Abstract
Objectives
To evaluate the short- and long-term effectiveness of the multidisciplinary training program (MTP). To show the benefits which the network organization brings to the treatment of chronic low back pain (CLPB).
Methods
The member centres of the Renodos back pain network included 748 subjects in the MTP. The centres used a common evaluation protocol including pain and quality of life visual analogue scales (VAS), fingertip-to-floor distance (FFD), muscle isometric endurance tests, Roland-Morris Disability Questionnaire (RDQ), the Dallas Pain Questionnaire (DPQ) and the Hospital Anxiety Depression (HAD) scale. Measurements were carried out before (T0) and immediately after (T1) the intervention, and at the 3-, 6-, 12-month (T3, T6, T12) follow-up visits.
Results
Statistically discernible improvement occurred for men and women on every outcome measure from before to after the MTP (T0–T1, p < 0.0001). This improvement obtained at T1 was maintained for most of the outcome measures throughout the 12-month follow-up. However, the pain intensity and isometric muscle endurance times showed significant negative evolution. Significant differences between genders were found for the trunk flexibility measurement (FFD), the isometric endurance time of the quadratus lumborum muscle, the RDQ and the HAD depression. There was no time–gender interaction.
Conclusion
The MTP was effective in reducing back pain intensity, functional disability, symptoms of anxiety and depression and in improving quality of life, flexibility and isometric muscle endurance time. It was possible to propose the MTP to both men and women. A network organization effectively contributes to the harmonization of evaluation methods and brings coherence to the treatment of CLBP patients.
Résumé
Objectifs
Évaluer les effets à court et long terme de la prise en charge (PEC) pluridisciplinaire. Montrer les apports bénéfiques d’une organisation en réseau pour le traitement de la lombalgie chronique (LC).
Méthode
Un protocole d’évaluation standardisé comprenant un interrogatoire, un bilan physique et une évaluation du retentissement de la lombalgie a été utilisé pour évaluer 748 patients LC inclus dans la PEC. Les mesures ont été réalisées à l’entrée (T0) et à la sortie (T1) de la PEC, puis lors de visites de suivi à trois, six et 12 mois (T3, T6, T12).
Résultats
L’amélioration des scores entre T1 et T0 a été hautement significative pour tous les paramètres chez les hommes et les femmes et a perduré jusqu’à T12 pour la plupart d’entre eux. Cependant, une évolution négative significative a été observée pour le score à l’EVA douleur entre T1–T3, puis T1–T6 ainsi que pour les scores aux tests d’endurance musculaire entre T1–T3, T1–T6, puis T1–T12. Des différences significatives entre genres ont été observées pour le test de la distance doigts–sol, le temps d’endurance isométrique du muscle carré des lombes, l’échelle d’incapacité fonctionnelle pour l’évaluation des lombalgies (Eifel) et l’échelle Hospital Anxiety and Depression (HAD). Aucune interaction temps genre n’a été observée.
Conclusion
La PEC a montré son efficacité à court et long terme et peut être proposée aux deux genres réunis. L’organisation en réseau contribue efficacement à l’harmonisation des méthodes d’évaluation et apporte de la cohérence dans la PEC et le traitement du patient LC.
1
English version
1.1
Introduction
Multidisciplinary training programs (MTP) are now acknowledged as providing an efficient therapeutic solution in the treatment of chronic low back pain (CLBP) . This approach makes it possible to take the multifactorial nature of this disease into account (physical, psychological, professional and social factors) and requires the intervention of a pluridisciplinary team revolving around and focusing on the patient.
As part of a larger collective intervention, the MTP can be carried out within the framework of a network, a structured level of pluridisciplinarity, which enables the strengthening of interactivity and group dynamics . Currently developing, health care networks aim at the promotion of new and more coherent interventions. They have already proved interesting benefits in the treatment of pathologies such as AIDS and cancer . What about CLBP?
Network experiences in the field of CLBP are still rare and the literature on the subject is lacking. No publication on back pain networks abroad can be found in the international literature. However, a study carried out by Moisan et al. in the West of France showed the advantages of a network organisation within the framework of a program for CLBP patients, to improve their working conditions.
