This article reviews the literature regarding the outcomes of various nonoperative and operative treatment options for osteonecrosis of the hip. This article provides the orthopedic community with the latest evidence regarding the suitability of currently available treatment modalities in various stages of the disease.
Key points
- •
A multitude of medical treatment options have been described for the treatment of early stage osteonecrosis.
- •
Mesenchymal stem cell–based therapies with conventional methods of treatment have shown early promise in the treatment of the precollapse stage of osteonecrosis.
- •
Prospective randomized multicenter trials comparing pharmacotherapy with core decompression and stem cell–based therapies are needed in future.
- •
Cementless total hip arthroplasty with highly cross-linked polyethylene and new generation of ceramic bearings have shown excellent results at short-term to midterm follow-up.
Introduction
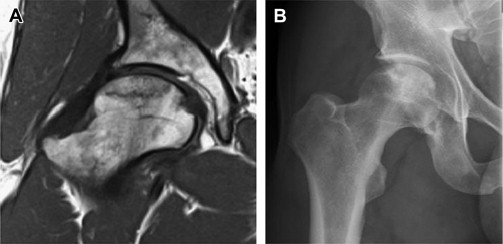
Osteonecrosis (ON) of the hip, with its varied causes and poorly understood pathogenesis, is an incapacitating disease primarily affecting the active population in the third and fourth decades of life. Management of ON has continued to remain a dilemma despite improvements in both medical and surgical treatment of this disease. The goal of management is to diagnose ON early in the precollapse stage and prevent subsequent progression to collapse and end-stage arthritis ( Fig. 1 ). Treatment has typically been based on the staging of ON ( Table 1 ); however, various other factors, such as the extent of the lesion, location, and causes, are often also taken into account when planning treatment. Although numerous studies reporting on a variety of operative and nonoperative methods have been published in the literature, there has been no consensus with regard to the ideal treatment of the precollapse stage of these lesions. Moreover, encouraging clinical outcomes following recent advances in short stem designs, porous biomaterials for cementless fixation, and ceramic or highly cross-linked polyethylene bearings have led to debate about the optimal implant for hip arthroplasty in patients with end-stage ON. This article presents a review of the current evidence regarding the outcomes of various nonoperative and operative treatment options for ON.
| Ficat and Arlet | University of Pennsylvania | ARCO | Japanese Orthopedic Association | ||||
|---|---|---|---|---|---|---|---|
| Stage | Findings | Stage | Findings | Stage | Findings | Stage | Findings |
| I | Normal radiograph | 0 | Normal hip | 0 | Normal hip | 1 | Demarcation line |
| II a | Diffuse cystic/sclerotic lesions | I | MRI findings only | 1 | MRI findings only | 2 | Early femoral head flattening |
| II b | Crescent sign (subchondral fracture) | II | Diffuse cystic/sclerotic lesions | 2 | Focal osteoporosis, cystic lesions, sclerosis | 3 | Cystic lesions |
| III | Presence of sequestrum in radiograph; femoral head collapse | III | Subchondral step-off | 3 | Crescent sign (subchondral fracture) | — | — |
| IV | Loss of articular cartilage and osteoarthritis with a deformed femoral head | IV | Femoral head flattening | 4 | Acetabular involvement | — | — |
| — | — | V | Acetabular involvement or joint space narrowing | — | — | — | — |
| — | — | VI | Advanced joint degeneration | — | — | — | — |
Nonoperative treatment
A variety of pharmacologic and biophysical treatments have recently been suggested for prevention of disease progression following ON. These treatment modalities have been proposed to favorably affect various points in the purported etiopathogenic pathway of ON. The goal of medical treatment in the precollapse stage is to improve function and provide pain relief, prevent radiographic progression to subchondral fracture and collapse, and allow healing of the necrotic lesions. The following nonsurgical modalities have shown promise in the treatment of the precollapse stage of ON.
