Anatomy and Kinematics of the Hip
Mark R. Hutchinson MD
John Hung MD
J.W. Thomas Byrd MD
Normal range of motion of the hip is measured from a neutral or anatomic position of erect posture with the toes pointed forward.
The presence of labral tears is directly associated with degenerative changes in adjacent articular cartilage.
Labral tear location should be described as anterior, superior, or posterior and, if possible, peripheral or central. Tears may also be described as longitudinal, radial, or flap tears.
The muscles crossing the hip joint are some of the most powerful in the body. Twenty-two muscles cross the hip joint and provide motor power for functional range of motion, balance, and gait.
Both supine and lateral positions in arthroscopy require some element of traction along the femur to open the joint space; therefore, both have a risk of pudendal nerve palsy due to excessive traction against a perineal post.
The hip joint is an important link in the kinetic chain connecting the lower extremity to the core. It must have the structural integrity to assume the loads of body weight not only through static stance but also through a myriad of dynamic activities such as walking, climbing, running, and jumping. The hip must also be both flexible and powerful. Normal range of motion is measured from a neutral or anatomic position of erect posture with the toes pointed forward. From this position, the normal hip can flex 120 to 130 degrees, extend 15 to 30 degrees, adduct 25 to 30 degrees, abduct 30 to 50 degrees, externally rotate 40 to 60 degrees, and internally rotate 30 to 40 degrees. Extremes of motion are limited by bony anatomy, ligamentous and capsular restraints, and active motor tension. Coordinated motor power of the muscles that cross the joint is essential for balance, normal gait, and transferring energy up the kinetic chain. Indeed, the muscles crossing the hip joint are some of the most powerful in the body.
The purpose of this chapter is to review the anatomy of the hip as it relates to orthopaedic sports medicine and arthroscopy. Anatomy is the foundation of diagnosis, physical examination, and successful surgical intervention. This chapter will cover in sequence superficial anatomic landmarks; bony anatomy including facets of the pelvis, acetabulum, and proximal femur; capsule, labrum, and ligamentous structure; muscle tendon units that cross the hip joint and power motion; associated bursae including the trochanteric bursa and iliopsoas bursa; and neurovascular structures that supply the anatomic structures about the hip and are at risk during surgical and arthroscopic approaches (Fig 25-1). The final section will be dedicated to the unique perspective of anatomy from an arthroscopic point of view.
Superficial Anatomic Landmarks
Superficial bony landmarks assist in the examination of the hip to specifically identify pathology and to guide safe surgical approaches and portal placement. The anterior and posterior surfaces of the pelvis are an obvious delineation between anterior and posterior structures. Laterally, the border can be palpated from the border of the iliac crest, the anterior superior iliac spine, and the greater trochanter. Medially, the delination between anterior and posterior
structures extend distally from the symphysis pubis along the palpable superficial adductor, the gracilis.
structures extend distally from the symphysis pubis along the palpable superficial adductor, the gracilis.
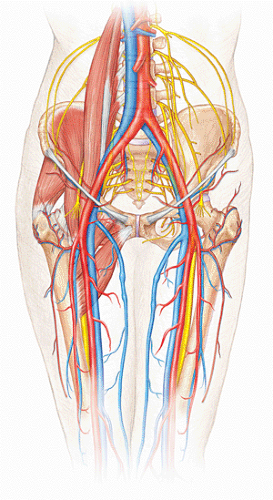 Fig 25-1. Anterior perspective of the hip demonstrates the relationship of bone structure, muscles, nerves, arteries, and veins about the hip. |
Additional superficial anatomic landmarks anteriorly include the hip flexion crease, the palpable inguinal ligament (creating the roof of the femoral triangle), and the femoral artery (palpated by pulse) (Fig 25-2). The obvious superficial anatomic landmark laterally is the greater trochanter, which serves as the insertion point of the hip abductors and defines the site of trochanteric bursitis when present. The anterior edge of the tensor fascia lata can frequently be palpated with internal and external rotation of the hip as it passes over the greater trochanter. Posteriorly, important palpable landmarks include the spinous processes of the lumbo-sacral spine, the posterior superior iliac spine, the sacroiliac joints, the ischium serving as insertion of the hamstring musculature, and the sciatic notch, which can relatively be assessed as a soft spot medial and superior to the ischium deep to the gluteal musculature.