Our work presents the experience of the Renodos back pain network. It is an associative regional structure in the North of France, composed of a group of physicians specialized in spine pathologies, low back pain in particular, working within organized and multidisciplinary structures. The Renodos network first started work aiming at the harmonization of its practices and evaluation methods thanks to the setting up of a standardized evaluation protocol for CLBP patients.
The purpose of this study is to evaluate the short- and long-term effectiveness of the MTP. It also enables reflection both on the quality and efficiency of the Renodos evaluation protocol and on the benefits which a network organization brings to the treatment of CLPB.
1.2
Methods
The study design was a multicenter one, with observational, prospective and non-randomized follow-up.
The Renodos network is an associative structure which owes its foundation to the mobilization of physicians specialized in spine pathologies. They created a leading committee in which they gather to take decisions concerning the orientations, objectives and evaluation of the network. It currently enables cooperation between 22 physicians and their teams of therapists (rheumatologists, rehabilitation physicians, physiotherapists, occupational therapists, psychotherapists, sports therapists, nurses and social workers). It also works in close relationship with external partners (company doctors, medical advisors, general practitioners). The different teams all propose an intervention based on the MTP.
The first action of the Renodos back pain network has been the harmonization of the MTP and the standardization of an evaluation protocol for CLBP. A standard procedure was defined for all the centres within the network. It includes recommendations concerning the duration of the MTP, indispensable human and technical resources, content of both the MTP and of the evaluation protocol.
1.2.1
Multidisciplinary training program
The patients, in groups of four to five, trained for 20 days, spread over a maximal period of 5 weeks. The MTP was carried out in complete or day hospitalization and consisted in physical training including muscle-strengthening (for the trunk, lower and upper limbs), cardiovascular exercises, active stretching, and proprioceptive exercises. The patients were informed that the exercises were progressive and that they should thus start slowly and gently to avoid over-activity.
They also received information and guidance on physiopathological mechanisms of non-specific CLBP, posture and ergonomics, as well as psychological care (conversations, relaxation therapy).
Simultaneously, contact was made with appropriate authorities at their workplace to prepare the patients’ return-to-work (adaptation of the workstation, resumption of part-time work for therapeutic reasons).
The primary goal of the MTP is not to cure the pain but to restore the patient’s daily functioning . It focuses on maximizing the residual capacity of CLBP patients by reducing pain-related behaviour, by increasing the patients’ autonomy, and by encouraging them to take an active role in the rehabilitation process . The patients indeed played the greatest role in their recovery and had to show a willing and motivated attitude (establishing a moral contract with at least an attempt to return to work at the end of the MTP).
Frequent contacts between teams ensured the homogeneity of the MTP.
1.2.2
Evaluation protocol
Assessments were carried out at four times: before (T0) and immediately after (T1) the intervention, and at the 3 and 6 and 12-month (T3, T6, T12) follow-up visits.