Non–Weight Bearing
Although non–weight bearing has been proposed as a treatment option for early stage ON (stage I and II, Ficat and Arlet), Mont and colleagues, in a meta-analysis of 819 patients, reported poor clinical outcomes in more than 80% of the patients at a mean follow-up of 34 months (range, 1.6–10 years) following nonoperative treatment. No difference in outcomes was seen between full, partial, and non–weight-bearing regimens in their study. In a recent systematic review with level II evidence the same author reported that 59% (394 of 664 hips) of asymptomatic hips had onset of symptoms or progressed to collapse at a mean follow-up of 7 years (range, 0.2–20 years). The investigators also reported that the incidence of progression to collapse was highest in patients who had sickle cell disease (73%; 29 of 40 hips) in contrast with patients who had systemic lupus erythematosus, who had the lowest rate of progression to collapse at 17% (10 of 59 hips). One-hundred and forty-nine hips (32%) with small or medium-sized lesions (<50% of head involvement) progressed to symptoms or collapse, whereas large lesions (>50%) had an 84% rate of progression.
Bisphosphonates
Progression of early stage ON to subchondral fracture and collapse is known to be related to the increased osteoclastic bone resorption around the necrotic region, which occurs as a result of the physiologic healing process. Bisphosphonates reduce osteoclastic activity and inhibit bone turnover, and have been proposed in the treatment of early stage ON. The improvement in bone mineral density in the femoral head following their long-term use may thus prevent, or at least delay, the development of collapse.
Agarwala and colleagues, in their report of 395 hips at a mean follow-up of 4 years (range, 1–8 years), reported a radiographic progression to collapse in 12.6% (27 of 215 hips) in stage I and 55.8% (72 of 129 hips) in stage II (Ficat and Arlet staging) following treatment with alendronate 10 mg daily for 3 years. The mean time to collapse was 3.5 years (range, 3–6 years) in stage I and 2.9 years (range, 2–5 years) in stage II hips. The same author in a recent publication of 53 hips at 10-year follow-up reported a 29% collapse rate in the precollapse stage of ON (10 of 34 hips) following 3 years of continuous alendronate use at 70 mg weekly. The investigators thus concluded that the natural history of untreated ON with more than 70% collapse rate was favorably altered with alendronate use.
Lai and colleagues, in a prospective randomized study of 54 hips in Steinberg stage II and III ON, reported a significant decrease in the rate of radiographic progression to collapse in patients treated with 70 mg of alendronate (2 of 29 hips) weekly for 1 year compared with the placebo group (19 of 25 hips; P <.001) at 2-year (range, 2–2.3 years) follow-up. Moreover, 14% (4 of 29 hips) of patients in the treatment of group had radiographic progression of 1 stage or more during the observation period compared with 80% (20 of 25 hips) in the placebo group.
However, Chen and colleagues reported conflicting evidence in a recent prospective, randomized, double-blinded, placebo-controlled trial (level I evidence) with 65 hips in stage IIC and IIIC (University of Pennsylvania classification). They reported no significant difference in radiographic disease progression, quality-of-life improvement, and prevention of total hip arthroplasty between the alendronate and the placebo cohorts at the final follow-up at 2 years. However, the investigators thought that the study was underpowered to detect statistical significance despite a numerical reduction in the rate of disease progression (61% vs 66%) and total hip arthroplasty conversion (12.5% vs 15.2%) in the alendronate group.
Anticoagulants
Hypofibrinolysis and thrombophilia leading to venous outflow obstruction and increased intraosseous pressure have been reported by various researchers to be a pathogenic factor in the development of ON. Thus, conceptually systemic anticoagulation may delay or may even reverse the process of ischemic ON by preventing clot propagation and enhancing clot lysis. Glueck and colleagues, in a prospective study of 25 patients (35 hips) with known thrombophilia and Ficat stage I or II ON of the hip, reported that 95% of hips (19 of 20 hips) with primary ON and 20% (3 of 15 hips) of patients with secondary ON (secondary to corticosteroid use) had no progression of disease at a minimum follow-up of 2 years (mean, 3 years; range, 2–4 years) following enoxaparin therapy (60 mg/d for 3 months).
