CHAPTER 19 Proximal Tibial Osteotomy
High tibial osteotomy (HTO) is a surgical procedure used to change the mechanical weight-bearing axis and alter the loads carried through the knee. Conventional indications for HTO are medial compartment osteoarthritis and varus malalignment of the knee causing pain and dysfunction, but the indications for HTO have expanded with concomitant cartilage regeneration procedures and meniscal transplantation. Knee instability has been considered a contraindication; however, today the indications for HTO include patients with chronic ligament deficiencies and malalignment, because this procedure can change not only the coronal but also the sagittal plane of the knee, improving stability. In addition, despite good long-term results with total knee arthroplasty, there remains a significant concern regarding the longevity of these prostheses, particularly in younger patients. In contrast, osteotomy provides an alternative that preserves the knee joint, which, when appropriately performed, should not compromise later arthroplasty should this be necessary. The reported results of proximal tibial osteotomy vary considerably across the literature, but in general the procedure provides good relief of pain and restoration of function in approximately 80% to 90 % of patients at 5 years and 50% to 65 % at 10 years.1 Most authors who have analyzed these results have found that success is directly related to ideal patient selection and achieving optimal alignment.2 Accurate preoperative assessment and surgical technique are therefore essential to achieve a satisfactory outcome. This chapter will discuss the importance of alignment, clinic evaluation, radiographic assessment, indications and contraindications, techniques, and special situations regarding proximal tibial osteotomy.
ANATOMY
Importance of Alignment
The tibia has a coronal and sagittal plane, and it is mandatory to consider both in every situation. The normal anatomic axis (coronal plane) of the knee has a range from 5 to 7 degrees. In varus knees (malalignment in the coronal plane), degeneration of the articular cartilage tends to progress because of deviation of the mechanical axis.3 In the normal knee, the medial posterior tibial slope (sagittal plane) is usually 9 to 11 degrees and the lateral posterior tibial slope is generally 6 to 11 degrees; however, a wide range of values have been reported in various studies.4,5 The sagittal plane of the knee has often been ignored but its changes cause important modifications in the biomechanics of the knee and in joint stability. Decreased posterior tibial slope causes posterior tibia translation and helps the anterior cruciate ligament (ACL)–deficient knee. In contrast, increased tibial slope causes anterior tibial translation and helps the posterior cruciate ligament (PCL)–deficient knee. Some studies6,7 have demonstrated that the correction of the alignment is associated with the regeneration of articular cartilage that seemed apparently normal.
PATIENT EVALUATION
History and Physical Examination
A thorough clinical assessment requires a detailed history and physical examination. Specific analysis of this information will help determine whether a patient is likely to benefit from osteotomy. Important aspects of a patient’s general history include age, occupation, activity level, and medical and surgical history. Particularly significant are the expectations that the patient has for activity postoperatively. The patient may have noticed an increasing deformity or a static long-term malalignment. Pain history should focus on the site and severity, as well as aggravating and relieving factors. A history of locking, catching, or instability may indicate a mechanical source of symptoms, and the specific details of each of these symptoms should be sought to determine whether other procedures, such as arthroscopy, may be beneficial as an adjunct to osteotomy. Lower limb alignment should be assessed at each level, and the gait should be observed for any abnormalities, particularly a thrust in the direction of the deformity, indicating a significant dynamic component. Presence of deformity in all three planes should be assessed, particularly rotational deformity, because this is more difficult to assess later radiographically. Whether a deformity is fixed or correctable should be determined. The prresence of an effusion is determined and location of tenderness should be recorded carefully. Range of motion is measured, particularly looking for a flexion contracture and the amount of flexion comfortably achieved. Good mobility of the knee is a prerequisite, with no less then 110 degrees of flexion and no more than 10 degrees of extension loss. Patellar tracking and the presence of crepitus is to be noted, although the status of the patellofemoral joint is not determinate of indication. Ligaments are examined, including the ACL, AMC, PCL, medial cruciate ligament (MCL), and lateral cruciate ligament (LCL). Adjacent joints are examined and assessment of neurovascular function is essential.