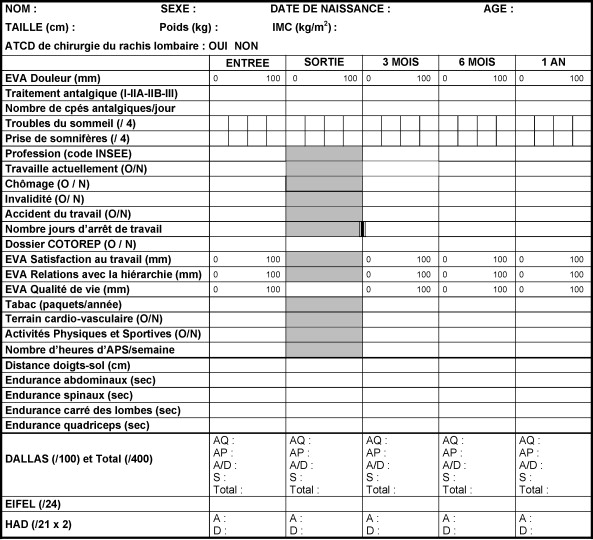
Paying special attention to the harmonization of the evaluation methods used by the therapists, the Renodos network worked on a standardized evaluation protocol using tools previously validated in the literature and reproducible between observers. It created a grid and its form-filling guide ( Fig. 1 ) covering the selected criteria of the evaluation protocol. The following measurements were performed:
- •
pain intensity and overall assessment of quality of life by the patient were measured on visual analogue scales (VAS) with a score from 0 to 100 mm;
- •
trunk flexibility was measured by fingertip-to-floor distance (FFD) ;
- •
muscle isometric endurance was evaluated with the duration of isometric contraction of the abdominal and spinal muscles, as described by Ito et al. (Ito test) and Biering-Sorensen (Sorensen back endurance test) , quadratus lumborum (side bridge test McGill ) and quadriceps muscles (chair test);
- •
functional status was assessed with the validated French adaptations of the Roland-Morris Disability Questionnaire (RDQ) and the Dallas Pain Questionnaire (DPQ) . The RDQ (24 yes/no items) measures the patients’ self-rated disability due to back pain, the final score ranging from 0 (no disability) to 24 (severe disability);
- •
the Dallas Pain Questionnaire assesses the impact of the chronic pain in four aspects of the patients’ lives: daily activities, work and leisure activities, as well as perceived anxiety-depression and social interest. These four aspects constitute categories (score from 0 to 100%) among which 16 items are distributed;
- •
the psychological profile of the patient was assessed by the Hospital Anxiety Depression (HAD) scale . This is divided into an anxiety subscale (HAD a ) and a depression subscale (HAD d ), both comprising seven intermingled items .
1.2.3
Studied population
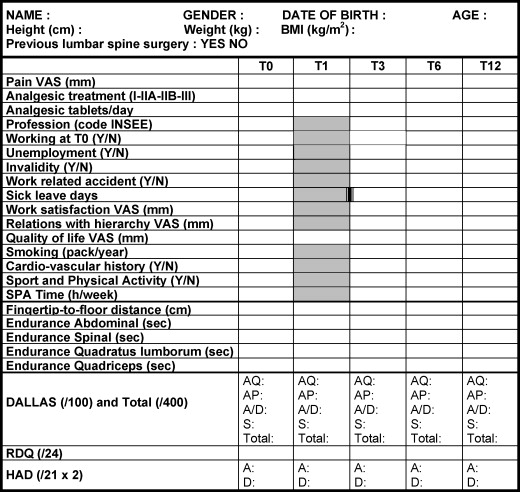
Seven hundred and forty-eight patients (371 men, 377 women) with CLBP coming from seven centres in the network initially entered the study between 2002 and 2006 ( Fig. 2 ).
1.2.3.1
Inclusion criteria
Men and women suffering from CLBP with:
- •
a symptomatology evolving for more than 3 months with: a considerable impact on the patient’s life (above 8 on the RDQ); a pain intensity above 50 mm on the VAS, and the impact of chronic pain on the patient’s daily life assessed by the DPQ:
- ∘
as moderate (four categories below 50%), with sufficient muscle endurance (above 2 min in the isometric endurance test), only needing MTP in case of high pain intensity (VAS > 50 mm),
- ∘
as moderate or intermediate (first two categories above 50%, last two categories below 50%), with intermediate muscle endurance,
- ∘
with strong psychological impact (four categories above 50%), included in the MTP only if the systematic psychological interview allows to envisage an efficient intervention within a group;
- ∘
- •
a lower lumbar pain, which may radiate to the buttocks without reaching the knees, persisting for at least 3 months;
- •
a mechanical characteristics without inflammatory symptomatology;
- •
a normal neurological examination;
- •
an absence of predominant radicular pain (sciatic or crural).
1.2.3.2
Exclusion criteria
Patients with symptomatic back pain (spondylitis or tumour) and major psychological affection were not included.