Hypolipidemics
Corticosteroids have been reported in multiple studies to be associated with the development of ON. These pharmacologic agents induce differentiation of pluripotent marrow stem cells into the adipocyte lineage by stimulating expression of adipocyte-specific genes 422(aP2) and PPARγ2 while decreasing expression of Cbfa1/Runx2 and osteocalcin promoter, which normally promotes differentiation into an osteocyte lineage. In addition, corticosteroids increase angiogenic sensitivity to vasospastic agents like endothelin-1 and decrease response of blood vessels to vasodilators such as bradykinin. Statins have been reported to counteract this abnormal adipocyte differentiation by promoting osteoblastic differentiation and may prevent the development of corticosteroid-induced ON.
In a retrospective analysis of 284 patients receiving high-dose corticosteroids, Pritchett reported that 3 patients (1%) developed ON following statin treatment at a mean follow-up of 7.5 years (range, 5–11 years). However, Ajmal and colleagues reported that statin therapy did not significantly reduce the risk of ON in their series of 338 renal transplant patients receiving high-dose corticosteroids at a mean follow-up of 7.5 years compared with patients who did not receive statins (range, 3.5–19 years; P = .8).
Extracorporeal Shock Wave Therapy
Incidental finding of increased pelvic bone mineral density seen after extracorporeal shock wave therapy for renal stones stimulated interest in its use in orthopedics. Although the mechanism through which extracorporeal shock wave therapy exerts its beneficial effects in ON is currently unknown, it seems that extracorporeal shock wave therapy causes stimulation of neovascularization through increased expression of angiogenic growth factors. Ludwig and colleagues, in a prospective study of 21 patients, reported improvement in pain, mobility, and Harris hip scores in 66.6% (14 patients) at 1-year final follow-up. Follow-up magnetic resonance imaging (MRI) revealed either a decrease in size of the necrotic regions (6 patients) or healing of the lesions (4 patients), whereas the area of poor circulation remained unchanged in the remaining 4 patients.
Wang and colleagues, in a randomized trial of 57 hips at a mean follow-up of 2 years (range, 2–3.3 years) comparing extracorporeal shock wave therapy with bone grafting, reported significant improvement in pain and Harris hip scores, and decreased need for total hip arthroplasty in the extracorporeal shock wave therapy group ( P <.001). Seventy-nine percent of patients improved (≥50% reduction in hip pain and ≥50% improvement in hip function), whereas 20% remained unchanged or became worse following extracorporeal shock wave therapy. In the bone grafting cohort, 29% of patients improved, whereas 72% deteriorated or remained unchanged. More recently, the same investigators in a long-term follow-up study (mean, 8.5 years; range, 7.7–8.8 years) of these 57 hips reported that patients with extracorporeal shock wave therapy had significantly better clinical outcomes (76% vs 21% good or fair; P <.001) and decreased need for total hip arthroplasty (24% vs 64%; P = .002) compared with the bone grafting cohort.
Hsu and colleagues, in a prospective randomized study of 98 hips comparing extracorporeal shock wave therapy and a cocktail regimen of extracorporeal shock wave therapy, hyperbaric oxygen, and alendronate, reported similar improvement in clinical outcomes in both cohorts at mean 2-year follow-up (range, 1.5–4 years). The size of the lesion either remained unchanged or improved in 90% of patients in both groups at final follow-up. Wang and colleagues, in a randomized trial of 55 hips with stage I to III ON (Association Research Circulation Osseous classification) reported no significant difference in the pain control ( P = .4), hip function ( P = .1), and the need for total hip arthroplasty ( P = .8) with extracorporeal shock wave therapy (6000 impulses at 28 kV at each session) in patients with systemic lupus erythematosus (SLE) and a non-SLE control group at minimum of 2 years’ follow-up.