Diagnostic Imaging
In 1992, Dugdale and colleagues8 proposed a flow chart for the radiologic evaluation of a patient with a varus of the knee, which was later modified by Noyes and associates.9 They stated that the patient should get stress x-rays if physical examination reveals any of the following: positive varus stress test, increased varus during thrust, increased tibial external rotation at 30 degrees of knee flexion, or varus recurvatum during standing or walking. If the x-rays are positive, the patient should get supine, full-length anteroposterior (AP) x-rays of both legs to evaluate the alignment. If the physical examination reveals none of these, the patient should get full-length double-stance AP x-rays of both legs. If a varus deformity is absent, they suggested that the patient undergo a soft tissue reconstruction; if this deformity is present, it is important to evaluate whether a lateral joint line opening is associated. If this is the case, the patient should get stress x-rays; if not the case, two methods to evaluate the amount of correction to perform during surgery could be used (see later). Since this study, many other reports have been published for radiographic evaluation of the alignment of the lower limb. We believe that the following imaging studies with (standard and stress x-rays) be obtained for these patients.
Standard X-Ray Evaluation
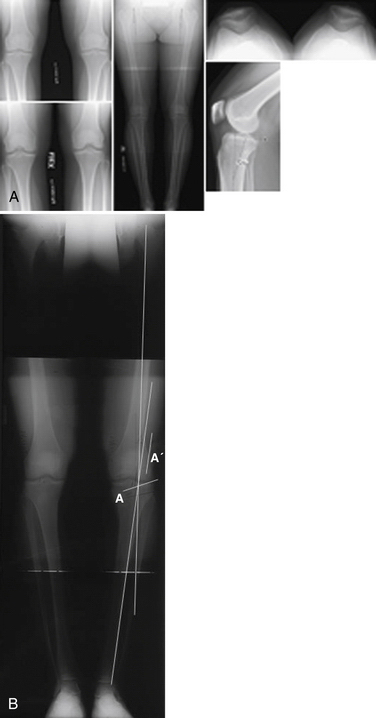
A full-length, double-stance AP x-ray is mandatory to evaluate femorotibial alignment (Fig. 19-1), as described by Moreland and coworkers.10 An AP x-ray is taken from the hips to the ankles with the patient standing and the patellae looking forward using a suitable cassette to filter the x-ray beam gradually for proper visualization of both hips and ankles.
Dugdale and colleagues8 have proposed two methods to quantify the amount of correction to perform if a malalignment is present. In both methods, a line along the tibial plateau and its intersection with the desired mechanical axis of the lower extremity is marked (in this chapter this point is called P for simplicity). A line is traced from the center of the femoral head to P and a line is traced from the center of the tibiotalar joint to P. In the first method, the angle formed at the intersection between these two lines represents the amount of correction required. In the second method, the radiographic film is cut along the osteotomy line and along a vertical line that converges with the first. Leaving a 2-mm hinge at the medial tibial margin, the distal part of the film is rotated until the femoral head, P, and the tibiotalar joint are along the same line. The overlapping wedge margin is the amount of correction to perform. It was also demonstrated that if lateral and/or posterolateral soft tissue structures are insufficient, for every increase of 1 mm in the lateral joint line width, there is 1 degree of added varus. Supine X-rays are important to eliminate the added varus because of the deficiency of the lateral and/or posterolateral structures and to evaluate the actual amount of correction to perform. It was also shown that after HTO, the mechanical axis of the lower extremity is translated laterally—3 to 4 mm for each degree of valgus correction—and this value depends on the height of the patient. We essentially use the same technique as described earlier to estimate the correction required.
The bilateral long-leg standing view is used (see Fig. 19-1B) to calculate the desired location of the new mechanical axis. If the two intersection lines are drawn from the center of the hip and from the center of the ankle, through the lateral tibial spine or 62% of the joint, bringing these two lines together will create the new mechanical axis. The osteotomy is drawn (line A) and measured and transposed to the two intersecting lines (line A′); the amount of opening measured at that point is the amount of correction required.
