Abstract
Return to work is the main long-term objective of rehabilitation programs for patients with chronic low back pain (LBP).
Objectives
Evaluation of work status and number of sick leaves in 87 severely impaired LBP patients 2 years after a functional restoration program.
Patients and methods
Open prospective study. Population: 87 chronic LBP patients. Intervention: multidisciplinary functional restoration program. Ergonomic advice on the workplace was performed for 53 patients. Outcome: work status and number of sick leaves due to LBP.
Results
The characteristics of the 26 patients lost to follow-up did not differ significantly from the rest of the population before the program. In the 61 remaining patients, 48 (78%) were at work at 2 years, 43 full-time and 22 at the same job. Nineteen worked in a different environment. Sick leaves were reduced by 60% compared to the 2 years prior to the program: 128 days (± 200 days) versus 329 days (± 179 days); p < 0.005.
Conclusion
Sick leaves remained significantly reduced and the number of workers who were at work significantly increased at 2 years after an intensive program.
Résumé
Introduction
Le maintien dans l’emploi à long terme est l’objectif principal des programmes de reconditionnement de patients lombalgiques chroniques.
Objectifs
Évaluation de la présence au travail et de la diminution des durées d’arrêt de travail de 87 salariés lombalgiques deux ans après un programme de reconditionnement à l’effort.
Patients et méthodes
Étude prospective ouverte menée sur 87 lombalgiques chroniques, issus de trois départements. Tous ont été inclus dans un programme multidisciplinaire de reconditionnement à l’effort et 53 ont bénéficié d’une action ergonomique en entreprise. L’évaluation porte sur la présence au travail à deux ans et le nombre de jours d’arrêt de travail en rapport avec une lombalgie.
Résultats
Vingt-six patients sont sortis de l’étude pour de multiples raisons. Leurs caractéristiques initiales ne sont pas significativement différentes du reste de la population. Sur les 61 cas analysables, 48 (78 %) sont au travail, dont 43 à plein temps et 22 au même poste. Dix-neuf travaillent sur un autre poste ou ont changé de métier. La durée moyenne des arrêts de travail est diminuée de 60 % par rapport à ce qu’elle était deux ans avant le stage : 128 jours (± 200 jours) contre 329 jours (± 179 jours) ; p < 0,005. Soixante-dix-huit pour cent des lombalgiques sont au travail à deux ans alors qu’ils n’étaient que 28 % avant le stage.
Conclusion
La diminution de la durée d’arrêt de travail comme la présence au travail après un programme de reconditionnement à l’effort reste significative avec un recul de deux ans.
1
English version
1.1
Introduction
Return to work of low back pain (LBP) patients remains a public health issue as recently stated by the federal centre for healthcare expertise, KCE .
Chronic LBP is a common condition: a survey conducted in the area “Pays-de-la-Loire” showed that 58% of workers had suffered from LBP in the past year, and that 7% reported that pain was present every day. A recent report by Leclerc et al. highlights the social consequences of LBP . The main issue is the occurrence of major disability in a limited number of patients and this was already pointed by Spitzer et al. more than 20 years ago .
Several different approaches have been developed during the past two decades. The risk factors for chronicity have been extensively studied and therapeutic strategies have been developed. Psychosocial characteristics, among which the fears and believes concerning movement, have been shown to play a major role. Counselling strategies have been increasingly focused on these elements. LBP programs have been developed, based on the concept of physical and psychosocial deconditionning. They include multidisciplinary interventions with the objective of resuming activities and returning to work. Short-term outcomes such as improvement of physical performance are very significant . Evaluation of such programs includes the cost–effectiveness evaluation and requires long-term follow-up and data on the long-term work status. Such data are quite scarce and most of the available studies are limited to one-year follow-up .
Since 2000, several cohorts of LBP patients have been studied . Results at 1 year of a series of 87 patients showed a 60% decrease of sick leaves and 72% of the patients had returned to work . The objective of the present study is to report the results at 1 years and define the main factors predictive of return to work.