Pulsed Electromagnetic Therapy
Pulsed electromagnetic therapy is thought to favorably affect early stage ON through stimulation of osteogenesis and angiogenesis similar to extracorporeal shock wave therapy. Massari and colleagues, in their retrospective analysis of 76 hips treated with electromagnetic field stimulation in Ficat stage I to III, reported that the 94% of hips in stage I and II avoided the need for total hip arthroplasty with a significantly higher proportion of hips in stage III progressing to total hip arthroplasty at a mean follow-up of 2 years. At present, evidence in favor of electromagnetic stimulation is limited and further research is needed to explore its potential role in early stage ON.
Hyperbaric Oxygen
Hyperbaric oxygen therapy, by increasing extracellular oxygen concentration, reduces cellular ischemia, and is also known to reduce edema by inducing vasoconstriction. Reis and colleagues reported radiographic improvement in 81% of their patients (n = 25) with Steinberg stage I ON following 100 days of daily hyperbaric oxygen therapy. Camporesi and colleagues also reported improvement in pain and range-of-motion at final follow-up of 7 years in a study of 19 patients randomized to receive 30 treatment doses of either hyperbaric oxygen or hyperbaric air for a total period of 6 weeks. None of the patients in the hyperbaric oxygen group required total hip arthroplasty for disease progression at the time of final follow-up.
Vasodilators
Vasodilators from prostacyclin I2 derivatives (eg, iloprost) are known to improve blood flow in the terminal vessels and until recently their potential efficacy was only defined in the treatment of vasospastic conditions like vasculitis, pulmonary hypertension, SLE, Raynaud phenomenon, and sickle cell crisis.
Based on promising early evidence that iloprost may have a role in bone regeneration at the cellular level, Jager and colleagues conducted a prospective study on 50 patients (98 joints) to explore the analgesic and curative potential of iloprost in the treatment of bone marrow edema (BME) and early stage ON. They reported significant improvement in pain, quality of life, Knee Society scores and Harris hip scores, and radiographic decrease (56% showing complete disappearance of BME) in the extent of BME in bones with Association Research Circulation Osseous (ARCO) stage I and II following a 5-day infusion protocol of intravenous iloprost at 6 months’ follow-up. However, no improvement was seen in the advanced stages of ON despite showing an analgesic effect in some patients. Disch and colleagues also reported significant improvement in pain, hip function, and BME in 33 patients (n = 16 with BME and n = 17 with ON) at mean 2 years’ (range, 1–3 years) follow-up. At present, randomized controlled trials and further long-term data are needed before prostacyclin analogues can be recommended for routine use in early stage ON.
Introduction
Osteonecrosis (ON) of the hip, with its varied causes and poorly understood pathogenesis, is an incapacitating disease primarily affecting the active population in the third and fourth decades of life. Management of ON has continued to remain a dilemma despite improvements in both medical and surgical treatment of this disease. The goal of management is to diagnose ON early in the precollapse stage and prevent subsequent progression to collapse and end-stage arthritis ( Fig. 1 ). Treatment has typically been based on the staging of ON ( Table 1 ); however, various other factors, such as the extent of the lesion, location, and causes, are often also taken into account when planning treatment. Although numerous studies reporting on a variety of operative and nonoperative methods have been published in the literature, there has been no consensus with regard to the ideal treatment of the precollapse stage of these lesions. Moreover, encouraging clinical outcomes following recent advances in short stem designs, porous biomaterials for cementless fixation, and ceramic or highly cross-linked polyethylene bearings have led to debate about the optimal implant for hip arthroplasty in patients with end-stage ON. This article presents a review of the current evidence regarding the outcomes of various nonoperative and operative treatment options for ON.

