Abstract
Introduction
A previous study (carried out in 2003–2004) had included 34 patients with traumatic brain injury in order to study the feasibility and usefulness of music therapy in patients with this type of injury.
Objective
To evaluate the effect of music therapy on mood, anxiety and depression in institutionalised patients with traumatic brain injury.
Study methodology
A prospective, observational study.
Materials and methods
Thirteen patients with traumatic brain injury were included in the present study and took part in individual, weekly, 1-hour music therapy sessions over a period of 20 weeks. Each session was divided into two 30-minute periods – one devoted to listening to music (receptive music therapy) and the other to playing an instrument (active music therapy). The assessment criteria (measured at weeks 1, 5, 10, 15 and 20) were mood (on the face scale) and anxiety–depression (on the Hospital Anxiety and Depression [HAD] Scale). Mood was assessed immediately before and after the first music therapy session and every fifth session.
Results
Music therapy enabled a significant improvement in mood, from the first session onwards. This short-term effect was confirmed by the immediate changes in the scores after music therapy sessions (from 4.6 ± 3.2 to 2.6 ± 2; p < 0.01). Music therapy also led to a significant reduction in anxiety–depression ( p < 0.05) from week 10 onwards and up until the end of the study (week 20).
Conclusion
These results confirm the usefulness of music therapy in the treatment of anxiety–depression and mood in patients with traumatic brain injury. Music therapy could usefully form an integral part of the management programme for these patients.
Résumé
Objectif
Évaluer l’intérêt de la musicothérapie sur l’humeur et l’anxiété–dépression dans la prise en charge des patients cérébrolésés traumatiques (Glasgow Coma Scale de 3 et 4) institutionnalisés en foyer d’accueil médicalisé.
Matériels et méthodes
Étude prospective observationnelle sur 13 patients cérébrolésés. Les patients étaient suivis pour une période de 20 semaines et participaient une fois par semaine à une séance individuelle de musicothérapie d’une heure. La séance était partagée en deux périodes de 30 minutes à savoir une partie consacrée à l’écoute musicale (musicothérapie réceptive : méthode validée en U) et une partie à la pratique instrumentale (musicothérapie active). Les critères de jugement, mesurés à S1, S5, S10, S15 et S20, étaient l’humeur (échelle à visages) et l’anxiété–dépression (Hospital Anxiety and Depression [HAD] Scale). L’humeur était évaluée juste avant et après les séances de musicothérapie.
Résultats
La musicothérapie s’est accompagnée d’une amélioration significative de l’état d’humeur dès la première séance. L’effet à court terme a été confirmé par les résultats apportés juste après les séances de musicothérapie (4,6 [± 3,2] à 2,6 [± 2] ; p < 0,01). La musicothérapie permettait aussi de réduire de façon significative l’anxiété–dépression ( p < 0,05) à partir de S10 jusqu’à S20.
Conclusion
Ces résultats confirment l’intérêt de la musicothérapie dans la prise en charge de l’anxiété–dépression et sur l’état de l’humeur des patients traumatisés crâniens. La musicothérapie peut être une démarche s’intégrant parfaitement dans la prise en charge de ces patients. Une étude contrôlée, randomisée est possible et doit être promue pour confirmer l’impact de la musicothérapie sur l’humeur et, éventuellement sur la consommation d’antidépresseurs chez des patients traités.
1
English version
1.1
Introduction
Traumatic brain injury is characterised by cognitive and behavioural disorders . Motor after-effects are also common and often have an impact on functional independence . Although neuropsychological and behavioural disorders affect two thirds of patients with traumatic brain injury, our lack of knowledge of these conditions can hamper the rehabilitation and, social and professional reintegration of these individuals for many years after their accident . Post-traumatic behavioural disorders (including hyperactivity, agitation, mood swings, irritability, excitation, lack of inhibition, hostility and distrust) constitute major problems with respect to the management, rehabilitation, and social and family reintegration of these patients . Indeed, it appears that some of these disorders may become chronic or even worsen over time .