1.2
Patients and methods
This is a prospective open study. The inclusion criteria were:
- •
age between 18 and 53;
- •
presence of chronic LBP or lumbo-radiculalgy according to the criteria of the French health evaluation agency ;
- •
presently employed with a permanent contract;
- •
on sick leave or having been on sick leave for over 6 months in the past 2 years.
Exclusion criteria were secondary LBP, osteoarthritis or neurological disease precluding physical exercise, cardiovascular disease (diagnosed after cycloergometer stress tests) and psychiatric disorders incompatible with the participation in a group program.
1.3
Intervention
The intervention includes participation in a functional restoration program (FRP) and ergonomic intervention on the workplace. The FRP program was standardised and performed in two rehabilitation centres. It has been described in detail in the study reporting results at 1 year . This program includes physiotherapy interventions, occupational therapy interventions and psychological counselling. The medical supervisor is a physiatrist. Patients participate as in- or outpatients 6 hours per day, 5 days a week during 5 weeks.
The ergonomic intervention is provided on the workplace by a regional agency devoted to the improvement of work conditions (ARACT), according to the standards defined for “short interventions” by the national agency (ANACT). This intervention is only possible after agreement of the company and was performed for 53 patients. It consists in:
- •
a diagnosis of the work conditions, conducted with the different actors;
- •
the definition of an action program;
- •
feedback for the company.
This intervention is tailored to the specific context of the company and cannot be completely standardised.
1.4
Evaluation
The evaluation is similar to that conducted at 1 year . Finger to floor distance was used to evaluate flexibility. The strength of the trunk flexors and extensors was evaluated by the Ito et al. and Sorensen tests. Lifting ability was evaluated by the “Progressive Isoinertial Lifting Evaluation” (PILE) test . Quality of Life was evaluated by the self-administered Dallas questionnaire . Disability was evaluated by the Quebec self-administered questionnaire . The Hospital Anxiety and Depression scale (HAD) was used to evaluate psychological consequences of LBP.
Sick leaves due to LBP were self-reported by the patients.
1.5
Statistical analysis
Mean value and standard deviation were calculated for quantitative variables. The chi 2 test was used to compare qualitative variables and the T test for quantitative variables. Non-parametric tests for paired variables (chi 2 and Wilcoxon test) were used for to compare the pre- and post-treatment values of qualitative variables. Pre- and post-treatment c quantitative variables were compared by the student t test.
Analysis of the predictive factors of return to work was performed by univariate analysis for the 61 patients in whom the work status at 2 years follow-up was available. We tested the following variables: gender, age, work constraints, previous spinal surgery, being on sick leave at the beginning of the program, having been on sick leave for over 1 year during the past 2 years, LBP due to industrial accident, Dallas score, HAD score, VAS pain score, physical criteria (FFT, Ito and Sorensen scores), self-assessment of improved physical condition at the end of the program, self-assessment of ability to return to work; self-assessment of ability to resume leisure and sports activities. Multivariate analysis was then performed using logistic regression modelling .
Quantitative variables were dichotomised as above or below the median value in order to obtain balanced classes. The following variables: gender, sick leave, implementation of the ergonomic intervention were forced into the logistic regression model. All variables which were related to the work status in the univariate anaysis with a correlation above 20% were included in the multivariate analysis. Statistical significance was set at 5%.
Analysis were performed on the SPSS software for Windows version 13.0.
1.6
Results
At 1 year, 83 patients completed the evaluation; one had not completed the program; two refused to come back for evaluation and one was lost to follow-up ( Fig. 1 ).