Bone Anatomy/Osteology
The pelvis is a complex structure composed of bony and ligamentous constructs. There are two inominate bones connected at the pubis symphysis, in addition to their interconnections with the sacrum. The inominate bones are composed of three components: ilium, ischium, and pubis. These bones converge to form the acetabulum, which articulates with the femoral head to comprise the hip joint (Fig 25-3). The bony pelvis is maintained structurally by dense ligamentous structures. The formation of the sacroiliac joint is one of excellent stability due to the expanse of the articular surfaces as well as the broad extensive ligamentous structures that make up the sacroiliac joint. The ligaments that provide the structural stability include the interosseus sacroiliac ligaments, posterior sacroiliac ligaments, anterior sacroiliac ligaments, and the sacrotuberous, sacrospinous ligaments. Posteriorly, the construct of the ligaments act in the same way suspension bridges function. The posterior superior iliac spines act as the pillars, the interosseus ligaments serving as the suspensory bars, and the sacrum acts as the bridge.
The acetabulum is described as an incomplete hemisphere and serves as the socket for this classic diarthrodial, ball and socket joint. The articular surface is shaped like a horseshoe surrounding the nonarticular cotyloid fossa (Figs 25-4 and 25-5). The socket is supported by the anterior and posterior columns of bone oriented in an inverted Y-shape. The posterior column is composed of the ischium, the ischiala spine, the posterior half of the acetabulum, and the dense bone of the sciatic notch. The anterior column is composed of the anterior iliac crest, the anterior iliac spines, the anterior half of the acetabulum, and the pubis. The inferior aspect of the acetabulum (the lower two limbs of the horseshoe) is connected by the transverse ligament, which plays an important role in maintaining joint congruity and accepting transfer loads across the joint.
The acetabulum is obliquely oriented in the coronal plane 45 degrees to the floor and is usually anterior-faced (anteverted) at about 15 degrees. The anteversion is directly affected by the amount of pelvic tilt or rotation in the sagittal plane. With increased pelvic tilt the relative anteversion increases and with loss of pelvic tilt the acetabulum can actually face posteriorly. With neutral pelvic alignment, anteversion ranges from 5 to 20 degrees in men and 10 to 24 degrees in women (1,2,3).
The weight-bearing surface of the acetabulum is the dome or roof. This portion supports the femur during normal standing. This dome can be defined as the area encompassed by a 45-degree arc with a central axis through
the superior pole of the acetabulum. This area must be intact for adequate support in weight bearing through the acetabulum.
the superior pole of the acetabulum. This area must be intact for adequate support in weight bearing through the acetabulum.
The femoral head is a spherical structure that serves as the ball of the ball and socket joint and is predominantly covered by articular hyaline cartilage. A fovea sits centrally and superiorly on the articular surface and serves as the insertion of the ligamentum teres (Fig 25-4). The femoral neck is anteverted between 8 to 14 degrees in relation to the femoral condyles. This angle is determined by the femoral neck and the transcondylar axis of the knee. The femoral neck shaft angle averages 127 to 135 degrees (with angles >135 degrees known as coxa valga, and angles <120 degrees knows as coxa vara). The effect of this femoral offset or overhanging head and neck is to lateralize the hip abductors, which increases their potential torque and reduces the overall force necessary to balance the pelvis. The base of the femoral neck broadens into the lesser and greater trochanters, which serve as strong sites for hip abductor and adductor motor attachments.
Capsule, Ligaments, and Labrum
The articular capsule of the hip joint is a strong, dense, fibrous capsule. Proximally, it is attached to the edge of the acetabulum, just peripheral to the labrum. It is attached distally to the neck of the femur. Anteriorly, it inserts along the intertrochanteric line and posteriorly, just proximal to the intertrochanteric crest. The capsule blends with a number of intrinsic ligaments, which serve to provide static stability to the hip joint on extremes of motion as well as maintain joint fluid in an enclosed space for lubrication.
