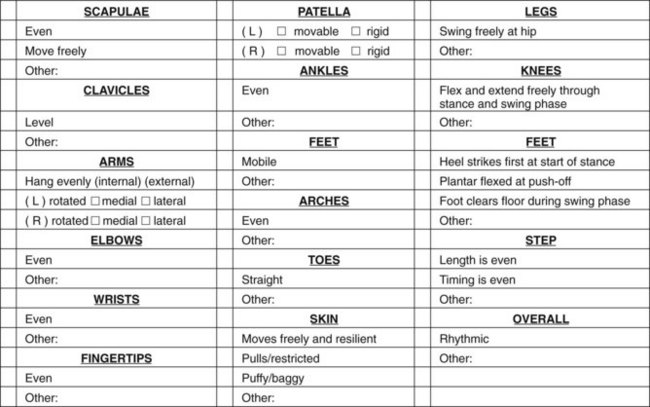
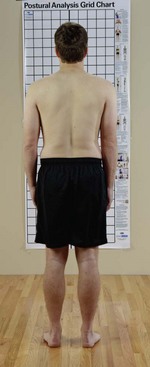
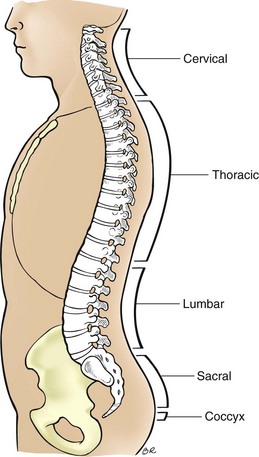
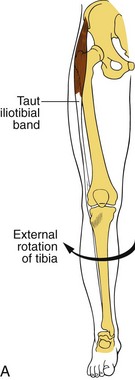
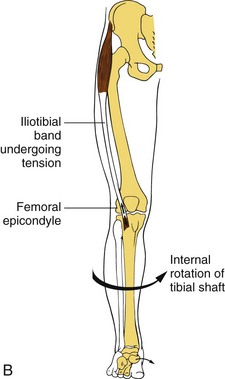
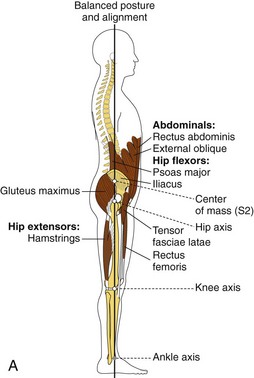
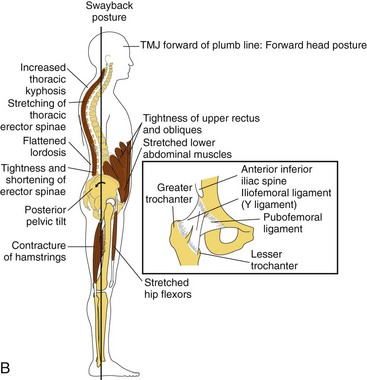
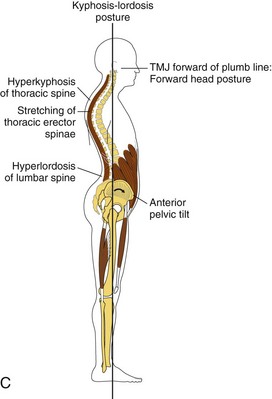
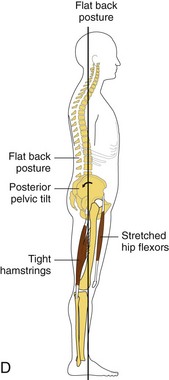
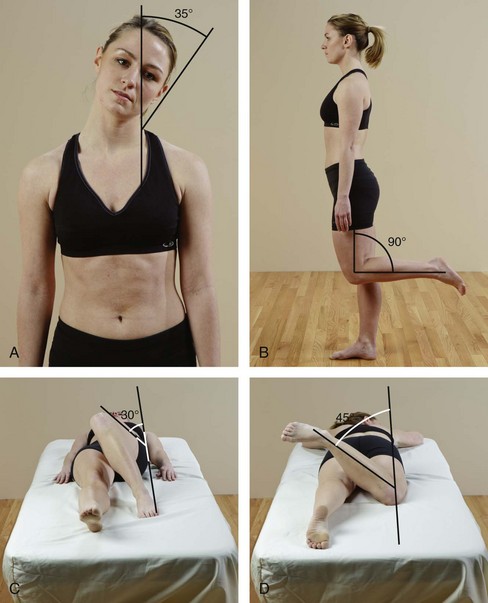
Chapter 10 Outcome Goals and Care or Treatment Plans Assessment Using Joint Movement Kinetic Chain Assessment of Posture Palpation of the Skin and Superficial Connective Tissue Palpation of Superficial Connective Tissue Only Palpation of Vessels and Lymph Nodes Palpation of Abdominal Viscera Understanding Assessment Findings Organizing Assessment Information into Treatment Strategies After completing this chapter, the student will be able to perform the following: 1 Describe assessment for the sport and fitness population. 2 Apply a clinical reasoning process to treatment plan development. 3 Develop outcome goals that are quantifiable and qualifiable. 4 Adapt charting methods to the athletic population. 5 Complete a comprehensive history. 6 Complete a comprehensive physical assessment. 7 Perform postural assessment. 8 Perform basic orthopedic tests to assess for joint injury. 9 Analyze movement assessment findings. 10 Perform muscle strength assessment. 11 Describe and assess kinetic chain function. 13 Perform palpation assessment. 14 Integrate clinical reasoning into the treatment plan using assessment findings. 15 Relate assessment data to first-degree, second-degree, and third-degree dysfunction, and categorize the adaptation response to stage 1, 2, or 3 pathology. 16 Integrate ongoing assessment data channeled into appropriate massage treatment strategies. This text assumes that the reader already has completed a comprehensive therapeutic massage course of study that included assessment procedures such as history taking, physical assessment, treatment plan development, and charting.1 The following procedures are recommended for targeting this specific population. • Surgery or medical procedures • Therapeutic exercise activities • Physical therapy intervention • Training types such as strength and conditioning and agility • Cognitive load (how much mental training required) • Practice and training schedules • Has the client hurt the area before? • How did the client hurt the area? • What was heard when the injury occurred—a crack, snap, or pop? • How bad was the pain and how long did it last? • Is there any sense of muscle weakness? • How disabling was the injury? • Could the client move the area right away? • Was the client able to bear weight for a period of time? • Has a similar injury occurred before? • Was there immediate swelling, or did the swelling occur later (or at all)? For an athlete with a chronic condition, ask the following: • What was the nature of the injury (trauma or repetitive use)? • What is the nature of the pain—hot, pokey, sharp? • When does the pain occur—when bearing weight or after activity? • What injuries have occurred in the past? • What first aid and therapy, if any, were given for these previous injuries? Ask the client to point to as well as explain the area of complaint. Is the client getting better, worse, or is the client in need of a referral? The following are common gestures: • A finger pointing