Magnetic Resonance Neurography 
Magnetic resonance neurography (aka MR neurography or MRN) is a modified version of current MR imaging techniques, which depicts peripheral nerves with greater conspicuity and in multiple different planes using a combination of high resolution and high contrast two-dimensional (2D) and three-dimensional (3D) imaging techniques. It is being increasingly employed in the diagnostic algorithm of peripheral neuropathy patients for the evaluation of nerve injury, entrapment, inflammation, and mass lesions. Since MRN provides sub -0.5 mm resolution on 2D imaging sequences and sub -1.5 mm resolution on 3D imaging sequences, the regional musculotendinous and joint structures are well seen on these sequences. Generally MRN is primarily performed for neurogenic symptoms, however, non-specific clinical symptoms suggesting sensory neuropathy or non-specific pain symptoms at times are better explained by the findings of regional joint derangement or inflammatory/autoimmune myopathy while the regional nerves might show normal appearance. Therefore, the reader should pay due diligence in the evaluation of various structural abnormalities in the field of view, and employ a structured reporting template to elegantly and accurately describe all the relevant abnormalities that may have the potential to guide patient’s treatment and management. This chapter discusses the imaging evaluation approach and describes how to fill the structured checklists in Boxes 1–3. These three checklists are relevant to the evaluation of brachial plexus, lumbosacral (LS) plexus, and generic MRN that could be used for any particular extremity areas. The generic MRN template can be used in isolation for a specific site, for example, carpal tunnel, tarsal tunnel, forearm neurography, etc; or if additional extremity site was performed as part of the plexus examination, for example, one would use brachial plexus and generic template for reporting of MRN examination of brachial plexus and right arm. Conceptual details of related MR physics and imaging protocol are discussed in the MR protocol optimization chapter.
 IMAGE EVALUATION
IMAGE EVALUATION
Similar to any other MR examination, a systematic approach to image evaluation is essential. The reader should try to glean relevant information from any available clinical findings or electrophysiology results to better evaluate and interpret the imaging findings. The below-outlined stepwise interpretation approach is only a practical guide, and all regional soft tissue structures should be evaluated in multiple planes for their optimal assessment. This will also help the readers perceive which structures are best depicted/evaluated on which particular plane.
1. During extremity neurography evaluation, first assess the long axis 2D and 3D images for gross bone or soft tissue injury or any mass lesion. Then, evaluate the muscles for any regional denervation changes. It is important to use good and uniform fat-suppression techniques to detect subtle edema-like signal changes in the denervated or myopathic muscles. This can be followed by assessment of regional joints for effusion, ganglion cyst, gross ligament injuries, labral and meniscal tears. Then, line up the similar-plane axial fat-saturated (fs) fluid sensitive and non-fs T1W images and synchronize them for tandem evaluation (Fig. 1). Diligently interrogate the regional muscles and nerves for signal intensity alterations, course, caliber, fascicles, and perineural fat planes. If there is an incidental finding of a mass lesion, further define its perineural extent, intraneural extension and fascicular involvement, etc. (Fig. 2). Compare the affected nerves to other regional nerves with regards to morphologic and signal alterations. Once a neural abnormality is detected, again look at the anatomically innervated downstream muscles for subtle denervation changes. Finally, in the light of available clinical findings, make a final impression of whether there is nerve injury (grade it), mass lesion (characterize it), entrapment (grade it), or polyneuropathy condition suggesting systemic or polyneuropathy causes, such as hereditary neuropathy, neurocutaneous syndrome, or inflammation.
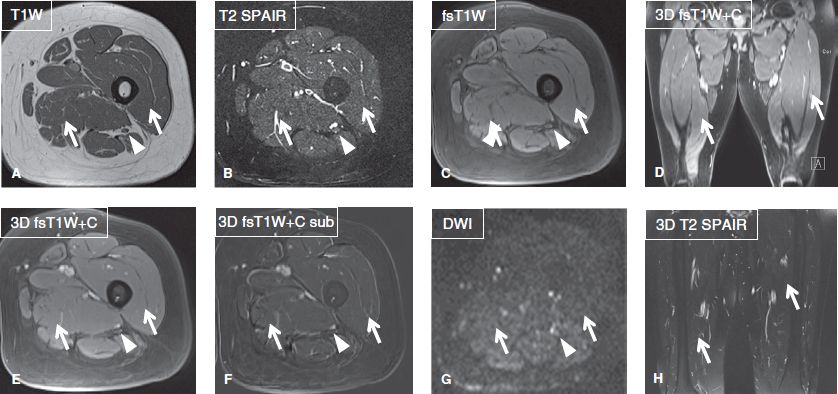
Fig. 1: Normal MRN appearance of peripheral nerves and skeletal muscles. Axial (A–C, E–G) and coronal (D, H) images demonstrate normal homogeneously intermediate signal intensity of skeletal muscles (short arrows) and sciatic nerves (arrowheads). The muscles and nerves lack abnormal enhancement or diffusion abnormality.