A number of recent clinical studies have demonstrated the positive impact of music therapy on the rehabilitation of patients with traumatic brain injury . Developments in functional imaging techniques have made it possible to study the action of music on cerebral functions and verify its impact . Indeed, studies in patients with brain lesions have shown that many different brain areas are involved in processing musical information . Music requires constant collaboration between the two hemispheres and thus encourages more harmonious cerebral activity . Studies have also shown that music therapy stimulates cognitive functions, acts on anxiety, depressive phases and aggressiveness and thus significantly improves mood, communication and independence in brain-injured patients .
A feasibility study (carried out during 2003–2004) on 34 patients with traumatic brain injury allowed us to demonstrate the usefulness of music therapy and to observe the significant results achieved using this technique. Sessions based on playing instruments (active therapy) were able to stimulate both cognitive functions (concentration, memory, etc.) and psychomotor functions (coordination, lateralisation of movements, etc.). Furthermore, receptive therapy (based on listening to music) enabled an improvement in anxiety and/or depression and encouraged the verbal expression of the patients’ suffering. In addition, music therapy could easily be included in a multidisciplinary management programme for patients with traumatic brain injury .
The aim of the present study was to assess the usefulness of music therapy with respect to mood and anxiety–depression in a population of patients with traumatic brain injury institutionalised in a medical rehabilitation centre. The study sought to:
- •
establish whether the method used in the USA by Nayak et al. could be applied in the context of a French rehabilitation center;
- •
determine any side effects of the method and;
- •
test the validity of the assessment criteria employed.
1.2
Materials and methods
1.2.1
Consent
A patient information sheet and an informed consent form was given to each patient prior to his/her inclusion, with the agreement of the social and medical staff responsible for patients in the rehabilitation center. Anxiety, depression and mood changes are recognised indications for music therapy and thus the care techniques employed were standard and not innovative. For this type of observational study, approval from an independent ethics committee was not required.
1.2.2
Study population
All the study subjects had experienced traumatic brain injury and were institutionalised in the “Les-Fontaines-d’Ô” rehabilitation center (Adages) in Montpellier, France, over the period from September 2005 to June 2006. The subjects were following a multidisciplinary patient management programme which combined physical exercise, physiotherapy, occupational therapy, relaxation, sophrology, sensory stimulation and cognitive training and which lasted an average of 6 hours a day.
1.2.3
Eligibility criteria
The criteria for inclusion were as follows: a diagnosis of serious, traumatic brain injury with a Glasgow Coma Scale score of 3 or 4; age between 25 and 50; the ability to speak and read French easily; the absence of treatment with psychotropic, anxiolytic or antidepressant drugs.
Patients excluded from the study were those presenting with mild to moderate traumatic brain injury, hearing deficiency or a history of audiogenic epilepsy. Patients were included in the study by a physician at the centre, following verification of compliance with the study eligibility criteria and the provision of informed consent.
1.2.4
Methods
Patients meeting all the inclusion criteria and none of the exclusion criteria participated in individual music therapy sessions, which took place once a week for 5 months (i.e., for 20 weeks).
Two music therapy techniques were employed.