1.2.4
Statistics
The two sample t test for continuous data and the Pearson’s Chi 2 test were used to analyse the differences in baseline characteristic of men and women. A linear mixed model for repeated measurements was used to analyse the between-groups effects of changes in each outcome variable at separate time points and the within-group changes.
The linear mixed model has the ability to accommodate missing data often encountered in longitudinal datasets. It takes all available information into account and deals with intrasubject correlation.
Then, a Bonferroni posthoc multiple comparison test was carried out. All analyses were performed using SAS 9.1 software. Significance was defined as p < 0.05.
1.3
Results
Fig. 2 presents the location of the centres and the number of patients from each of them. Of the 748 patients, 476 (63,6%: 227 men – 249 women), 292 (39,0%: 145 men – 147 women), 97 (12,9%: 56 men – 41 women) completed the study at the 3, 6 and 12-month follow-ups, respectively.
When men were compared with women for baseline characteristics, no statistically significant difference concerning age, medical history, working at T0, cardiovascular history or sporting and physical activity was found ( Table 1 ). However, the men were heavier and taller than the women, and they had a higher BMI than women ( p < 0.05). A greater number of men were smokers in comparison with women ( p < 0.05).
| Men ( n = 371) | Women ( n = 377) | P | |
|---|---|---|---|
| Age (yr) | 42.3 ± 8.9 | 42.8 ± 9.2 | ns |
| Body mass index (kg/m 2 ) | 26.6 ± 4.4 | 25.7 ± 5.1 | < 0.05 |
| Medical history (%) | 12.9 | 11.6 | ns |
| Working at T0 (%) | 27.1 | 28.0 | ns |
| Smokers (%) | 24.8 | 14.4 | < 0.05 |
| Cardiovascular history (%) | 5.5 | 4.6 | ns |
| Sport and physical activity (%) | 11.9 | 13.6 | ns |
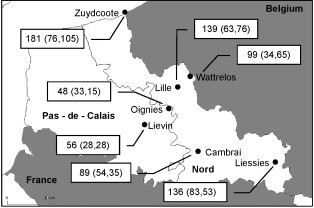
Table 2 provides details of changes over the 12-month follow-up in all the outcome measures for men and women separately. Statistically discernible improvements occurred in both groups for every outcome measure before and after the MTP (T0–T1, p < 0.0001). Concerning the results at follow-up ( Fig. 3 ), non-significant differences were found, with the exception of the pain VAS and the isometric endurance tests. These results mean that the improvement obtained at T1 was maintained for most of the outcome measures throughout the 12-month follow-up.
| Outcome measure | P value for time effect | P value for gender effect | P value for time–gender interaction |
|---|---|---|---|
| Pain VAS (0–100 mm) | < 0.0001 | 0.79 | 0.50 |
| Quality of life VAS (0–100 mm) | < 0.0001 | 0.37 | 0.48 |
| FFD (cm) | < 0.0001 | 0.002 | 0.67 |
| Abdominal (sec) | < 0.0001 | 0.09 | 0.56 |
| Spinal (sec) | < 0.0001 | 0.69 | 0.95 |
| Quadratum lumborum (sec) | < 0.0001 | < 0.0001 | 0.17 |
| Quadriceps (sec) | < 0.0001 | 0.05 | 0.28 |
| DPQ total score (/400) | < 0.0001 | 0.18 | 0.08 |
| RDQ (0–24) | < 0.0001 | 0.0002 | 0.50 |
| HAD anxiety (0–21) | < 0.0001 | 0.06 | 0.23 |
| HAD depression (0–21) | < 0.0001 | 0.02 | 0.23 |
Indeed, it should be noted that there was either no decrease in the results, or merely a slight one, between T1–T3, T1–T6 and T1–T12, but also between T3–T6, T3–T12 and T6–T12, although the subjects had been discharged from the MTP. Nevertheless, although the MTP was effective in reducing pain intensity and improving muscle isometric endurance in the short term (T0–T1), the improvement tended to diminish during the follow-up. Indeed, negative significant differences were observed for pain VAS between T1–T3 ( p < 0.002) and T1–T6 ( p < 0.0005). Negative significant differences were also found for the isometric endurance of the abdominal, spinal, quadratus lumborum and quadriceps muscles ( p < 0.0001) between T1–T3, T1–T6 (except for the quadriceps muscle for this last comparison where the result was non-significant) and T1–T12.