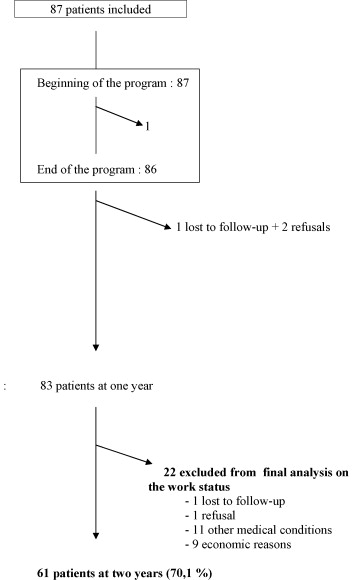
At 2 years, 81 patients (94%) completed the evaluation (one patient refused and one was lost to follow-up).
Twenty were excluded from further analysis for the following reasons:
- •
11 had stopped working for medical reasons unrelated to LBP;
- •
four had undergone surgery (one spinal cord injury, one intestinal occlusion, two knee sprains);
- •
four were hospitalized for psychiatric reasons;
- •
three were off work due to other medical conditions;
- •
nine had stopped working for economic reasons :
- ∘
one female patient stopped work after her husband had a promotion,
- ∘
three patients were fired for economic reasons,
- ∘
five patients followed occupational training programs).
- ∘
The analysis of the factors which were predictive of the work status was conducted in the 61 remaining patients (70%).
There was no significant difference in gender, age, duration of sick leave before treatment, nor in any of the outcome measures between the 21 patients excluded and the 61 patients included in the final analysis.
Forty-four patients over 61 were males; the mean age was 40.8 years. Eighty-four percent were employed in economic sectors characterized by heavy work constraints. The mean duration of sick leaves in the 2 years prior to the program was 329 ± 179 days. Seventy-two percent were on sick leave when included in the program.
Ergonomic intervention was conducted in 41/61 (67%).
At 2 years, 48 (79%) completed all tests (physical items, self-questionnaires, data on work status). The 13 others completed a telephone interview and gave information concerning their work status. Seven of them also completed the self-assessment of physical condition, of the ability to work and of the ability to resume sports activities.
Tables 1 and 2 summarize the physical data.
| Beginning of the program T1 | End of the program T5 | 1 year T12 | 2 years T24 | |||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (S.D.) | n | Mean (S.D.) | n | Mean (S.D.) | n | Mean (S.D.) | |
| VAS | 61 | 4.85 (2.0) | 61 | 3.35 (2.4) | 56 | 3.46 (2.7) | 48 | 3.83 (2.6) |
| Quebec | 61 | 31.62 (15.3) | 61 | 18.82 (15.3) | 57 | 22.14 (18.8) | 48 | 23.90 (15.3) |
| Dallas | 61 | 167.62 (67) | 61 | 88.82 (69) | 57 | 101.88 (90.3) | 48 | 113.47 (80.3) |
| ADL | 61 | 49.41 (15.8) | 61 | 29.23 (20.3) | 57 | 34.86 (24.7) | 48 | 38.75 (22.4) |
| W/L | 61 | 56.08 (21.4) | 61 | 29.43 (20.7) | 57 | 31.05 (26.5) | 48 | 34.69 (23.3) |
| A/D | 61 | 36.5 (22.0) | 61 | 17.58 (18.3) | 57 | 19.21 (23) | 48 | 24.17 (21.5) |
| Soc. | 61 | 27.60 (20.9) | 61 | 13.08 (18.3) | 57 | 16.75 (22.9) | 48 | 18.23 (20.5) |
| HAD | 61 | 16.02 (7.2) | 61 | 10.64 (7.4) | 57 | 12.26 (8.0) | 48 | 12.21 (6.6) |
| HAD anx | 61 | 9.79 (4.1) | 61 | 7.31 (4.5) | 57 | 7.77 (4.7) | 48 | 7.72 (4.3) |
| HAD dep | 61 | 6.59 (3.7) | 61 | 3.66 (3.4) | 57 | 4.49 (3.9) | 48 | 4.47 (3.2) |
| Beginning of the program T1 | End of the program T5 | 1 year T12 | 2 years T24 | |||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (S.D.) | n | Mean (S.D.) | n | Mean (S.D.) | n | Mean (S.D.) | |
| FFT (cm) | 61 | 19.51 (11.0) | 61 | 0.71 (13.3) | 56 | 5.43 (13.5) | 47 | 7.53 (13.6) |
| EXT (sec) | 61 | 71.32 (53.5) | 61 | 185 (79.4) | 54 | 134.66 (75.9) | 47 | 128.06 (73) |
| FLEX (sec) | 61 | 73 (55.8) | 61 | 163.34 (73.6) | 54 | 125.44 (77.1) | 47 | 99.32 (70.4) |
| Squats(kW) | 61 | 287.48 (137.5) | 61 | 462.47 (170.0) | 55 | 411.86 (175.0) | 45 | 413.91 (186) |
| PILE (body weight %) | 61 | 26.77 (11.9) | 59 | 37.57 (12.1) | 53 | 37.83 (12.3) | 40 | 38.11 (13.6) |
| Cyclo (kJ) | 61 | 71.46 (35.3) | 59 | 110.23 (52.1) | 44 | 86.53 (36.3) | ||
All outcome measures remain significantly better at 2 years follow-up than before treatment ( p < 0.01) ( Table 1 ).