1.2.4.1
Receptive music therapy
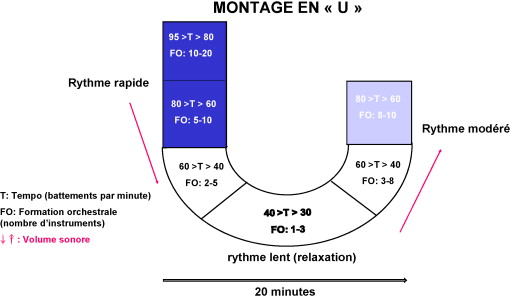
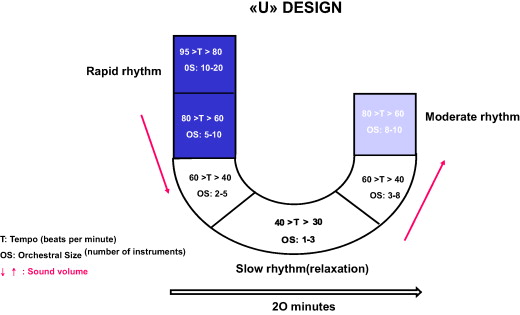
The new, validated, “U-based” music therapy technique was applied ( Fig. 1 ): it is mainly used in the context of acute and chronic pain and its effects; construction and frequency of application are comparable to a sophrology-type relaxation session. The music (chosen according to the patient’s personal taste) was played into headphones whilst the patient lay supine in an otherwise silent room. These music sequences generally lasted for 20 to 30 minutes and contained several pieces of music; each was a just few minutes long but the pieces were merged and linked, so as to gradually encourage the patient to relax. This effect was achieved firstly by slowing the musical rhythm and reducing the number of instruments in the orchestra, the frequencies and the volume (i.e., the descending phase of the “U”). The patient then moved through the maximum relaxation phase (i.e., the lower bend of the “U”), which was lastly followed by an increasingly dynamic phase (i.e., the ascending phase of the “U”) ( Fig. 2 ).
1.2.4.2
Active music therapy
This consisted in playing a musical instrument with the patient. Emphasis was placed on interventional techniques such as singing, instrumental or gestural improvisation, song-writing and the execution of rhythmic movements to musical accompaniment. It encouraged stimulation of cognitive functions through memorisation, concentration and attentiveness. Preference was given to the non-verbal register involving movement, thus encouraging both communication and expression in particular .
1.2.5
Study endpoints
The study’s primary endpoint was a change in mood. Such changes were measured using a patient-scored face scale , which involved the patients being shown five faces with expressions ranging from laughter to extreme sadness. This test is widely employed in a pediatric setting. The score ranges from 0 (a very good mood) to 10 (a very bad mood). These assessments were made immediately before and after sessions S1, S5, S10, S15 and S20. The aim was to determine the immediate efficacy of each music therapy session using this scale, which was presented by the therapist before and after each of the sessions in question.
Anxiety and depression components were assessed using the Hospital Anxiety and Depression (HAD) Scale which comprises 14 questions, seven for anxiety and seven for depression. Answers are scored from 0 to 3. The final scale thus ranges from 0 (mild anxiety–depression) to 21 (severe anxiety–depression) for each of the anxiety and depression components . Assessments were made during S1, S5, S10, S15, S20 and made it possible to monitor the change in these components over the duration of the study.
1.2.6
Statistical analysis
An overall description was performed for each of the variables considered. For qualitative variables, the frequencies of each modality were determined. For quantitative variables, mean, standard deviation, median, minima and maxima were calculated.
Demographic data were analysed at baseline (D0). Mean values were compared using Student’s t -test. Qualitative variables were compared using the Chi 2 test and a non-parametric Mann–Whitney test for non-Gaussian distributions. A p value below 0.05 was deemed significant.
Statistical analyses were performed in collaboration with the Medical Information Department at Montpellier University Hospital, using SAS software (SAS Institute Inc., Cary, NC, USA), version 6.12.
1.3
Results
1.3.1
Description of the study population
In all, 13 out of 47 screened patients met the criteria for inclusion. None of these 13 subjects subsequently withdrew from the study. The group comprised three men and 10 women. Two were of African origin and 11 were Caucasian. Eleven patients were single and two were divorced. The mean age was 31 years and the mean time since injury was 8 years (i.e., the mean age of patients at the time of brain injury was 23 years) ( Tables 1 and 2 ).