There was no significant difference between genders for the isometric endurance time of the abdominal, spinal and quadriceps muscles. Neither was there significant difference for the VAS scores for pain intensity and quality of life both in the DPQ and HAD anxiety. However, there were significant differences for the trunk flexibility measurement (FFD), the isometric endurance time of the quadratus lumborum muscle, the RDQ and the HAD depression. The data for men and women were therefore combined ( Fig. 3 ; left column) except for these 4 outcome measures; for the latter, it was of particular interest to make the differences between genders visible ( Fig. 3 ; right column).
The greatest differences between men and women occurred in the quadratus lumborum muscle endurance time ( p < 0.0001) and in RDQ score ( p = 0.0002). Men had a longer mean quadratus lumborum isometric endurance time. The scores in the Roland-Morris Disability Questionnaire showed that the impact of chronic pain on the patient’s life was more important for men than women. Women had lower mean scores than men in the FFD measure ( p = 0.002) and the HAD depression ( p = 0.02).
Finally, no time gender interaction was found.
1.4
Discussion
1.4.1
Short- and long-term effectiveness of the MTP
The multidisciplinary training program resulted in significant improvements among the patients by the end of the program. In addition, the results were maintained at follow-up. The MTP was effective both for men and women in reducing back pain intensity, functional disability, symptoms of depression and anxiety and in improving their quality of life, flexibility and isometric muscle endurance time between T0 and T1 but also between T0–T3, T0–T6 and T0–T12. These findings confirm those already found in the literature .
The results did not show time gender interaction, which means that scores and measures increased or decreased equally for both men and women. It is thus possible to propose the MTP to men and women altogether since they progress at the same rhythm, at the same level, or at a different but parallel one.
Furthermore, the absence of significant difference between genders for most of the parameters studied allowed the data to be processed and results analyzed without needing to differentiate between genders. However, it has to be noted that differences between men and women were found for four parameters.
To our knowledge, no work in the literature has studied gender differences in the FFD, the RDQ, the HAD and the quadratus lumborum muscle fatigue. However, Clark et al. showed that women exhibited significantly greater endurance for back extensor muscles during isometric trunk extension than men. Moreover, Kankaanpaa et al. suggests that women fatigue more slowly (better endurance time) than men in the Sorensen back endurance test (spinal muscle). This finding is in agreement with that observed in other studies but our results did not allow us to confirm it. Indeed, we did not find any significant difference between men and women for the spinal muscle endurance time.
According to the findings of our study, the differences in scores between men and women for these four parameters do not call into question the fact of proposing them the same MTP, since these differences do not disturb the individual improvement, which represents the main objective of this program.
The decrease in muscle isometric endurance times between T1 and T3 for both genders showed that the period following the program is often a difficult stage for patients. It is thus very important to incite them to pursue their efforts to maintain the results obtained during the intervention over the long-term . To make the patients aware of the benefits of the regular practise of a physical activity is one of the most important aims of the MTP. The therapists working within the network therefore have an essential role to play. They have to bear this point in mind in order to be able to transfer this awareness to the patients. For their part, to help the patients pursue a physical training, the sports therapists of the network worked on the creation of a training guide to use after hospitalization.
Finally, due to the difficulties encountered with the drop-out rate in this study, the results at T12 have to be interpreted cautiously and one of the network’s objectives for the future will be to try to monitor patients further at 6- and 12-month follow-up .
1.4.2
Quality and efficiency of the Renodos evaluation protocol
The Renodos network’s first priority was to work on harmonizing its practices and evaluation methods and the setting up of a standardized evaluation protocol for CLBP patients. This study showed that it is possible to draw up a standardized and validated evaluation grid allowing multicentre studies.