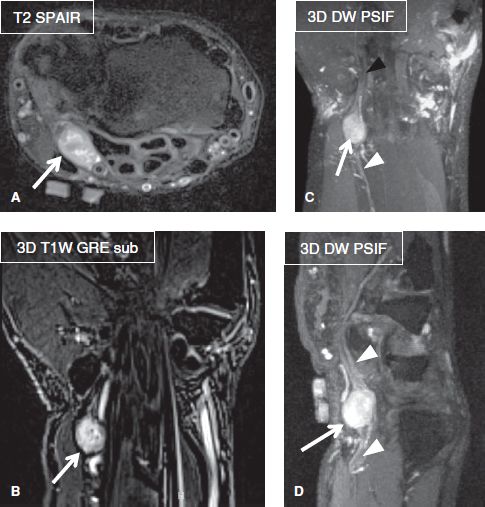
Fig. 2: Schwannoma of the ulnar nerve. Axial (A), coronal (B, C), and sagittal (D) images at the wrist exhibit a well-defined T2 hyperintense homogeneously enhancing mass (arrows), which features tail sign (arrowheads) and eccentric involvement of the ulnar nerve.
2. During the brachial or LS plexus evaluation, first look at the long axis 3D images for gross bony or soft tissue injury, or any mass lesion. Then, evaluate the muscles for gross regional denervation changes. This should be followed by systematic assessment of the spine (cervical or lumbar) and spinal cord, since spine pathology can be a major clinical confounder in the diagnosis of plexus pathology (Fig. 3). Look carefully for spinal cord or thecal sac impingement, cord edema or myelomalacia, severe neural foraminal stenosis, or other lesions that might explain patient symptoms or might contribute to downstream plexopathy or nerve entrapment (double crush syndrome). This should be followed by assessment of regional joints for effusion, ganglion cyst, gross ligament injuries or paralabral cysts suggesting labral tears. Then, line up the similar-plane axial fat-saturated (fs) fluid sensitive and non-fs T1W images during lumbar plexus evaluation and synchronize them for tandem evaluation. Diligently interrogate the regional muscles and nerves for alterations of signal intensity, course, caliber, fascicles, and perineural fat planes. If there is a regional mass lesion, further interrogate to define its extent, intraneural extension, fascicular involvement, etc. Compare the affected nerves to the regional nerves with regards to signal and morphologic alterations, since bilateral symmetry in the normal LS plexus and brachial plexus is quite remarkable (Fig. 4). Once a neural abnormality is detected, again look at the anatomically innervated downstream muscles for subtle denervation changes. During the brachial plexus evaluation, it is essential to evaluate sagittal inversion recovery images for side to side comparison with regards to signal and size alterations, as well as to distinguish among different segments of the brachial plexus (Fig. 5). Finally, in the light of the available clinical findings, make a final impression whether there is nerve injury (grade it), mass lesion (characterize it), entrapment (grade it), or one of the systemic/polyneuropathy condition, such as hereditary neuropathy, neurocutaneous syndrome, or inflammation.
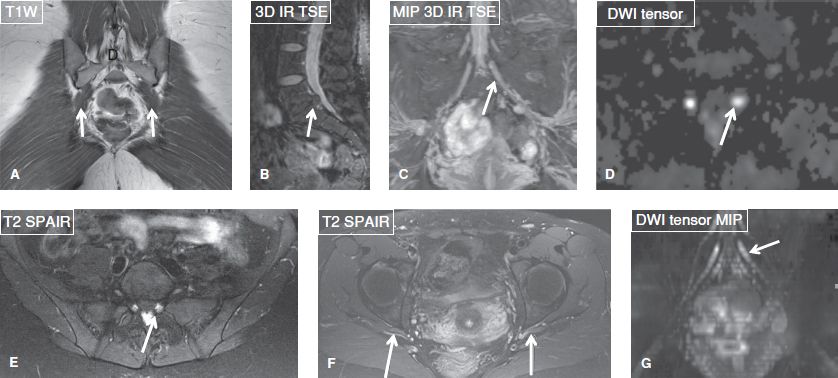
Fig. 3: Spine disease with left sciatica. A: Coronal image through pelvis shows normal symmetric piriformis muscles bilaterally (arrows). B: 3D sagittal reconstructed image shows disc herniation at L5–S1 level (arrow). C: 3D coronal MIP reconstructed image shows enlarged left S1 nerve (arrow). D, E: Axial images also confirm the abnormality. F: Axial image shows symmetrical appearance of the sciatic nerves (arrows) excluding pathology due to piriformis syndrome. G: MIP reconstruction from diffusion tensor image shows the subtle nerve enlargement along the long axis.