| Ficat and Arlet | University of Pennsylvania | ARCO | Japanese Orthopedic Association | ||||
|---|---|---|---|---|---|---|---|
| Stage | Findings | Stage | Findings | Stage | Findings | Stage | Findings |
| I | Normal radiograph | 0 | Normal hip | 0 | Normal hip | 1 | Demarcation line |
| II a | Diffuse cystic/sclerotic lesions | I | MRI findings only | 1 | MRI findings only | 2 | Early femoral head flattening |
| II b | Crescent sign (subchondral fracture) | II | Diffuse cystic/sclerotic lesions | 2 | Focal osteoporosis, cystic lesions, sclerosis | 3 | Cystic lesions |
| III | Presence of sequestrum in radiograph; femoral head collapse | III | Subchondral step-off | 3 | Crescent sign (subchondral fracture) | — | — |
| IV | Loss of articular cartilage and osteoarthritis with a deformed femoral head | IV | Femoral head flattening | 4 | Acetabular involvement | — | — |
| — | — | V | Acetabular involvement or joint space narrowing | — | — | — | — |
| — | — | VI | Advanced joint degeneration | — | — | — | — |
Nonoperative treatment
A variety of pharmacologic and biophysical treatments have recently been suggested for prevention of disease progression following ON. These treatment modalities have been proposed to favorably affect various points in the purported etiopathogenic pathway of ON. The goal of medical treatment in the precollapse stage is to improve function and provide pain relief, prevent radiographic progression to subchondral fracture and collapse, and allow healing of the necrotic lesions. The following nonsurgical modalities have shown promise in the treatment of the precollapse stage of ON.
Non–Weight Bearing
Although non–weight bearing has been proposed as a treatment option for early stage ON (stage I and II, Ficat and Arlet), Mont and colleagues, in a meta-analysis of 819 patients, reported poor clinical outcomes in more than 80% of the patients at a mean follow-up of 34 months (range, 1.6–10 years) following nonoperative treatment. No difference in outcomes was seen between full, partial, and non–weight-bearing regimens in their study. In a recent systematic review with level II evidence the same author reported that 59% (394 of 664 hips) of asymptomatic hips had onset of symptoms or progressed to collapse at a mean follow-up of 7 years (range, 0.2–20 years). The investigators also reported that the incidence of progression to collapse was highest in patients who had sickle cell disease (73%; 29 of 40 hips) in contrast with patients who had systemic lupus erythematosus, who had the lowest rate of progression to collapse at 17% (10 of 59 hips). One-hundred and forty-nine hips (32%) with small or medium-sized lesions (<50% of head involvement) progressed to symptoms or collapse, whereas large lesions (>50%) had an 84% rate of progression.
Bisphosphonates
Progression of early stage ON to subchondral fracture and collapse is known to be related to the increased osteoclastic bone resorption around the necrotic region, which occurs as a result of the physiologic healing process. Bisphosphonates reduce osteoclastic activity and inhibit bone turnover, and have been proposed in the treatment of early stage ON. The improvement in bone mineral density in the femoral head following their long-term use may thus prevent, or at least delay, the development of collapse.
Agarwala and colleagues, in their report of 395 hips at a mean follow-up of 4 years (range, 1–8 years), reported a radiographic progression to collapse in 12.6% (27 of 215 hips) in stage I and 55.8% (72 of 129 hips) in stage II (Ficat and Arlet staging) following treatment with alendronate 10 mg daily for 3 years. The mean time to collapse was 3.5 years (range, 3–6 years) in stage I and 2.9 years (range, 2–5 years) in stage II hips. The same author in a recent publication of 53 hips at 10-year follow-up reported a 29% collapse rate in the precollapse stage of ON (10 of 34 hips) following 3 years of continuous alendronate use at 70 mg weekly. The investigators thus concluded that the natural history of untreated ON with more than 70% collapse rate was favorably altered with alendronate use.
Lai and colleagues, in a prospective randomized study of 54 hips in Steinberg stage II and III ON, reported a significant decrease in the rate of radiographic progression to collapse in patients treated with 70 mg of alendronate (2 of 29 hips) weekly for 1 year compared with the placebo group (19 of 25 hips; P <.001) at 2-year (range, 2–2.3 years) follow-up. Moreover, 14% (4 of 29 hips) of patients in the treatment of group had radiographic progression of 1 stage or more during the observation period compared with 80% (20 of 25 hips) in the placebo group.