Nevertheless, since the evaluation methods remain perfectible, efforts to reach standardization and harmonization within the scope of a quality and efficiency process are ongoing within the network. The form-filling guide has recently been modified to further standardize the instructions given for the isometric endurance muscular tests . Indeed, it is important to minimize the methodological variations, which could generate disparities in the results .
Subsequent to the findings in our study, the Renodos network has given thought to the evolution which its evaluation protocol should follow. Certain initially selected criteria have been questioned and the need to integrate new ones identified.
The question “do you practise a physical activity?” regarding the criterion “sport and physical activity” ( Fig. 1 ) is very open, leaving room for numerous interpretations, and the answers received are thus difficult to use. As a result, the sports therapists in the network are contemplating the use of a physical condition test on a cycloergometer, which would give more objective results.
Moreover, the only psychological dimension evaluated in the current protocol being anxiety disorders and depression (HAD), it has been agreed among the psychologists in the network to add the “Coping Strategy Questionnaire” . This questionnaire allows us to assess cognitive and behavioural pain coping strategies that subjects use when they feel pain. The importance of psychosocial and environmental factors in CLBP is now being recognized , thus it seemed necessary to take it into account in the protocol.
1.4.3
Benefits of a network organisation for the treatment of CLPB
Network organization first of all effectively contributes to the harmonization of evaluation methods; harmonization rather than homogenisation, to leave room for the therapists’ expression and initiatives, which enriched the network and gave it flexibility. Knowledge sharing, consultation between dynamic and motivated teams, as well as discussions on intervention conditions have optimized the Renodos network activity. These exchanges, developed through the setting up of working groups intended for the therapists within the network, have allowed the protocol to progress and guarantee stable utilisation.
Fruitful communication between the evaluators has played an essential role in the quality of the proposals put forward. As a network organization lends itself to the transmission of important messages, the emulation between the therapists involved is facilitated and the value of their work enhanced. The keystone of the coordination within the Renodos lies in the circulation of information .
Such a network is characterized by group dynamics and therefore constitutes a privileged field for collectively building up new professional references .
The main objective being to provide better treatment for CLBP, energies are focused on the patient, who is at the centre of this network’s dynamics. This mode of functioning brings coherence to the treatment of patients. They feel confident and secure in an environment where all the therapists use a common language. This “area of confidence” which surrounds them is a key element in the success of their treatment.
One of the characteristics of network action is its long-term influence. Establishing patient follow-up up to one year after treatment is another key point: It allows the maintenance of patients’ motivation and the preservation of the positive effects of the Renodos intervention through the MTP. The network hopes to increase the number of patients benefiting from this long-term follow-up.
During the follow-up visits, the patients get to meet again the therapists who took care of them. Simultaneously, the training guide set up by the sport therapists involved in the network helps the patients to pursue their efforts between and after these visits. It would be necessary to follow them through the evaluation of their sport activities after the MTP.
The Renodos network puts forward the following as priority fields for further development:
- •
links with sports associations in a position to help the patient to pursue physical activity. This action is carried out in a social context and also focuses on the long term, with the aim of making the patient autonomous (instead of using periodical refresher training in rehabilitation centres);
- •
links with physiotherapists and general practitioners, to share the network experience through training and information sessions . Contacts have been made with company doctors from the North of France.
1.5
Conclusion
The convincing results achieved by the Renodos network not only give credibility to multidisciplinary back training as treatment for CLBP, but also bring about recognition by other physicians, authorities, clinics, etc. The best outcome would be for this Renodos experience to lead to the creation of new CLBP networks, which are currently still too scarce.
What is important now is to maintain the motivation of the therapists involved, as this is essential to foster the efficient functioning of the network. Still at an early stage in its development, the Renodos network needs to strengthen its experience and pursue its development by opening up to the outside and to other networks. Exchanges with the latter, both in France and abroad, present a major interest and thus constitute a future priority.