| Description of patients | |||
|---|---|---|---|
| Variable | Modality | Population | % |
| Gender | Male | 3 | 77 |
| Female | 10 | 23 | |
| Total | 13 | 100 | |
| Origin | African | 2 | 15 |
| French | 11 | 85 | |
| Total | 13 | 100 | |
| Educational level | University | 1 | 8 |
| Secondary qualification | 3 | 23 | |
| Secondary – no qualification | 9 | 69 | |
| Total | 13 | 100 | |
| Family status | Single | 11 | 85 |
| Divorced | 2 | 15 | |
| Total | 33 | 100 | |
| Variable | n | Mean | Standard deviation | Maximum | Median | Minimum |
|---|---|---|---|---|---|---|
| Age (years) | 13 | 31.1 | 9.3 | 50 | 31 | 25 |
| Age at accident (years) | 13 | 22.8 | 10.5 | 47 | 22 | 5 |
| Time since accident (years) | 13 | 8 | 7.5 | 25 | 6 | 1 |
1.3.2
Effects of music therapy sessions on mood: before–after
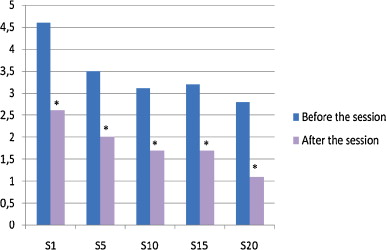
Table 3 shows the mean face scale scores for mood immediately before and after each of the S1, S5, S10, S15 and S20 music therapy sessions. Significant improvements ( p < 0.05) could be observed after each music therapy session. As early as the first session, this improvement was around 2 (± 2) points (–43%), from a mean presession level of 4.6 (± 3.2). It is noteworthy that between S1 and S5, the presession score improved from 4.6 (± 3.2) to 3.5 (± 3) ( p < 0.05). Significant changes appeared from one session to another ( p < 0.05). The mood score generally rose (i.e., worsened) slightly between the end of one session and the beginning of the next session ( Table 3 and Fig. 2 ). The score differences were also significant for the periods before S1–S10, S1–S15 and S1–S20 ( p < 0.05).
| Value | Before music therapy | After music therapy | Difference (S.D.) | % | p | ||
|---|---|---|---|---|---|---|---|
| n | Mean (S.D.) | n | Mean (S.D.) | ||||
| S1 | 13 | 4.6 (± 3.2) | 13 | 2.6 (± 2.0) | −2.0 (± 2) | −43 | 0.008 * |
| S5 | 13 | 3.5 (± 3) | 13 | 2.0 (± 1.8) | −1.5 (± 2) | −43 | 0.03 * |
| S10 | 13 | 3.1 (± 2.7) | 13 | 1.7 (± 2.1) | −1.4 (± 2) | −45 | 0.06 * |
| S15 | 13 | 3.2 (± 2.7) | 13 | 1.7 (± 2.1) | −1.5 (± 1.6) | −47 | 0.01 * |
| S20 | 13 | 2.8 (± 2) | 13 | 1.1 (± 1.0) | −1.7 (± 1.6) | −61 | 0.008 * |
* According to Student’s paired t -test; * p < 0.05 = significant.
1.3.3
Effects of music therapy on anxiety–depression (HAD score)
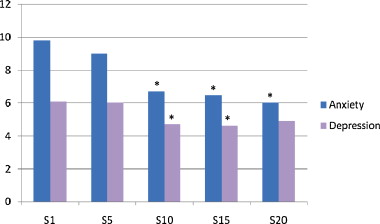
The patients’ mean level of anxiety at the start of the study was deemed to be moderate (9.8 ± 5 out of 21). For the S1–S5 period, the difference was not significant (−0.8 ± 3.1). However, significant reductions ( p = 0.05) were seen for periods S1–S10 (−3.1 ± 2.5), S1–S15 (−3.3 ± 5.1) and S1–S20 (−3.8 ± 5.4). It is noteworthy that there was a relative improvement of 39% in the level of anxiety between S1 and S20 ( Table 4 and Fig. 1 ).