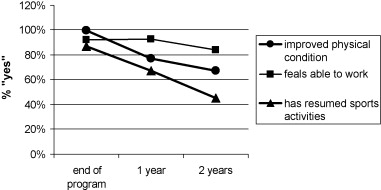
Fifty-six over 61 (92%) “feel able to work” at the end of the program; 53/57 (93%) at 1 year and 46/55 (84%) at 2 years.
Sixty-one over 61 (100%) « feel their physical condition is improved » at the end of the program, 44/57 (77%) at 1 year and 37/55 (67%) at 2 years.
Fifty-three over 61 (87%) “feel able to resume sports activities” at the end of the program, 38/57 (67%) at 1 year and 25/55 (45%) at 2 years.
Less than half of the patients still had a physical activity 2 years after the program. Despite this fact, two thirds felt that their physical condition was better and three out of four felt able to work. Fig. 2 shows the decrease of the items “improved physical condition” and “physical activity” at 1 year whilst 80% still “feel able to work” at 2 years.
1.6.1
Results of the physical tests
All outcome measures remain significantly better at 2 years compared to pre-treatment values ( p < 10 −3 ). The decrease between the values at 1 and 2 years is not significative in contrast, which what had been found between the end of the program and 6 months ( Table 2 ).
1.6.2
Work status at 2 years
Seventeen over 61 (28%) are at work at the beginning of the program, 52/61 (85%) at 1 year and 48/61 (78%) at 2 years. Among the 13 patients off work, four are on disability pension, two are on sick leave after lumbar surgery, one has lost his job because of his disability and six are on sick leave for LBP ( Table 3 ).
| Work status | End of the program T5 | 1 year T12 | 2 years T24 |
|---|---|---|---|
| Full-time | 33 | 47 | 43 |
| Half-time | 15 | 2 | 2 |
| Part-time | 2 | 3 | 3 |
| Same job | 41 | 27 | 22 |
| Different job | 5 | 13 | 19 |
| Adapted job | 4 | 12 | 7 |
Among the patients who are at work, five patients have gone back to a different job immediately after the program and 12 others have changed their job in the two following years. In all cases the new job is physically less demanding. Adaptations in the work are three times more frequent at 1 year than at the end of the program. Fifteen patients work half time at the end of the program and this remains stable at 2 years.
1.6.3
Evolution of sick leaves
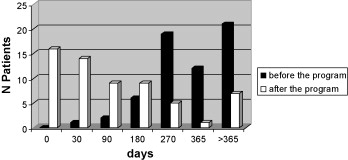
The mean duration of sick leaves decreases by 60% in the 2 years following the program, compared to before the program (128 ± 200 days versus 329 days ± 179 days).