2
Version française
2.1
Introduction
Le réentraînement à l’effort en prise en charge (PEC) pluridisciplinaire est à présent reconnu comme une voie thérapeutique efficace dans le traitement de la lombalgie chronique . Cette approche permet de prendre en compte le caractère multifactoriel de cette pathologie (facteurs physiques, psychologiques, professionnels, sociaux), avec l’intervention d’une équipe pluridisciplinaire centrée sur le patient.
Dans le cadre d’une intervention collective plus large, cette activité pluridisciplinaire peut s’exercer en réseau, niveau structuré de pluridisciplinarité, qui permet d’accroître l’interactivité et la dynamique de groupe . En plein développement, les réseaux de soins doivent permettre de promouvoir de nouvelles prises en charge plus cohérentes des patients. L’organisation en réseau a déjà prouvé son efficacité dans le traitement de pathologies chroniques telles que le sida et le cancer . Qu’en est-il pour la lombalgie chronique ?
Les expériences de réseaux dans le domaine de la lombalgie sont encore rares et la littérature sur le sujet est pauvre. D’après nos recherches, la littérature internationale ne semble pas proposer d’études sur des réseaux de lombalgie à l’étranger. À noter toutefois que, dans une région de l’ouest de la France, un travail réalisé par Moisan et al. a montré les bénéfices tirés d’un fonctionnement en réseau dans le cadre d’un programme de maintien dans l’emploi de lombalgiques chroniques.
Notre étude présente l’expérience du Réseau Nord-Pas-de-Calais du DOS (Renodos). Le Renodos est une structure associative régionale du Nord de la France constituée de médecins spécialistes prenant en charge des pathologies rachidiennes, en particulier lombaire chronique, au sein de structures organisées et pluridisciplinaires. Le Renodos a entrepris de travailler pour harmoniser ses pratiques et mettre en place un protocole d’évaluation standardisé des patients.
L’objectif de cette étude a été prioritairement d’évaluer les effets à court et long terme de la PEC au sein du réseau. Notre travail visait aussi parallèlement à mener une réflexion sur la qualité et l’efficacité du protocole d’évaluation Renodos et l’apport bénéfique d’une organisation en réseau pour le traitement de la lombalgie chronique.
2.2
Patients et méthode
L’étude réalisée a été observationnelle, multicentrique, prospective et non randomisée.
Le Renodos est une structure associative qui s’est constituée grâce à la mobilisation de médecins spécialistes de la Région Nord-Pas-de-Calais, en charge des pathologies rachidiennes, notamment lombaire chronique. Ils se sont organisés en comité de pilotage participant à la prise de décision quant aux orientations du réseau, aux objectifs qu’il se fixe et aux évaluations. Ce réseau permet actuellement la collaboration entre 22 médecins membres actifs et leurs équipes de thérapeutes (médecins rhumatologues, rééducateurs, kinésithérapeutes, ergothérapeutes, psychologues, éducateurs sportifs, infirmières, assistantes sociales). Il fonctionne également en relation avec des partenaires extérieurs (médecins du travail, médecins conseils de caisse, médecins généralistes). Les différentes équipes proposent toutes une PEC pluridisciplinaire de type réentraînement à l’effort.
La première action du Renodos a été d’entreprendre l’harmonisation de la PEC pluridisciplinaire et la standardisation des pratiques d’évaluation des patients lombalgiques chroniques. Dans ce cadre, un « cahier des charges » minimum commun à tous les centres a été défini comprenant la durée de la prise charge, les moyens humains et techniques indispensables, le contenu de la PEC pluridisciplinaire et du protocole d’évaluation.
2.2.1
PEC pluridisciplinaire
La PEC s’effectue dans chaque centre sur 20 journées, sur une période maximale de cinq semaines, par groupe de quatre à cinq sujets. Elle se déroule en hospitalisation complète ou en hôpital de jour et comprend invariablement des exercices de renforcement musculaire des quatre membres et du tronc, un travail des capacités aérobies, des étirements actifs et de la proprioception. Le patient reçoit une éducation quant aux mécanismes physiopathologiques de la lombalgie commune et aux méthodes d’économie rachidienne. Il est aussi guidé vers l’auto entraînement, l’hospitalisation devant être suivie par la réalisation régulière d’un programme d’exercices personnel et d’activités physiques plus globales, sportives notamment.