However, Chen and colleagues reported conflicting evidence in a recent prospective, randomized, double-blinded, placebo-controlled trial (level I evidence) with 65 hips in stage IIC and IIIC (University of Pennsylvania classification). They reported no significant difference in radiographic disease progression, quality-of-life improvement, and prevention of total hip arthroplasty between the alendronate and the placebo cohorts at the final follow-up at 2 years. However, the investigators thought that the study was underpowered to detect statistical significance despite a numerical reduction in the rate of disease progression (61% vs 66%) and total hip arthroplasty conversion (12.5% vs 15.2%) in the alendronate group.
Anticoagulants
Hypofibrinolysis and thrombophilia leading to venous outflow obstruction and increased intraosseous pressure have been reported by various researchers to be a pathogenic factor in the development of ON. Thus, conceptually systemic anticoagulation may delay or may even reverse the process of ischemic ON by preventing clot propagation and enhancing clot lysis. Glueck and colleagues, in a prospective study of 25 patients (35 hips) with known thrombophilia and Ficat stage I or II ON of the hip, reported that 95% of hips (19 of 20 hips) with primary ON and 20% (3 of 15 hips) of patients with secondary ON (secondary to corticosteroid use) had no progression of disease at a minimum follow-up of 2 years (mean, 3 years; range, 2–4 years) following enoxaparin therapy (60 mg/d for 3 months).
Hypolipidemics
Corticosteroids have been reported in multiple studies to be associated with the development of ON. These pharmacologic agents induce differentiation of pluripotent marrow stem cells into the adipocyte lineage by stimulating expression of adipocyte-specific genes 422(aP2) and PPARγ2 while decreasing expression of Cbfa1/Runx2 and osteocalcin promoter, which normally promotes differentiation into an osteocyte lineage. In addition, corticosteroids increase angiogenic sensitivity to vasospastic agents like endothelin-1 and decrease response of blood vessels to vasodilators such as bradykinin. Statins have been reported to counteract this abnormal adipocyte differentiation by promoting osteoblastic differentiation and may prevent the development of corticosteroid-induced ON.
In a retrospective analysis of 284 patients receiving high-dose corticosteroids, Pritchett reported that 3 patients (1%) developed ON following statin treatment at a mean follow-up of 7.5 years (range, 5–11 years). However, Ajmal and colleagues reported that statin therapy did not significantly reduce the risk of ON in their series of 338 renal transplant patients receiving high-dose corticosteroids at a mean follow-up of 7.5 years compared with patients who did not receive statins (range, 3.5–19 years; P = .8).
Extracorporeal Shock Wave Therapy
Incidental finding of increased pelvic bone mineral density seen after extracorporeal shock wave therapy for renal stones stimulated interest in its use in orthopedics. Although the mechanism through which extracorporeal shock wave therapy exerts its beneficial effects in ON is currently unknown, it seems that extracorporeal shock wave therapy causes stimulation of neovascularization through increased expression of angiogenic growth factors. Ludwig and colleagues, in a prospective study of 21 patients, reported improvement in pain, mobility, and Harris hip scores in 66.6% (14 patients) at 1-year final follow-up. Follow-up magnetic resonance imaging (MRI) revealed either a decrease in size of the necrotic regions (6 patients) or healing of the lesions (4 patients), whereas the area of poor circulation remained unchanged in the remaining 4 patients.