| n | Mean (S.D.) | Min/max | % | p | ||
|---|---|---|---|---|---|---|
| Anxiety | ||||||
| Values | S1 | 13 | 9.8 (± 5) | 1/17 | 100 | N.S. |
| S5 | 13 | 9.0 (± 3.4) | 4/18 | 92 | N.S. | |
| S10 | 13 | 6.7 (± 3.2) | 1/13 | 68 | < 0.05 * | |
| S15 | 13 | 6.5 (± 2) | 4/10 | 66 | < 0.05 * | |
| S20 | 13 | 6.0 (± 3.4) | 2/14 | 61 | < 0.05 * | |
| Differences | S1–S5 | 13 | −0.8 (± 3.1) | −3/7 | −8 | N.S. |
| S1–S10 | 13 | −3.1 (± 2.5) | −5/11 | −32 | < 0.05 * | |
| S1–S15 | 13 | −3.3 (± 5.1) | −3/12 | −34 | < 0.05 * | |
| S1–S20 | 13 | −3.8 (± 5.4) | −2/14 | −39 | < 0.05 * | |
| Depression | ||||||
|---|---|---|---|---|---|---|
| Values | S1 | 13 | 6.1 (± 2.9) | 0/13 | 100 | N.S. |
| S5 | 13 | 6.0 (± 3.2) | 3/14 | 98 | N.S. | |
| S10 | 13 | 4.7 (± 3.2) | 1/10 | 77 | < 0.05 * | |
| S15 | 13 | 4.6 (± 2.9) | 0/10 | 75 | < 0.05 * | |
| S20 | 13 | 4.9 (± 3.4) | 1/12 | 80 | N.S. | |
| Differences | S1–S5 | 13 | −0.1 (± 3) | −7/3 | −2 | N.S. |
| S1–S10 | 13 | −1.3 (± 1.8) | −2/5 | −23 | < 0.05 * | |
| S1–S15 | 13 | −1.4 (± 3.4) | −2/5 | −25 | < 0.05 * | |
| S1–S20 | 13 | −1.1 (± 2.1) | −2/5 | −20 | N.S. | |
* According to Student’s paired t -test; N.S. = not significant; * p < 0.05 = significant.
The baseline depression score was low (6.1 ± 2.9 out of 21). For this parameter, the difference (−1.3 ± 1.8) between S1 and S10 was significant ( p < 0.05), with a relative improvement of 23%. The differences remained significant for S1 versus S15 (−1.4 ± 3.4), with a relative improvement of 25%. However, the results were no longer significant for S10 versus S20 ( Table 4 and Fig. 3 ).
1.4
Discussion
Significant before-versus-after improvements in the primary endpoint (mood) were observed for each of the five assessed music therapy sessions. Enhancement of the effect was also observed with the increase in the number of sessions, which could suggest a dose-dependent effect ( Table 3 ). This improvement was around 43% following the first weekly session and rose to 61% by the 20th session. Our results confirmed those observed by Nayak et al. in the context of a controlled, randomised study performed in 2000 in an American functional rehabilitation center. The authors demonstrated the value of music therapy for improving mood and behaviour in patients with traumatic brain injury. During Nayak et al.’s study, the mean ( n = 10) primary endpoint score (a patient-scored face scale) fell from 4.6 (± 1.8) to 2.8 (± 1.3), with a relative improvement of 39%. During our study, we achieved an improvement of 2 (± 2) points, with scores falling from 4.6 (± 3.2) after the first session to 2.6 (± 2), i.e., a 43% improvement. Our results were thus comparable with those reported by Nayak et al. and thus confirm the short-term efficacy of a music therapy session with respect to mood. Further studies are necessary to determine how long this effect is sustained after sessions are discontinued – an assessment 1 hour after the end of the session would have been interesting. Nevertheless; we obtained significant differences between the initial assessment (i.e., just before the first session) and the start of the fifth, 10th, 15th and 20th sessions ( p < 0.05).
The results concerning anxiety–depression (HAD) at S10 demonstrated a significant difference for both components ( p < 0.05). The significant effect of music therapy on anxiety was seen to persist until S20. The results concerning the affective component of symptom changes showed that the effect of music therapy was sustained. One week after the discontinuation of sessions, the anxiolytic effect was still present.
In terms of the various mechanisms involved in music–subject interaction, it seems very likely that music can modify the course of disorders through its sensory, cognitive, affective and behavioural effects. Hence, music therapy is mainly active on memory disorders, anxiety–depression and agitation.