Parallèlement, une PEC psychologique du patient est assurée (entretiens, séances de relaxation ou de sophrologie) et un contact est pris avec le milieu du travail pour préparer au mieux la reprise professionnelle (aménagement ou changement du poste de travail, reprise en mi-temps thérapeutique, par exemple).
L’objectif premier de la PEC n’est pas le traitement de la douleur mais la restauration fonctionnelle du patient qui reste l’acteur principal de l’amélioration de son état. Il est encouragé a avoir un rôle actif dans sa PEC et se doit d’être volontaire et motivé (mise en place d’un contrat moral).
Des échanges réguliers entre les équipes de thérapeutes des différents centres assurent l’homogénéité de la PEC proposée au sein du réseau.
2.2.2
Protocole d’évaluation
Chaque patient a été évalué à l’entrée (T0) et à la sortie (T1) de la PEC, puis lors de visites de suivi fixées à trois mois (T3), six mois (T6) et un an (T12) après la fin de la PEC.
Le Renodos dispose d’une grille d’évaluation ( Fig. 1 ), accompagnée d’un guide de remplissage. Les critères d’évaluation ont été sélectionnés par les membres du Renodos dans un souci d’harmonisation des pratiques au sein du réseau. Les outils d’évaluation ont fait l’objet d’un choix rigoureux, au regard de leurs qualités métrologiques (validité, fidélité, sensibilité au changement). La grille récapitule les différentes étapes du protocole d’évaluation qui comporte un interrogatoire standardisé, un bilan physique et une évaluation du retentissement de la lombalgie. Au cours de ces étapes les mesures suivantes ont été effectuées :
- •
l’évaluation de l’intensité de la douleur du patient et l’estimation de sa qualité de vie ont été réalisées à l’aide d’échelles visuelles analogiques (EVA) . L’intensité de la douleur (EVA douleur) correspond à la distance en millimètres entre la position du curseur déplacé manuellement par le patient et l’extrémité « pas de douleur » de l’échelle (0 mm), l’autre extrémité comportant la mention « la pire douleur imaginable » (100 mm). L’échelle de la qualité de vie (EVA qualité de vie) comporte à ses extrémités les mentions « la pire » (0 mm) et « la meilleure imaginable » (100 mm) ;
- •
la mobilité générale est mesurée à l’aide du test de la distance doigts–sol (DDS) ;
- •
l’endurance isométrique des abdominaux a été évaluée avec le test de Ito , celle des spinaux avec le test de Sorensen , celle du carré des lombes avec le « side bridge test » de McGill et enfin celle des quadriceps avec le test de la chaise encore nommé test de Killy ;
- •
le retentissement fonctionnel de la lombalgie a été mesuré avec l’échelle d’incapacité fonctionnelle pour l’évaluation des lombalgies (Eifel) , version française validée du Questionnaire Roland-Morris . Vingt-quatre items sont à cocher. Plus le patient coche d’items, plus son incapacité fonctionnelle sera importante ;
- •
le retentissement de la douleur lombaire dans la vie quotidienne du patient a été quant à lui évalué à l’aide de la version française validée de l’autoquestionnaire de Dallas (Dallas) . Le score total de l’indice fonctionnel du questionnaire de Dallas (sur 400) correspond à la somme des quatre moyennes des catégories « activités quotidiennes », « travail/loisir », « anxiété/dépression » et « sociabilité ». Plus le score est élevé, plus le retentissement est important ;
- •
le retentissement psychologique de la lombalgie est apprécié à l’aide de l’échelle « Hospital Anxiety and Depression » (HAD) validée en français par Lépine et al. . Cette dernière mesure les composantes anxieuse et/ou dépressive. Chaque composante évaluée affiche une échelle comprise entre 0 et 21, les réponses étant cotées de 1 à 3. Les scores les plus élevés correspondent à une symptomatologie plus sévère .