Anatomy
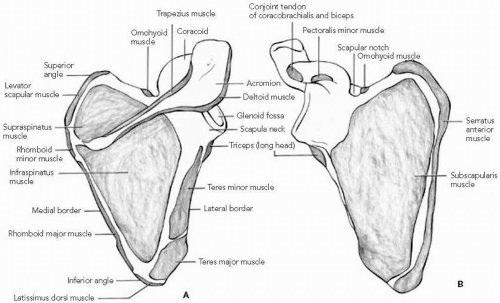
The scapula is enveloped by multiple layers of muscles. The anterior surface provides attachment for the subscapularis, serratus anterior, omohyoid, pectoralis minor, conjoined tendon of the coracobrachialis and short head of the biceps, long head of the biceps, and long head of the triceps (
Fig. 18-2).
37 The posterior surface of the scapula provides muscular attachment sites for the levator scapulae, the rhomboid major, the rhomboid minor, the latissimus dorsi, the teres major, the teres minor, a portion of the long head of the triceps, the deltoid, the trapezius, the supraspinatus, the infraspinatus, and a portion of the omohyoid (
Fig. 18-2).
37 The intramuscular position of the scapula provides it with great mobility and a protective cushion that are no doubt responsible for the low incidence of scapular injury.
The close proximity of neurovascular structures to the scapula places them at risk for injury. The pectoralis minor tendon inserts at the base of the coracoid process and the lateral border of the suprascapular notch. The brachial plexus and axillary artery travel posterior to the pectoralis minor tendon. The suprascapular nerve traverses through the suprascapular notch to innervate the supraspinatus muscle, whereas the suprascapular artery passes over it. The suprascapular nerve continues through the spinoglenoid
notch to innervate the infraspinatus muscle. At the medial border of the scapula, the dorsal scapular and spinal accessory nerves descend along the thorax, along with branches of the transverse cervical artery.
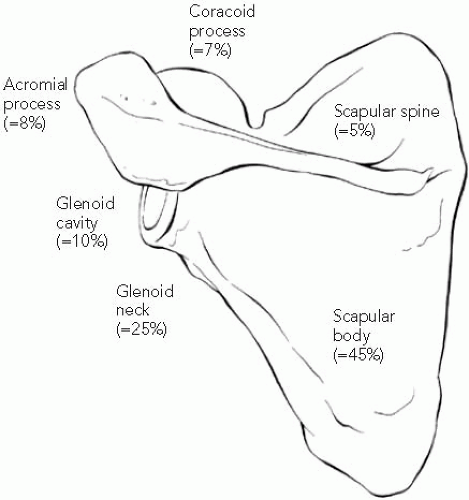
The osseous components of the scapula, which consist of the body and spine, coracoid process, acromion process, glenoid, and inferior angle, arise from several ossification centers.
67 At birth, the body and spine form one ossified mass. However, the coracoid process, acromion process, glenoid, and inferior angle are all cartilaginous. The coracoid process is a coalescence of four or five centers of ossification. The center of ossification for the midportion of the coracoid appears at age 3 to 18 months and may be bipolar. The ossification center for the base of the coracoid, which includes the upper third of the glenoid, appears at 7 to 10 years. Two ossification centers appear at age 14 to 16 years: a center for the tip and a shell-like center at the medial apex of the coracoid process. The ossification centers for the base and the midportion of the coracoid coalesce during adolescence at age 14 to 16 years. The other ossification centers fuse at the age of 18 to 25 years.
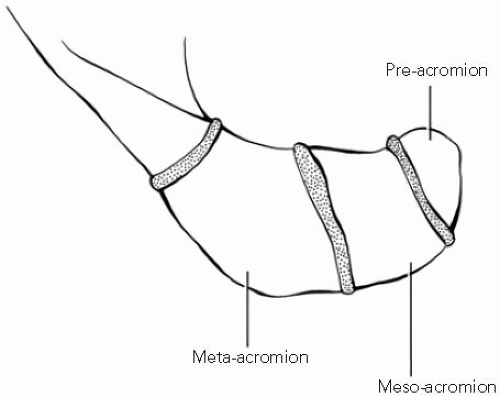
The acromion is a coalescence of two or three centers of ossification that appear between the ages of 14 and 16 years, coalesce at the age of 19 years, and fuse to the spine at the age of 20 to 25 years. Failure of the anterior acromion ossification center to fuse to the spine gives rise to the os acromiale. This unfused apophysis is present in 2.7% of random patients and is bilateral in 60% of cases.