The effects of receptive music therapy are usually related to the fact that individualised musical listening markedly relieves painful experiences. The impact of this type of therapy may be due to music-specific neuropsychological effects that act on sensory components (causing contra-stimulation of afferent fibres), cognitive components (often deflecting attention by creating images and banishing memories of pain), affective components (modifying moods associated with states such as depression or anxiety and thus relieving tension and feelings of anguish) and behavioural components (acting on muscle hypotonia and psychomotility) . The effects of music therapy are based on the impact of music on different components in the overall, painful experience and changes in the perception of pathological disorders .
Psychological factors may also contribute to reducing affective symptoms: the music is chosen as a function of the patient’s personal taste and thus in response to individual listening needs. Talking to patients following a session may thus provide an opportunity for some of them to free themselves of their problems and encourage a supportive, listening relationship .
Music therapy has a considerable effect on mood. In the context of our study, the anxiolytic effect of music therapy was probably strong because of its combination with all the other rehabilitation activities. However, our work also clearly demonstrated a clinically relevant short-term effect of music therapy, with the patients acting as their own controls (i.e., pre- and post-session assessments).
This type of technique may require a large number of sessions. Emphasis should also be placed on adapting the style of music (classical, modern, jazz, easy listening, rock, electronic, world music, etc.) to the patient’s receptiveness .
Our aim was to demonstrate the feasibility and short-term efficacy of music therapy in patients with traumatic brain injury acting as their own controls. These initial findings provide a good working basis for a controlled, randomised study for assessing the value of music therapy; the goal would be to add a new therapeutic weapon (devoid of side effects) to the already wide-ranging arsenal available for the rehabilitation of patients with traumatic brain injury. Ultimately, this will enable a comparison with other similar therapeutic interventions, such as speaking or singing.
1.5
Conclusion
The present preliminary study suggests the value of music therapy in patients with traumatic brain injury as part of a multidisciplinary management programme. Music therapy contributes to functional and cognitive rehabilitation by improving mood and the anxiety–depression components in severe patients with traumatic brain injury. The intentional use of the potential and properties of music acts through many interacting mechanisms (be they sensorial, cognitive, affective or behavioural) and thus enables a direct impact over time on all these components in the patient.
2
Version française
2.1
Introduction
Le traumatisme crânien se caractérise par des troubles cognitifs et du comportement . Les séquelles motrices sont aussi fréquentes et ont souvent des conséquences sur l’indépendance fonctionnelle . Ces troubles neuropsychologiques et comportementaux touchent les deux tiers des patients et leur méconnaissance entrave la rééducation et la réinsertion socioprofessionnelle de ces personnes des années après l’accident . Ces nombreux troubles du comportement post-traumatiques incluent l’hyperactivité, l’agitation, la labilité, l’irritabilité, l’excitation, la désinhibition, l’hostilité et la méfiance, et sont source de difficultés majeures dans la prise en charge, la réadaptation et la réinsertion sociale et familiale de ces blessés . Il semble que certains de ces troubles se pérennisent, voire parfois s’amplifient avec le temps .
Quelques études cliniques récentes ont permis de mettre en évidence le rôle favorable de la musicothérapie dans la réadaptation des traumatisés crâniens . L’évolution des techniques d’imagerie fonctionnelle a permis de vérifier et d’étudier l’action de la musique sur les fonctions cérébrales . Les études auprès de personnes atteintes de lésions cérébrales ont permis de montrer la diversité des zones du cerveau impliquées dans le traitement de l’information musicale . La musique demande une collaboration constante entre les deux hémisphères qui favorise une activité cérébrale plus harmonieuse . Les études montrent ainsi que la musicothérapie stimule les fonctions cognitives, agit sur l’anxiété, les phases dépressives, l’agressivité et améliore ainsi de façon significative l’humeur, la communication et l’autonomie des patients cérébrolésés .