Fourteen patients (23%) have been on sick leave at least 6 months in the two following years. The number of sick leaves is not significantly different during the second post-program year, compared to the first ( Fig. 3 ) ( Tables 4 and 5 ).
| Variables | At work at one year | p | At work at two years | p | ||
|---|---|---|---|---|---|---|
| ( n = 62) | % | n = 48 | % | |||
| “feels able to work” T5 | ||||||
| Yes | 60 | 81.1 | < 0.001 | 46 | 82.1 | < 0.06 |
| No | 2 | 22.2 | 2 | 40.0 | ||
| Ergonomic intervention | ||||||
| Yes | 45 | 86.5 | < 0.002 | 33 | 80.5 | < 0.6 |
| No | 17 | 54.8 | 15 | 75.0 | ||
| Dallas T1 > median value | ||||||
| Yes | 26 | 60.4 | < 0.002 | 24 | 77.4 | < 0.8 |
| No | 36 | 90.0 | 24 | 80.0 | ||
| Anxiety/dépression Dallas T5 > median value | ||||||
| Yes | 27 | 64.3 | < 0.003 | 28 | 73.7 | < 0.3 |
| No | 35 | 85.4 | 19 | 86.4 | ||
| Anxiety/ Depression Dallas T1 > median value | ||||||
| Yes | 26 | 61.9 | < 0.007 | 22 | 68.8 | < 0.07 |
| No | 35 | 87.5 | 25 | 89.3 | ||
| ADL Dallas T1 > median value | ||||||
| Yes | 28 | 63.4 | < 0.013 | 24 | 77.4 | < 0.8 |
| No | 34 | 87.2 | 24 | 80.0 | ||
| Industrial accident | ||||||
| Yes | 23 | 92.0 | < 0.014 | 14 | 77.8 | < 0.9 |
| No | 39 | 67.2 | 34 | 79.7 | ||
| Dallas T5 > median value | ||||||
| Yes | 27 | 64.2 | < 0.024 | (25) | 78.1 | < 0.9 |
| No | 35 | 85.4 | (23) | 79.3 | ||
| Sick leave before treatment ≥ 6 months/1 year | ||||||
| Yes | 19 | 65.5 | < 0.037 | 17 | 81.0 | < 0.5 |
| No | 42 | 85.7 | 31 | 77.5 | ||
| Work/Leisure Dallas T5 > median value | ||||||
| Yes | 29 | 84.6 | < 0.043 | 26 | 76.5 | < 0.6 |
| No | 33 | 65.9 | 22 | 81.5 | ||
| “has resumed sports activities” T5 | ||||||
| Yes | 29 | 84.6 | < 0.043 | 44 | 83.0 | < 0.06 |
| No | 33 | 65.9 | 4 | 50.0 | ||
| HAD depression T1 > median value | ||||||
| Yes | 24 | 70.6 | < 0.07 | 24 | 72.7 | < 0.07 |
| No | 27 | 90.0 | 23 | 92.0 | ||
| PILE %body weight T1 > median value | ||||||
| Yes | 33 | 82.5 | < 0.09 | 28 | 90.3 | < 0.03 |
| No | 29 | 67.4 | 20 | 66.7 | ||
| Work/leisure Dallas T1 > median value | ||||||
| Yes | 32 | 69.6 | < 0.19 | 24 | 75.0 | < 0.5 |
| No | 29 | 80.5 | 23 | 82.1 | ||
| HAD depression T5 > median value | ||||||
| Yes | 25 | 73.5 | < 0.4 | 24 | 72.7 | < 0.2 |
| No | 28 | 84.8 | 24 | 85.7 | ||
| Variables | OR | IC 95% | p |
|---|---|---|---|
| PILE %bw T1 ≥ 50% | 8.2 | 1.5 45.3 | 0.015 |
| HADd T1 ≥ 50% | 0.2 | 0.0 1 | 0.052 |
We analyzed the factors associated with the work status at 2 years and compared them to what had been found at 1 year. This analysis was performed in the 61 patients in which all data were available. Forty-eight of them were at work. The factors were compared to those identified at 1 year (83 patients, 62 of them were at work).
