Abstract
Stroke is a leading cause of adult motor disability. The number of stroke survivors is increasing in industrialized countries, and despite available treatments used in rehabilitation, the recovery of motor functions after stroke is often incomplete. Studies in the 1980s showed that non-invasive brain stimulation (mainly repetitive transcranial magnetic stimulation [rTMS] and transcranial direct current stimulation [tDCS]) could modulate cortical excitability and induce plasticity in healthy humans. These findings have opened the way to the therapeutic use of the 2 techniques for stroke. The mechanisms underlying the cortical effect of rTMS and tDCS differ. This paper summarizes data obtained in healthy subjects and gives a general review of the use of rTMS and tDCS in stroke patients with altered motor functions. From 1988 to 2012, approximately 1400 publications were devoted to the study of non-invasive brain stimulation in humans. However, for stroke patients with limb motor deficit, only 141 publications have been devoted to the effects of rTMS and 132 to those of tDCS. The Cochrane review devoted to the effects of rTMS found 19 randomized controlled trials involving 588 patients, and that devoted to tDCS found 18 randomized controlled trials involving 450 patients. Without doubt, rTMS and tDCS contribute to physiological and pathophysiological studies in motor control. However, despite the increasing number of studies devoted to the possible therapeutic use of non-invasive brain stimulation to improve motor recovery after stroke, further studies will be necessary to specify their use in rehabilitation.
1
Introduction
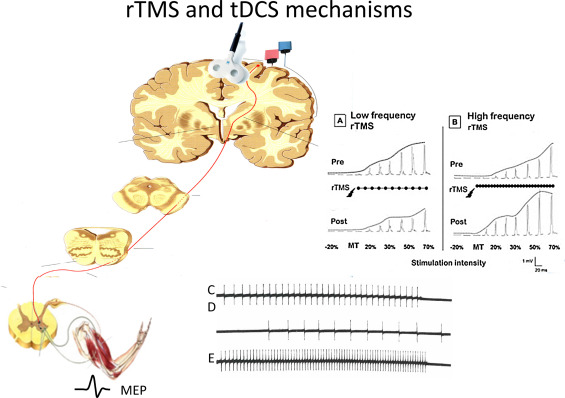
Since the 1980s, the development of non-invasive techniques (electrodes simply positioned on the scalp over the target brain area) allowing for reversible manipulation of the cortex excitability has paved the way to physiological studies in healthy humans. In a second step, these non-invasive techniques were introduced in pathophysiological studies. To briefly summarize the main data , these studies reveal that isolated transcranial magnetic stimulation (TMS) applied over the motor cortex induces a motor evoked potential (MEP) in the target muscle recorded by surface electromyography (EMG) ( Fig. 1 ). Low-frequency repetitive TMS (rTMS < 1 Hz) reduces the excitability of the motor cortex, thus decreasing the MEP amplitude, whereas high-frequency rTMS (>5 Hz) increases it ( Fig. 1 ). Anodal transcranial direct current stimulation (tDCS) increases the motor cortex excitability and cathodal tDCS decreases its excitability ( Fig. 1 ). The effects of rTMS and tDCS are not limited to the motor cortex target area but also affect distant interconnected brain and spinal networks . Both rTMS and tDCS induce after-effects , which is a powerful argument to explore their possible therapeutic effects.
Stroke is a leading cause of long-term adult disability, and the number of patients with chronic motor deficit after stroke is increasing in industrialized countries, despite classical rehabilitation techniques. In the 2004 review by Dobkin, listing the current strategies for stroke rehabilitation, only 60% of patients with hemiparesis achieved functional independence in simple activities of daily living . The author also stressed that the effect of therapeutics is limited during the acute stage and the management of stroke mainly focuses on secondary prevention and rehabilitation.
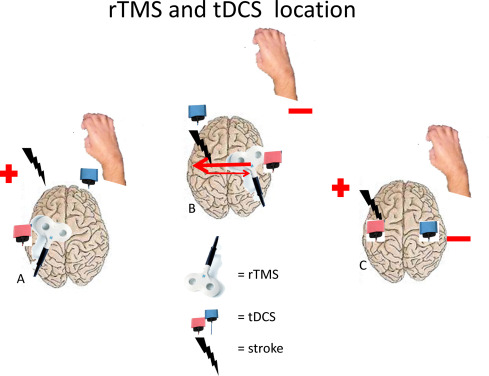
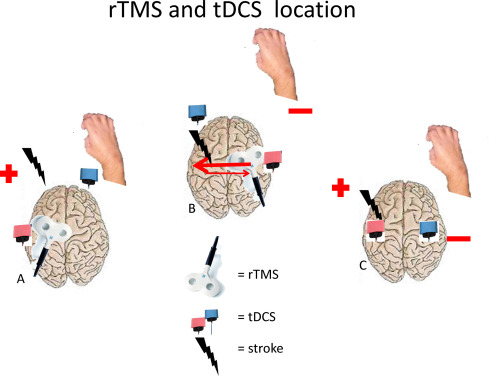
The search to improve rehabilitation during the last decades has led to different strategies to manipulate or induce brain plasticity. An increasing number of studies, involving rTMS and tDCS, are devoted to their possible therapeutic effects to improve motor functions after stroke . These therapeutic trials consisted of excitatory stimuli applied on the motor cortex with a lesion to increase the efficacy of the remaining cells; inhibitory stimuli applied on the non-lesioned cortex to decrease the inhibitory connections from the non-lesioned hemisphere to the lesioned one; and both stimulations combined, with or without traditional rehabilitation and with or without sham stimulation. These studies differ by the characteristics of the stimulation and number of sessions. The outcome measures used to objectively determine the possible effect of these stimulations differed among studies, including in the assessment of the clinical motor function, muscle force or spasticity scales; appreciation of daily living; functional MRI (fMRI); and electrophysiology. They also differed in whether the possible effect was tested during the intervention, immediately after or at longer time after the end of the intervention.