to a specific area suggests an acupressure or motor point hyperactivity or a joint problem. What the pointing means depends on the area indicated. • If the finger is pointed to a specific area and then the hand swipes in a certain direction, it may be a trigger point problem. • If the area is grabbed, pulled, or held and is moved as if being stretched, this often indicates muscle or fascial shortening. • If movement is needed to show the area of concern, the area may need muscle lengthening combined with muscle energy work to prepare for the stretch and reset of neuromuscular patterns. • If the client moves into a position and then acts as if stuck, the area may need connective tissue stretching. • If the client draws lines on his body, this may indicate nerve entrapment in the fascial planes or grooves. The more serious the condition, the longer it will last. Other terms used to describe symptoms include the following: Sharp, stabbing, tearing describes a more severe injury to the musculoskeletal system or a nerve root condition. This type of sensation is experienced with muscle or ligament tears, especially when the muscle or ligament is being used. The sensation is usually relieved at rest. A nerve root inflammation can elicit a sharp or stabbing pain, independent of movement. Tingling, numbing, picky describes a nerve compression near the spine or in the extremities, or a circulation impairment. Throbbing, hot is associated with acute injury inflammation and swelling, such as an abrasion puncture wound or an acute bursitis. Severe throbbing is a contraindication to massage. Gripping, cramping is typically used to describe a serious condition, often a nerve root injury or a visceral condition. Gripping and cramping pain is a contraindication to massage and requires referral to a doctor. The client can choose from the following descriptors: • What activities make the condition worse—moving, sitting, standing, walking, or resting? • What sport movement is affected—running, jumping, cutting, swinging, acceleration, or deceleration? Clarifying assessment questions to ask include the following: In general, physical assessment includes the following: • Head: neutral position neither tilted nor rotated • Shoulders: level, not elevated or depressed • Scapulae: neutral position, medial borders essentially parallel and approximately 3 to 4 inches apart • Thoracic and lumbar spines: straight • Pelvis: level with both posterior superior iliac spines in same transverse plane • Hip joints: neutral position neither adducted nor abducted or rotated (internal or external) • Head: neutral position, not tilted forward or backward • Cervical spine: normal curve, slightly convex to anterior • Scapulae: flat against upper back • Thoracic spine: normal curve, slightly convex to posterior • Lumbar spine: normal curve, slightly convex to anterior • Pelvis: neutral position, anterior superior iliac spine in same vertical plane as symphysis pubis • Hip joints: neutral position, leg vertical at right angle in sole of foot Chart the findings and relate them to the client’s history (Figure 10-1). For the physical assessment, the main considerations are body balance, efficient function, and basic symmetry (Box 10-1). When assessing posture, it is important for the massage therapist to notice the complete postural pattern. Most compensatory patterns occur in