A lateral x-ray view is used to evaluate posterior tibial slope. A number of methods have been reported to quantify its value. Dejour and Bonnin4 have recommended tracing a line along the proximal tibial anatomic axis (PTAA) and a line along the tibial plateau; the angle between these two lines is tibial slope. Moore and Harvey,11 in 1974, described the tibial plateau angle. They recommended tracing a line along the anterior tibial cortex (ATC) and a line along the medial tibial plateau; the angle between these two lines is tibial slope.
Brazier and associates5 have proposed three other methods:
They compared these three techniques and stated that the most reliable are the PTAA and PTC methods.
Cullù and coworkers12 have compared the various methods and found higher values for the same patients using the method described by Moore and Harvey11 and lower values with the PFAA method.5 We recommend using the line along the articular surface of the medial tibial plateau and the anatomic axis (PTAA) for assessing the posterior slope, because it is simple and reproducible.
Stress X-Ray
The lateral stress view, according to the Telos method, was first described by Jacobsen in 1976.13 The patient lies in the lateral decubitus position with the knee flexed at 90 degrees and is encouraged to relax. The heel is fixed to a stand and the arm of the Telos GA II device (Telos; Weterstadt, Germany) applies a posterior force to the tibia. In this position, a lateral x-ray is taken. The test is then performed with the knee at 25 degrees of flexion.13 This method is important in chronic PCL-deficient knees to evaluate anterior and posterior tibial translation with regard to the femur. It is also useful to detect a fixed posterior tibial subluxation, as described by Strobel and colleagues14 in 2002; they found it to be present in 44% of patients with a PCL lesion.
The lateral stress view using the kneeling method15 also measures posterior subluxation. The patient kneels on a bench with the knee in 90 degreesof flexion; the bench supports the lower legs only up to the tibial tubercle. A lateral x-ray is taken.
In addition, a lateral stress view with hamstring contraction was described by Chassaing and associates16 in 1995. The patient lies in the lateral decubitus or seated position, with the knee at 90 degrees of flexion and the heel fixed to a stand. A lateral x-ray is taken while the patient contracts the hamstring for at least 10 seconds.17
Finally, a lateral stress view is obtained according to the gravity method described by Stäubli and Jakob in 1990.18 The patient lies in the supine position with the hip and the knee at 90 degrees of flexion, supported by an assistant, with the leg in neutral rotation. In this position, a lateral x-ray is taken.
The axial stress view described by Puddu and coworkers19 in 2000. The patient lies in the supine position, with both knees at 70 degrees of flexion, the feet plantigrade in moderate plantar flexion, and the tibia in neutral rotation. The x-ray beam is directed parallel to the longitudinal patellar axis from distal to proximal and the distance between the anterior tibial profile and the center of the femoral groove is measured. The side to side difference is the amount of posterior instability.
Jung and colleagues, in 2006,17 compared these five methods, focusing on posterior translation, side to side difference, condylar rotation, time to perform the test, and pain during the test. Considering all these factors, they stated that the most effective methods are with the Telos device at 90 degrees of knee flexion and the kneeling method, even if they are painful and time-consuming procedures. The Telos procedure is the most expensive but the most reliable for detecting a posterior tibial subluxation.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is useful to evaluate the meniscal, articular cartilage, and soft tissue (ligamentous) status of the knee. In addition, with compartment overload, there may be subchondral edema, indicating the need for unloading that compartment. Traumatic subchondral bone lesions20 can easily be detected.
TREATMENT
Indications And Contraindications
Proper patient selection is fundamental for satisfactory postoperative results. In general, having the knee joint in good condition will result in a more predictable outcome. Naudie and associates1 have concluded that younger patients who have excellent knee range of motion (ROM), higher functional demand, and a lower grade of osteoarthritis (OA) will have better outcomes, and that the survival of the HTO will be much longer than in more advanced knees.
Indications
 Varus knee with associated medial cartilage defects (i.e., osteochondritis dissecans, osteonecrosis)
Varus knee with associated medial cartilage defects (i.e., osteochondritis dissecans, osteonecrosis) Varus knee with associated instability (ACL, PCL, PLC) and evidence of medial compartment overload or lateral or posterolateral thrust
Varus knee with associated instability (ACL, PCL, PLC) and evidence of medial compartment overload or lateral or posterolateral thrust