PILE above the median value at the beginning of the program (PILE T1) is the only factor significantly ( p < 0.03) correlated with the work status at 1 years when univariate analysis is performed. Multivariate analysis reveals a significant positive correlation of PILE T1 and a significant negative correlation of the depression subscore of the HAD scale.
1.7
Discussion
This study shows that over 78% of the patients included in the program remain at work at 1 years. The proportion was of 72% at 1 year. This is in agreement with the results of the meta-analyses performed by Hayden et al. , by Kool et al. , and with the studies by Friedrich et al. and Verfaille et al. . In agreement with these previous data, our results show the efficiency of such programs, on the medium- and long-term. Despite overall satisfactory results, 13% of the patients remain on sick leave for LBP or lumbar surgery. When patients on disability pension are included in the count, the proportion of patients off work for over 6 months reaches 23%. Proctor et al. also report that a small proportion of patients remain in unsatisfactory situations despite selection criteria at the entry of the program.
The main methodological difficulty is the analysis of the status of patients who do not work but in which the reason for the cessation of activity is not LBP. We chose to exclude them from the final analysis . We also chose to exclude the five patients who where re-training because the delay and duration of this retraining was very variable. The sub-group of patients excluded from the final analysis was comparable to the general population for all criteria. This procedure reduces the power of the study and possibly over-estimates the decrease in the number of sick leaves.
The only factor correlated with the number of sick leaves is the performance on the lifting task before the program. This has not, to our knowledge, been previously reported and deserves confirmation. Factors which have been previously reported to be correlated such as: “feels able to work”, “has resumed physical activities”, or Dallas or HAD scores above the median value do not, in our study, reach significance. The increase in the physical or psychological criteria during the program does not appear to be correlated with the work status at 2 years either. Ergonomic intervention is not significantly correlated to the work stats at 2 years and we found no clear relation between ergonomic intervention and effective changes in the work environment. Although ergonomic intervention has been described as one of the tools to promote return to work, this does not appear in this study . This may be in part due to the difficulties in standardising this intervention. The possibility of such an intervention heavily depends on work organisation characteristics which probably in themselves influence return to work and this is a major methodological issue.
After decreasing in the 6 months following the program, Physical criteria remain stable and remain better at 2 years than before the program. This is achieved despite the fact that more than half of the patients do not perform physical activities. The absence of correlation between pursued physical activity and the presence at work has already been described by other authors .
The determination of risk factors for persisting LBP and persisting work disability is extremely difficult even when meta-analyses are performed . This discrepancy is in part due to the role of other factors. Kool et al. stress the importance of coping strategies developed during such programs. Recently, Mc Geary et al. highlight the role of pain intensity and reports that high pain intensities before the program are often associated with bad outcomes both in LBP and other musculoskeletal diseases. The debate on the respective influences of depression and anxiety and of fear and believes remains open .
For Wessels disabilities play a greater part in return to work than impairments; but Chambon et al. and Smeets et al. report a decrease of <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='VO2max’>VO2maxVO2max
V O 2 max
values in chronic LBP.
Sullivan et al. highlight the importance of the work environment in addition to the psychosocial context in determining the probability to return to work. This could be a major issue and lead to a double approach combining individual components but also the reality of the work context as proposed in the predictive factors developed by Proctor et al. . Over-reaction creates disability more surely than purely physical impairments as described by Genêt et al. . This environmental approach of the LBP worker has been particularly developed by Loisel and justifies the concept of “therapeutic return to work” . In a similar approach, Linton et al. include the family and relatives of the patients in the context .
In chronic LBP, networking is necessary and should include rehabilitation facilities, occupational specialists, and the work environment. This allows communication of the conclusions of the program and progressive return to work and requires that all information can be shared between the patient, relatives, service providers, healthcare facilities as in some of the Canadian models .
