CHAPTER 33 Volar Carpal Ganglion Cysts
Use of the arthroscope for diagnosis and management of wrist disorders has evolved significantly since Roth first described the technique of wrist arthroscopy in 1988.1 The development of sophisticated optical systems and instruments specific for small joint applications has enabled the experienced wrist arthroscopist to perform complex reconstructive procedures. Wrist arthroscopy facilitates visualization of intra-articular anatomy, whereas small, motorized shavers enable resection and elimination of intra-articular and capsular lesions.
In 1995, Osterman and Raphael presented a technique for the arthroscopic treatment of ganglion cysts arising from the dorsal portion of the scapholunate interosseous ligament and manifesting as dorsal space-occupying lesions.2 The initial skepticism regarding treatment of this lesion has been quelled, and arthroscopic treatment of dorsal cysts has become routine for experienced arthroscopists. Although the anatomic origin of volar carpal ganglions has not been as well defined as for their dorsal counterparts and the location is not as consistent as for the dorsal ganglion, many of these cysts do have an intra-articular capsular origin.3–5 Arthroscopic resection of volar ganglia is an effective technique with potential advantages when compared with traditional open techniques.
ANATOMY
Ganglion cysts are saclike structures that do not have a true cellular lining. They are benign soft tissue tumors that are most commonly found in the wrist but may occur adjacent to or originating from any joint. Approximately 10% of the time, they form from tendon sheaths. They are filled with a viscous fluid that contains glucosamine, albumin, globulin, and hyaluronic acid.6 The origin of most ganglion cysts is idiopathic. Occasionally, a traumatic event precedes the development of a cyst, lending support to a possible traumatic origin of these lesions. Mathoulin’s histologic analysis of ganglion cysts indicates that the base of the cyst arises in the histologic layer between the synovium and the joint capsule.7 His group postulates that this area is exposed to stress that initiates histologic degenerative lesions, particularly mucoid degeneration. These masses are not inflammatory, and they do not arise as simple herniations from the joint capsule.6,8 Other causative factors are capsular rents caused by preexisting joint pathology, synovial fluid leakage with secondary cyst formation, and mucoid degeneration or mucin secretion stimulated by joint stress or other degenerative processes. Occult volar ganglia may also contribute to volar wrist pain without a visible or palpable mass. Symptoms may be caused by capsular injury, inflammatory changes, or local pressure.
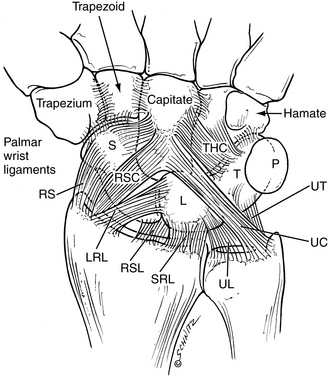
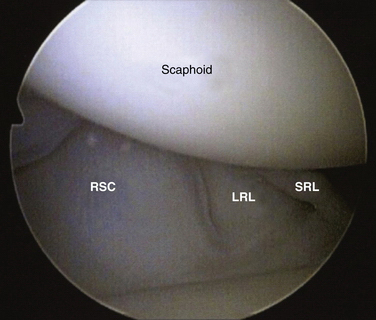
The anatomic origin of the volar ganglion cyst is not as well defined as that of its dorsal counterpart. The literature suggests a radioscaphoid, scaphotrapezial, or trapeziometacarpal (TM) joint origin.9 Volar cysts may also arise from the flexor carpi radialis (FCR) tendon sheath or other aberrant locations. Aydin and colleagues studied open excision of volar ganglions and reported that 45% arose from the radiocarpal joint, 40% from the scaphotrapeziotrapezoid (STT) joint, and 5% from the FCR sheath.10 Most arise from the radiocarpal joint, and when they do, they have a volar capsular origin from the relatively deficient area between the radioscaphocapitate (RSC) and long radiolunate (LRL) ligaments.4,11 The ligaments represent the volar extrinsic components that work in conjunction with the intrinsic and extrinsic dorsal ligaments and with the interosseous ligaments to provide wrist stability. Starting radially and proceeding in an ulnar direction, they are the RSC, the LRL, and the short radiolunate (SRL) ligaments (Fig. 33-1). When they are visualized arthroscopically, distinct clefts can be seen between these ligaments. The volar ganglion cyst can be identified in the clefts between the extrinsic radiocarpal ligaments. Ho and associates, in their study on arthroscopic resection of volar carpal ganglia, observed that 75% of the cysts arose from the interval between the RSC and LRL, and 25% originated between the LRL and SRL.3 The capsular origin can be visualized arthroscopically (Fig. 33-2).