response to external forces imposed on the body. However, if the client has had an injury, maintains a certain position for a prolonged period, or overuses a body area, the body may not be able to return to a normal dynamic balance efficiently. The balance of the body against the force of gravity is the fundamental determining factor in a person’s posture or upright position. Even subtle shifts in posture demand a whole body compensatory pattern (Figure 10-2). Cervical, thoracic, lumbar, and sacral curves develop because of the need to maintain an upright position against gravity (Figure 10-3). Postural dysfunction occurs in the three planes of movement (sagittal, frontal, and transverse), as well as in supination and pronation (Figures 10-4 and 10-5). FIGURE 10-4 A, Ideal posture. B, Swayback posture. C, Kypholordotic posture. D, Flat back posture. Effects of postural imbalance. (Modified from Saidoff DC, McDonough AL: Critical pathways in therapeutic intervention: extremities and spine, St Louis, 2002, Mosby.) Remember that each person is unique, and many factors influence available range of motion. Just because a joint does not have the textbook range of motion (ROM) does not mean that what is displayed is abnormal. Abnormality is indicated by nonoptimal function. This can be seen as a limitation or an exaggeration in the “textbook normal” range of motion (Box 10-2). ROM is measured in degrees. Joint movement is measured from the neutral line of anatomic position. Movement of a joint in the sagittal, frontal, or transverse plane is described as the number of degrees of flexion, extension, adduction, abduction, and internal and external rotation (Figure 10-6). For example, the elbow has approximately 150 degrees of flexion at the end range and 180 degrees of extension. Anything less than this is hypomobility, and anything more is considered hypermobility. Massage therapists typically estimate degrees of movement, and other professionals use specific equipment to obtain precise information. The normal ROM of joints is found in anatomy texts such as Mosby’s Essential Sciences for Therapeutic Massage. FIGURE 10-6 Examples of approximate degrees of movement. A, 35 degrees of lateral flexion. B, 90 degrees of knee flexion. C, 30 degrees of internal hip rotation. D, 45 degrees of external hip rotation.
Assessment for Sports Massage and Physical Rehabilitation Application
Assessment Details
History
Gestures
Symptoms
![]() See the Evolve website that accompanies this book for an example of a history taking form.
See the Evolve website that accompanies this book for an example of a history taking form.
Physical Assessment
Physical Assessment of Posture
Standard Posture Front View
Standard Posture Back View
Standard Posture Side View
Active Movements
![]() Log on to your Evolve website to watch Video 10-1: Multiplanar Assessment (Functional Assessment).
Log on to your Evolve website to watch Video 10-1: Multiplanar Assessment (Functional Assessment).
Range of Motion
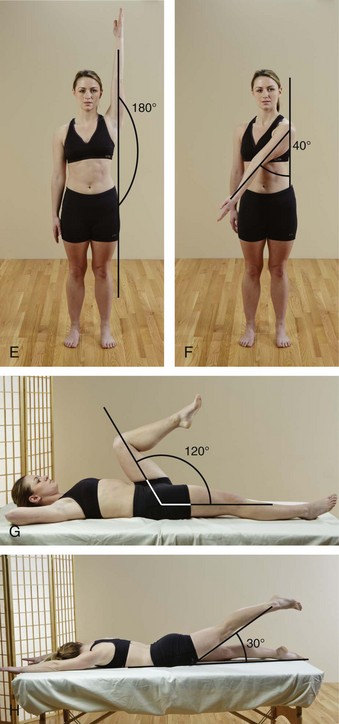
E, 180 degrees of shoulder abduction. F, 40 degrees of horizontal shoulder adduction. G, 120 degrees of hip flexion. H, 30 degrees of hip hyperextension.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Assessment for Sports Massage and Physical Rehabilitation Application
Only gold members can continue reading. Log In or Register to continue