1.8
Conclusion
Despite the methodological difficulties, these results show that the benefit of a functional restoration program remains significant at 2 years follow-up in terms or reduction of sick leaves.
Determining factors correlated with the return to work is difficult, in part because of the lack of power of our study but also because many different factors coexist, are interdependent, none of them being in itself determinant.
2
Version française
2.1
Introduction
Le problème du retour à l’emploi des lombalgiques chroniques demeure un problème de santé publique de premier ordre comme en témoigne le récent rapport du Centre fédéral d’expertise des soins de santé belge, KCE .
La lombalgie chronique est fréquente : 58 % des salariés de Pays-de-la-Loire disent avoir souffert de lombalgies dans l’année et 7 % de façon quotidienne d’après une étude épidémiologique du réseau de surveillance des TMS . Ses conséquences sociales sont mises en lumière par l’équipe d’Annette Leclerc dans un récent rapport de l’Inserm . De plus, la caractéristique essentielle de ce véritable fléau est la survenue d’incapacités prolongées dans un nombre réduit de cas comme l’illustrait déjà le rapport Spitzer et al., il y a 20 ans .
Au cours des deux dernières décennies, plusieurs types d’approche ont été développés. De nombreux travaux ont analysé les facteurs de risque de passage à la chronicité et proposé des stratégies thérapeutiques. Le caractère central des éléments psychosociaux, notamment des peurs et croyances relatives au mouvement, a été mis en évidence. Les stratégies d’information thérapeutique ont été de façon croissante ciblée sur ces aspects . Des programmes de traitement des patients lombalgiques chroniques ont été développés . La majorité reposent sur le concept de déconditionnement physique et psychosocial et proposent des interventions multidisciplinaires dont l’objectif est la reprise ou le maintien dans l’activité, notamment professionnelle. Les résultats immédiats de ces programmes sur les limitations des performances physiques initiales sont très significatifs . L’évaluation de ces programmes, notamment dans son versant médicoéconomique, nécessite aussi un suivi, permettant d’analyser le parcours, en particulier professionnel au long cours. Ces données restent actuellement relativement peu disponibles ; la plupart de ces études disposent d’un an de recul et rares sont celles de plus d’un an .
Plusieurs cohortes de patients ont été suivies dans la région de Pays-de-la-Loire depuis 2000 . Les résultats à un an d’une cohorte de 87 patients montraient une diminution de 60 % de la durée des arrêts de travail et un maintien dans l’emploi pour 72 %. L’objectif de la présente étude est d’analyser l’évolution de ces résultats au cours de la deuxième année et de tenter de dégager des facteurs prédictifs de retour ou de maintien dans l’emploi de cette population à haut risque d’exclusion.
2.2
Patients et méthodes
2.2.1
Population
Il s’agit d’une étude prospective ouverte, incluant 87 patients adressés à une consultation pluridisciplinaire entre 1998 et 2001. Les critères d’inclusion étaient :
- •
un âge compris entre 18 et 53 ans ;
- •
lombalgique ou lomboradiculalgique chronique selon les critères de l’Anaes ;
- •
salarié titulaire d’un contrat de travail ;
- •
être en arrêt de travail ou avoir totalisé plus de six mois d’arrêt de travail au cours des deux années précédentes.
Les critères d’exclusion étaient :
- •
l’existence d’une lombalgie secondaire ;
- •
l’existence de troubles articulaires ou neurologiques ne permettant pas le programme de réadaptation à l’effort ;
- •
une désadaptation cardiaque à l’effort sur test d’effort sur cycloergomètre préalable ;
- •
l’existence de troubles psychiatriques ne permettant pas une inclusion dans un groupe.