PATIENT EVALUATION
History and Physical Examination
Most ganglion cysts occur in women in their second, third, or fourth decade of life. The onset is usually insidious, with a progressive increase in size occurring over many years. The ganglion usually manifests as a visible and palpable mass. Patients may relate a traumatic event, such as a wrist hyperextension injury, that occurred before the cyst appeared; however, most cannot recall an event or activity related to the development or appearance of the mass. The masses may be painful, and the symptoms usually are described as an aching discomfort in the region of the mass. Cosmetic dissatisfaction and concern that the mass represents a malignancy are associated complaints. A painless mass is the most frequent presenting complaint.12 Westbrook’s study of 50 patients indicated that a minority of patients presented with pain, 38% presented because of the cosmetic appearance of the mass, and 28% were concerned that the ganglion was malignant.13
The diagnosis is easily made with visual inspection (Fig. 33-3). A 1- to 2-cm, round or ovoid mass usually manifests as a visible fullness in the interval between the FCR tendon and the radial artery. It may be unilobular or multilobular. Palpation reveals a mass that may be slightly tender. The consistency is usually soft and compressible, although chronic lesions may be quite firm. Transillumination with a penlight usually confirms the diagnosis. The differential diagnosis includes vascular lesions of the radial artery, and it is important to determine whether the mass is pulsatile or the pulsations of the radial artery can be distinguished from the mass itself. Despite the relatively easy diagnosis, it is important to exclude other causes of wrist discomfort, such as radiocarpal arthrosis, STT arthrosis, TM arthrosis, DeQuervain’s tendonitis, and FCR tendonitis. Isolated loading and stress testing of the individual joints should not produce any pain if the joint is not arthritic. The result of a Finkelstein maneuver should be negative, and there should be no tenderness of the first dorsal compartment tendons. Resisted wrist flexion should produce no pain over the FCR tendon. In patients with an occult volar ganglion cyst, the only positive physical finding may be fullness in the FCR–radial artery interval and pain with pressure in the region. Exclusion of other potential causes of volar radial wrist pain is essential.
Diagnostic Imaging
If the diagnosis is certain and the physical examination presents no confounding findings, imaging is not necessary. Wong and colleagues showed that radiographic abnormalities were diagnosed in only 13% of patients with ganglion cysts, and treatment was affected in only 1% of the cases in their study. They concluded that routine radiographs are not cost-effective.14 When desired, plain radiographs are usually sufficient as an imaging study to exclude arthrosis of the STT or TM joint. Arthroscopic management of volar ganglions is indicated only for capsular radiocarpal origins; preoperative radiographs that demonstrate arthrosis raise suspicion that the cyst may arise from a location other than the radiocarpal joint. If the nature of the mass is unclear, ultrasound or magnetic resonance imaging is useful. Ultrasound is a cost-effective study that demonstrates the mass as a hypoechoic lesion. Wang and associates were able to localize the stalk-like origin of the ganglion emanating from the volar radiocarpal joint in 7 of 15 cysts. They also found that small cysts can be hypoechoic or anechoic, and not all fulfill the ultrasound criteria for simple cysts.5