Une étude de faisabilité réalisée durant l’année 2003–2004 sur 34 patients cérébrolésés nous avait permis de démontrer la faisabilité et d’observer des résultats significatifs de la musicothérapie chez les traumatisés crâniens. Les séances basées sur la pratique instrumentale, dite active, ont permis de stimuler les fonctions cognitives (concentration, mémoire…) et psychomotrices (coordination, latéralisation des mouvements). La technique réceptive, basé sur l’écoute musicale, a permis une amélioration des troubles de l’anxiété–dépression et a favorisé la verbalisation de la souffrance des patients. De plus, la musicothérapie s’est intégrée facilement dans un programme pluridisciplinaire de prise en charge des traumatisés crâniens .
L’objectif de cette étude est d’évaluer l’intérêt de la musicothérapie sur l’humeur et sur l’anxiété–dépression dans une population de patients cérébrolésés institutionnalisés en foyer d’accueil médicalisé. Elle a cherché à vérifier l’applicabilité de la méthode utilisée aux États-Unis par Nayak et al. , dans le contexte d’un établissement médicosocial français, à rechercher les effets secondaires éventuels et à tester la validité des critères de jugement utilisés.
2.2
Matériels et méthodes
2.2.1
Consentement
Une fiche d’information, ainsi qu’un consentement éclairé de participation à l’étude, ont été remis au patient précédemment à l’inclusion en accord avec l’encadrement social et médical du foyer d’accueil médicalisé en charge des résidants. L’anxiété, la dépression et la modification de l’humeur sont en effet des indications reconnues de la musicothérapie et les techniques de soin utilisées étaient habituelles et non innovantes. Dans ce type d’étude, dites observationnelles, aucune soumission à un Comité de protection des personnes (CPP) n’est requise.
2.2.2
Population étudiée
Les patients, tous atteints de traumatismes crâniens, étaient institutionnalisés dans le foyer d’accueil médicalisé « Les-Fontaines-d’Ô » (Adages) de Montpellier, durant la période allant de septembre 2005 à juin 2006, où il leur était appliqué un programme de prise en charge pluridisciplinaire associant des exercices physiques, de la kinésithérapie, de l’ergothérapie, de la relaxation, de la sophrologie, des stimulations sensorielles et un entraînement cognitif, à raison d’une moyenne de six heures par jour.
2.2.3
Critères d’éligibilité
Les critères d’inclusion étaient un diagnostic de cérébrolésion grave avec un score au Glasgow Coma Scale à 3 ou 4, un âge compris entre 25 et 50 ans, l’aptitude à parler et à lire couramment le français et l’absence de traitement psychotrope et anxiodépressif.
N’étaient pas inclus les patients présentant un traumatisme crânien léger à modéré, un antécédent d’épilepsie audiogène ou une déficience de la fonction auditive. L’inclusion des patients dans l’étude a été réalisée par un médecin de l’institution qui s’assurait de la présence des critères d’éligibilité et de l’obtention du consentement.
2.2.4
Méthodes
Les patients répondant aux critères d’inclusion ont participé à des séances individuelles de musicothérapie. Les séances ont eu lieu une fois par semaine pendant cinq mois (20 semaines).
Deux techniques de musicothérapie ont été utilisées :
2.2.4.1
Musicothérapie réceptive
Nous avons utilisé la nouvelle technique de musicothérapie validée du montage en U ( Fig. 1 ) : essentiellement utilisée dans le cadre de douleurs aiguës et chroniques, son effet, sa construction et sa fréquence d’application sont comparables à une séance de relaxation de type sophrologie. La musique, choisie en fonction des goûts personnels du patient , a été diffusée au casque en position allongée, dans une salle silencieuse. La séquence musicale dure généralement de 20 à 30 minutes. Elle assemble plusieurs morceaux de quelques minutes chacun, fondus et enchaînés dans le but d’induire progressivement le patient à la détente. L’effet agit tout d’abord par une diminution du rythme musical, de la formation orchestrale, des fréquences et du volume (phase descendante du « U »). Ensuite, le patient traverse la phase de détente maximum (partie basse du « U »), qui est enfin suivie par une phase redynamisante (branche ascendante du « U ») ( Fig. 2 ).