The capsular ligaments include the iliofemoral ligament, pubofemoral ligament, and ischiofemoral ligament (Figs 25-6 and 25-7). These capsular ligaments thicken the capsule and make it challenging at times to penetrate when placing arthroscopic portals.
The iliofemoral ligament, also known as the Y ligament of Bigelow, originates from the anterior inferior iliac spine and the acetabular rim distally to the intertrochanteric line of the femur. This ligament is Y-shaped and becomes taut in extension of the hip. This ligament serves an important role in hip biomechanics to prevent hyperextension and maintain an erect posture in the standing position. The pubofemoral ligament originates from the pubic portion of the acetabular rim and blends with the iliofemoral ligament. It serves to provide strength to the inferior and anterior aspect of the hip joint. It becomes tight into abduction and extension. The ischiofemoral ligament originates from the ischial acetabular rim and inserts to the superior lateral femoral neck along the medial aspect of the greater trochanter. It also becomes taut into hip extension, again, preventing hyperextension of the hip joint.
 Fig 25-6. Anterior view of the capsuligament complex of the hip demonstrates the Y ligament of Bigelow, the iliofemoral ligament, and the pubofemoral ligament. (Courtesy of Anatomic Chart Company.) |
The ligamentum teres is an intra-articular ligament originating from the acetabular notch (with extension to the transverse acetabular ligament) inserting into the fovea of the femoral head. Within this ligament, there exists a foveal artery originating from the obturator artery. The artery is viable in children but may not play a significant role of arterial supply to the femoral head in adults. This ligament is contained within a sleeve of synovial membrane but rupture with hip dislocation usually leads to violation of both. A torn ligamentum teres may catch within the articular surface of the joint and be an intra-articular source of a snapping hip.
The labrum is composed of fibro-elastic cartilage with interlacing network of collagen fibers, proteoglycans, glycoproteins, and cellular elements. Scanning electron microscopy revealed three distinct layers in the acetabular labrum: (a) the articular surface covered by a meshwork of thin fibrils; (b) beneath the superficial layer a layer of lamella-like collagen fibrils; and (c) the deepest layer of collagen fibrils oriented in a circular manner to absorb hoop stresses. The vascular supply reaches only the peripheral third of the labrum (4,5).
 Fig 25-7. Posterior view of the capsuloligamentous complex of the hip demonstrates the ischiofemoral ligament. (Courtesy of Anatomic Chart Company.) |
The role of the labrum is still not completely understood, but there is a number of proposed theories. An important role is likely in providing increased joint stability. By increasing the depth of the socket, the labrum assists in structurally maintaining the humeral head in the socket. In addition, the labrum provides a seal to the joint, thereby providing stability utilizing ambient and intra-articular pressures to keep the joint reduced. Hydrostatic fluid pressure with the intra-articular space is greater with an intact labrum than without which may enhance joint lubrication (6).
The labrum probably plays a significant role in load transmission across the hip (Fig 25-8). A number of studies have revealed that the presence of labral tears is directly associated with degenerative changes in adjacent articular cartilage (7,8). Nonetheless, the direct relationship with labral injury and increased cartilage degeneration may not be so clear because another study revealed increased degeneration only when both the labrum and the transverse acetabular ligaments were resected (5,9). Tear location should be described as anterior, superior, or posterior and, if possible, peripheral or central. Tears may also be described as longitudinal, radial, or flap tears (Fig 25-9). The majority of the tears involve the anterior labrum. This is true for sports-related injures, which are commonly torsional, occult tears with no specific mechanism, and in patients with degenerative joint disease or hip dysplasia. Isolated posterior labral tears typically occur with posterior hip dislocations or occasionally in dysplastic hips. Complex and severe injuries may involve the anterior, superior, and posterior labrum; therefore, thorough examination is always necessary (10,11). Degenerative tears may be associated with intra-articular degeneration and appear as friable tissue with complex tear patterns. Acute tears, radial flap, and longitudinal peripheral tears, may have sharper borders. Longitudinal peripheral tears have the potential for repair if identified early. Labral pathology associated with dysplastic hips may present with hypertrophy or degenerative tearing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