2.2.2
Intervention
L’intervention comporte, en outre, un programme de reconditionnement à l’effort, réalisé dans deux centres de rééducation selon un protocole identique, décrit de façon complète dans l’étude rapportant les résultats à un an . Ce programme associe une prise en charge kinésithérapique, ergothérapique et psychologique. Il est supervisé par un médecin de médecine physique et de réadaptation et réalisé en hospitalisation complète ou en hospitalisation de jour, six heures par jour, cinq jours par semaine, durant cinq semaines. Cette intervention est associée à une intervention ergonomique sur site avec la concours de l’action régionale d’amélioration des conditions de travail (Aract), selon une méthode inspirée du « diagnostic court » développé par l’Agence nationale des améliorations des conditions de travail (Anact). Elle n’est réalisée qu’après accord de l’entreprise et a concerné 53 des 87 patients. Elle comporte alors un diagnostic impliquant les acteurs en entreprise, l’élaboration de pistes d’action et d’amélioration, une restitution à l’entreprise. Cette intervention est adaptée au contexte de l’entreprise et ne peut être entièrement standardisée.
2.2.3
Évaluation
Le protocole d’évaluation à deux ans est identique à celui utilisé à un an . La souplesse globale est évaluée par la distance doigts–sol, la force des fléchisseurs et extenseurs du rachis par les tests isométriques de Ito et al. et de Sorensen , les capacités de port de charge par le test de Progressive Isoinertial Lifting Evaluation (PILE) , la qualité de vie par l’autoquestionnaire de Dallas , les limitations d’activité par l’autoquestionnaire de Québec , le retentissement psychologique par l’Hospital Anxiety and Depression scale (HAD) .
Les arrêts de travail dont le motif principal est la lombalgie sont mesurés à partir des déclarations du patient.
2.2.4
Analyse statistique des données
Les données quantitatives sont présentées sous forme de moyennes et d’écart-types (S.D.). Les tests statistiques utilisés pour les données indépendantes sont le calcul du Khi 2 pour les variables qualitatives et l’analyse de variance ou le test t de Student pour les variables quantitatives. Les comparaisons avant après sont réalisées à l’aide de tests non paramétriques appariés : test de Wilcoxon et calcul du Khi 2 selon la méthode de Mc Némar pour les variables qualitatives, d’une part, et test de Student pour les variables quantitatives, d’autre part.
Une analyse univariée des facteurs prédictifs de la reprise du travail 24 mois après la rééducation a d’abord été réalisée sur l’échantillon de 61 patients dont le statut de l’emploi a été obtenu à 24 mois. Les variables testées sont le sexe, l’âge, la notion de travail pénible, les antécédents chirurgicaux rachidiens, le fait d’être en arrêt au début de la session de rééducation, le fait d’être en régime « accident de travail », une durée d’arrêt de travail les deux ans qui précèdent le stage au moins égale ou supérieure à un an, les scores de Dallas, les échelles d’anxiété–dépression, l’autoévaluation de la douleur, les valeurs des tests physiques et l’autoévaluation d’une forme physique améliorée (FPA), de la reprise d’une activité sportive de loisir (RASL), de la capacité à travailler (SSCT) en début et/ou en fin de stage.
Une analyse multivariée a été ensuite effectuée à l’aide d’un modèle de régression logistique binaire pas à pas descendant .
Pour cela, les paramètres quantitatifs physiques, psychologiques et de qualité de vie ont été préalablement dichotomisés par rapport à leur valeur médiane afin d’obtenir des classes équilibrées.
Les variables sexe, durée d’arrêt de travail pour lombalgie au cours des deux ans précédant le stage, réalisation complète du programme de rééducation avec action ergonomique ont été forcées dans le modèle logistique. Toutes les variables liées à celle de la « présence au travail » à 24 mois au seuil de 20 % lors de l’analyse univariée ont été inclus dans le modèle logistique dont le seuil de significativité a été fixé à 5 %.
Les analyses ont été réalisées à l’aide du logiciel SPSS pour Windows version 13.0.
2.3
Résultats
À un an, l’évaluation a porté sur 83 cas, car un cas n’a pas achevé le programme, deux ont refusé d’être suivis, un a été perdu réellement de vue ( Fig. 1 ).