2
Background summary
The mechanisms underlying the effects of rTMS and tDCS applied over the motor cortex are fully described in this special issue . Here, we summarize the central nervous system structures that these stimulations likely involve. Excitatory stimulation enhances the excitability of the motor cortex under the electrodes, thus inducing a facilitatory effect on the contralateral corticospinal tract and the spinal motor neurons. This effect is revealed by an increase in MEP amplitude ( Fig. 1 ). The stimulation over the contralateral motor cortex also likely activates the ipsilateral corticospinal tract in stroke patients, but healthy subjects show no evidence of increased ipsilateral MEP amplitudes. The descending projections from upper motoneurones are not limited to the spinal motor neurones but are also propriospinal nuclei and spinal interneurons . In a given hemisphere, fMRI and magneto-encephalography studies have demonstrated that brain stimulation applied over the motor cortex may affect many brain regions at a distance involving other cerebral areas, basal ganglia and cerebellum. Finally, the homologous cortical area exhibits mutual inhibitory connections between the 2 hemispheres .
In summary, it must be remembered that non-invasive brain stimulation over the motor cortex induces changes in the target motor area but also in many cortico-subcortical and spinal structures. The likely excessive interhemispheric inhibition (IHI) from the non-lesioned hemisphere after stroke has led to exploring the possible therapeutic effects of inhibitory stimulation applied to the non-lesioned hemisphere and also dual stimulation (excitatory on the lesioned hemisphere and inhibitory on the non-lesioned hemisphere) ( Fig. 2 ). In recent years, 4 review articles have summed up the therapeutic trials of rTMS and tDCS performed for about 10 years. In searching MEDLINE via PubMed in February 2015 to identify the trials of rTMS and tDCS interventions in stroke patients with limb motor deficit, we found about 141 references for rTMS and 132 for tDCS. As reported in the 4 reviews quoted above, about 1400 publications involved non-invasive brain stimulation in humans, 180 of these devoted to stroke patients.
The criteria used by the authors of these 4 reviews to retain studies for meta-analysis differ as follows:
- •
Ayache et al. retained all studies devoted to the possible therapeutic effects of rTMS and tDCS on motor function in stroke patients. The authors excluded studies of only purely neurophysiological evaluation. Therefore, 66 studies involving 1785 patients (1343 for rTMS studies and 442 for tDCS studies) were analyzed;
- •
the review by Hsu et al. related to rTMS effects. The criteria used were number of patients involved in each study >5 and only randomized controlled trials. Thus, the authors retained 18 studies involving 392 patients;
- •
the Cochrane review focused on the effects of rTMS for improving function after stroke. Randomized controlled trials coupling rTMS therapeutics with sham or control interventions were included. The studies reporting only laboratory parameters were excluded. After screening 2431 titles and abstracts, the authors included 19 papers involving 588 patients;
- •
the Cochrane review described the effects of tDCS. Only randomized controlled trials and randomized controlled crossover trials were included. From 6231 records identified via database searching, the authors eliminated duplicate records (2726) and retained only studies meeting Cochrane criteria. Thus, only 18 studies involving 450 patients were retained for further analysis.
2
Background summary
The mechanisms underlying the effects of rTMS and tDCS applied over the motor cortex are fully described in this special issue . Here, we summarize the central nervous system structures that these stimulations likely involve. Excitatory stimulation enhances the excitability of the motor cortex under the electrodes, thus inducing a facilitatory effect on the contralateral corticospinal tract and the spinal motor neurons. This effect is revealed by an increase in MEP amplitude ( Fig. 1 ). The stimulation over the contralateral motor cortex also likely activates the ipsilateral corticospinal tract in stroke patients, but healthy subjects show no evidence of increased ipsilateral MEP amplitudes. The descending projections from upper motoneurones are not limited to the spinal motor neurones but are also propriospinal nuclei and spinal interneurons . In a given hemisphere, fMRI and magneto-encephalography studies have demonstrated that brain stimulation applied over the motor cortex may affect many brain regions at a distance involving other cerebral areas, basal ganglia and cerebellum. Finally, the homologous cortical area exhibits mutual inhibitory connections between the 2 hemispheres .
In summary, it must be remembered that non-invasive brain stimulation over the motor cortex induces changes in the target motor area but also in many cortico-subcortical and spinal structures. The likely excessive interhemispheric inhibition (IHI) from the non-lesioned hemisphere after stroke has led to exploring the possible therapeutic effects of inhibitory stimulation applied to the non-lesioned hemisphere and also dual stimulation (excitatory on the lesioned hemisphere and inhibitory on the non-lesioned hemisphere) ( Fig. 2 ). In recent years, 4 review articles have summed up the therapeutic trials of rTMS and tDCS performed for about 10 years. In searching MEDLINE via PubMed in February 2015 to identify the trials of rTMS and tDCS interventions in stroke patients with limb motor deficit, we found about 141 references for rTMS and 132 for tDCS. As reported in the 4 reviews quoted above, about 1400 publications involved non-invasive brain stimulation in humans, 180 of these devoted to stroke patients.