Wang and colleagues, in a randomized trial of 57 hips at a mean follow-up of 2 years (range, 2–3.3 years) comparing extracorporeal shock wave therapy with bone grafting, reported significant improvement in pain and Harris hip scores, and decreased need for total hip arthroplasty in the extracorporeal shock wave therapy group ( P <.001). Seventy-nine percent of patients improved (≥50% reduction in hip pain and ≥50% improvement in hip function), whereas 20% remained unchanged or became worse following extracorporeal shock wave therapy. In the bone grafting cohort, 29% of patients improved, whereas 72% deteriorated or remained unchanged. More recently, the same investigators in a long-term follow-up study (mean, 8.5 years; range, 7.7–8.8 years) of these 57 hips reported that patients with extracorporeal shock wave therapy had significantly better clinical outcomes (76% vs 21% good or fair; P <.001) and decreased need for total hip arthroplasty (24% vs 64%; P = .002) compared with the bone grafting cohort.
Hsu and colleagues, in a prospective randomized study of 98 hips comparing extracorporeal shock wave therapy and a cocktail regimen of extracorporeal shock wave therapy, hyperbaric oxygen, and alendronate, reported similar improvement in clinical outcomes in both cohorts at mean 2-year follow-up (range, 1.5–4 years). The size of the lesion either remained unchanged or improved in 90% of patients in both groups at final follow-up. Wang and colleagues, in a randomized trial of 55 hips with stage I to III ON (Association Research Circulation Osseous classification) reported no significant difference in the pain control ( P = .4), hip function ( P = .1), and the need for total hip arthroplasty ( P = .8) with extracorporeal shock wave therapy (6000 impulses at 28 kV at each session) in patients with systemic lupus erythematosus (SLE) and a non-SLE control group at minimum of 2 years’ follow-up.
Pulsed Electromagnetic Therapy
Pulsed electromagnetic therapy is thought to favorably affect early stage ON through stimulation of osteogenesis and angiogenesis similar to extracorporeal shock wave therapy. Massari and colleagues, in their retrospective analysis of 76 hips treated with electromagnetic field stimulation in Ficat stage I to III, reported that the 94% of hips in stage I and II avoided the need for total hip arthroplasty with a significantly higher proportion of hips in stage III progressing to total hip arthroplasty at a mean follow-up of 2 years. At present, evidence in favor of electromagnetic stimulation is limited and further research is needed to explore its potential role in early stage ON.
Hyperbaric Oxygen
Hyperbaric oxygen therapy, by increasing extracellular oxygen concentration, reduces cellular ischemia, and is also known to reduce edema by inducing vasoconstriction. Reis and colleagues reported radiographic improvement in 81% of their patients (n = 25) with Steinberg stage I ON following 100 days of daily hyperbaric oxygen therapy. Camporesi and colleagues also reported improvement in pain and range-of-motion at final follow-up of 7 years in a study of 19 patients randomized to receive 30 treatment doses of either hyperbaric oxygen or hyperbaric air for a total period of 6 weeks. None of the patients in the hyperbaric oxygen group required total hip arthroplasty for disease progression at the time of final follow-up.
Vasodilators
Vasodilators from prostacyclin I2 derivatives (eg, iloprost) are known to improve blood flow in the terminal vessels and until recently their potential efficacy was only defined in the treatment of vasospastic conditions like vasculitis, pulmonary hypertension, SLE, Raynaud phenomenon, and sickle cell crisis.
Based on promising early evidence that iloprost may have a role in bone regeneration at the cellular level, Jager and colleagues conducted a prospective study on 50 patients (98 joints) to explore the analgesic and curative potential of iloprost in the treatment of bone marrow edema (BME) and early stage ON. They reported significant improvement in pain, quality of life, Knee Society scores and Harris hip scores, and radiographic decrease (56% showing complete disappearance of BME) in the extent of BME in bones with Association Research Circulation Osseous (ARCO) stage I and II following a 5-day infusion protocol of intravenous iloprost at 6 months’ follow-up. However, no improvement was seen in the advanced stages of ON despite showing an analgesic effect in some patients. Disch and colleagues also reported significant improvement in pain, hip function, and BME in 33 patients (n = 16 with BME and n = 17 with ON) at mean 2 years’ (range, 1–3 years) follow-up. At present, randomized controlled trials and further long-term data are needed before prostacyclin analogues can be recommended for routine use in early stage ON.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