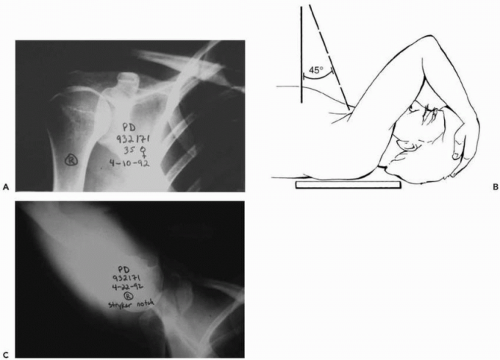
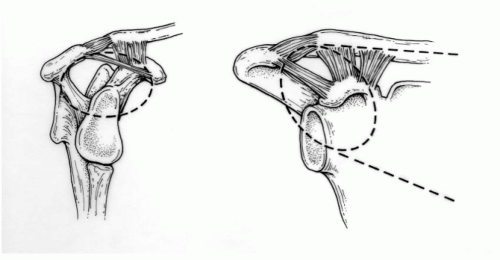
57 The size of the os acromiale depends on which of the four ossification centers of the acromion have failed to fuse (
Fig. 18-3). The most common site of nonunion is between the meso-acromion and the meta-acromion, which corresponds to the midacromioclavicular joint level. An axillary lateral radiograph clearly demonstrates the lesion. Norris has reported that the os acromiale has been mistaken for fracture and that there is an association between the os acromiale and a rotator cuff tear.
78The inferior angle of the scapula arises from an ossification center that appears at age 15 years and fuses with the remainder of the scapula at age 20 years. The vertebral border
arises from an ossification center that appears at age 16 to 18 years and fuses by the age of 25 years.
The glenoid fossa ossifies from four sources: (a) the coracoid base (including the upper third of the glenoid), (b) the deep portion of the coracoid process, (c) the body, and (d) the lower pole, which joins with the remainder of the body of the scapula at age 20 to 25 years.
Caution must be exercised when interpreting radiographs of the scapula in adolescents and young adults. The os acromiale is the most frequently quoted unfused apophysis and can be confused with fracture.
57,
78 In addition, the physes at the base of the coracoid and the tip of the coracoid process can be difficult to distinguish from fracture. In the appropriate setting, a radiograph of the contralateral scapula is useful in determining whether a radiographic “line” is truly a fracture or an unfused apophysis. Furthermore, the junction between the upper and lower glenoid in adults represents the coalescence of the previous ossification centers and is the site of origin of many glenoid fossa fractures with a transverse component.
Biomechanics
The scapula is suspended from the clavicle through the acromial clavicular joint and coracoclavicular ligament. The clavicle, in turn, joins the trunk at the sternoclavicular joint. The sternoclavicular joint is the only true joint attaching the upper extremity to the body. However, the scapula articulates with the posterior chest wall and spine through numerous muscular attachments. Although not a
synovial joint, the scapulothoracic articulation is a stable construct that is rarely disrupted.
16,
17,
45,
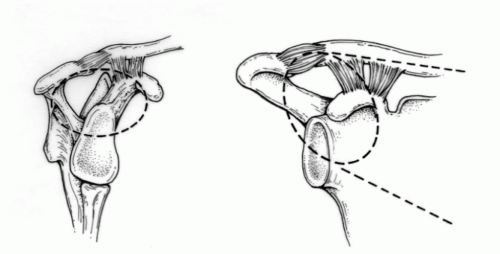
83The reliance of overhead activity on the relationships among the clavicle, coracoclavicular ligaments, acromioclavicular joint, acromion, and glenoid neck has led to the development of the concept of the superior shoulder suspensory complex (SSSC) by Goss.
32,
33 and
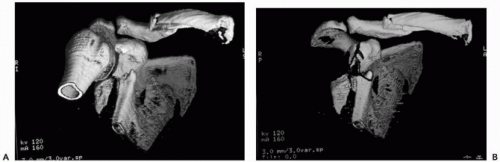
34 He likened the SSSC to a ring with two links. The ring is composed of the clavicle lateral to the coracoclavicular ligament, the coracoclavicular ligament itself, the glenoid, the coracoid process, and the acromion. The links are composed of the clavicle and the lateral scapular body and scapular spine (
Fig. 18-4). The SSSC is thought to provide stability for the shoulder complex. Moreover, disruption of two or more components of the SSSC may result in enough loss of stability of the shoulder complex to require operative fixation.
26,
32,
33 and
34,
40,
41 and
42,
60,
99Williams and colleagues
107 investigated the biomechanics of the SSSC in a cadaveric model, with particular reference to one specific type of double disruption of the SSSC—the “floating shoulder” (fracture of the glenoid neck and clavicular shaft). In their model, the coracoacromial ligament, which was not included in Goss’s original description of the SSSC, provided significant stability to the shoulder girdle. Complete lack of suspensory support of the shoulder did not occur as a result of ipsilateral clavicle and glenoid neck fractures without additional injuries to the coracoacromial and acromioclavicular ligaments. Williams et al. suggested that the coracoacromial ligament should be added to the SSSC (
Fig. 18-5).