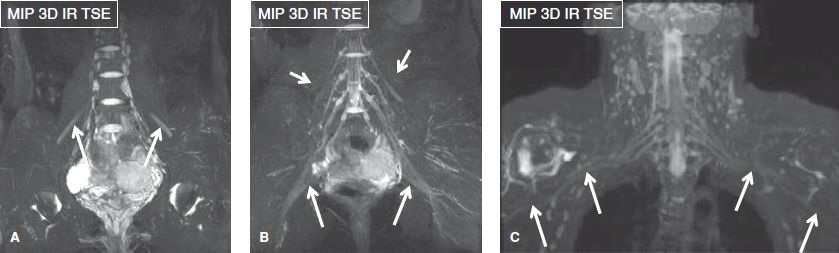
Fig. 4: Symmetrical versus asymmetrical plexus appearance. Coronal images (A, B) of the LS plexus show normal femoral nerves (arrows in A), sciatic nerves (long arrows in B), and the lateral femoral cutaneous nerves (short arrows in B). Coronal image (C) of the brachial plexus in a patient with a recent motor vehicle accident and associated ipsilateral humeral head fracture demonstrates asymmetric T2 hyperintensity of the right brachial plexus cords and peripheral branches (arrows), reflecting traction (Sunderland grade I–II) injury.
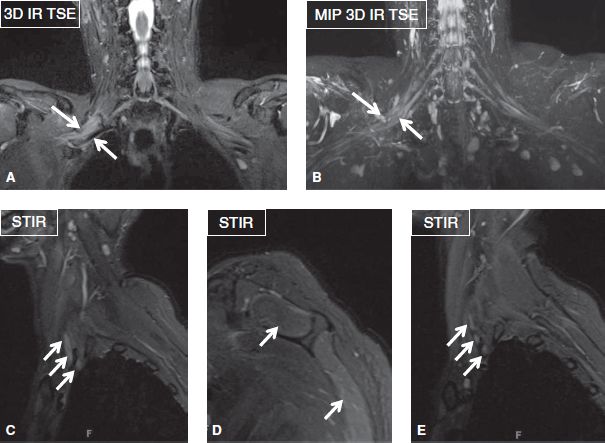
Fig. 5: Importance of sagittal images during brachial plexus evaluation. Brachial plexus iatrogenic stretch injury (Sunderland grade II/III injury). Coronal (A, B) and sagittal (C, D) images demonstrate asymmetric hyperintensity and thickening of the right brachial plexus (arrows) with predominant involvement of the upper and middle trunks, as well as edema of the ipsilateral infraspinatus muscle (asterisk). Notice normal trunks on the left side (arrows in E).
 BOX 1: The Structured Report: MRN of the Brachial Plexus
BOX 1: The Structured Report: MRN of the Brachial Plexus
The checklist for structured reporting of MR neurography of the brachial plexus. For each field, Normal is considered default in the dictation, whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendices 1 and 2 at the end of the chapter for a sample completed report.
Examination: MR Neurography of Brachial Plexus
FINDINGS:
Nerves:
Spinal cord: [<Normal> <Cord compression> <Cord edema> <Cord hemorrhage><Myelomalacia>]
Brachial plexus: Preganglionic: [<Normal> <Nerve root avulsion> <Pseudomeningocele>]
Brachial plexus: Postganglionic: [<Normal> <Thickening> <Asymmetrical or abnormal hyperintensity> <Laceration or rupture> <Nodularity> <Mass lesion>] of [<Nerve roots> <Trunks> <Divisions> <Cords> <Proximal peripheral nerves>]
Muscles/Tendons:
Scalenes: [<Normal> <Asymmetrical hypertrophy or Atrophy>]
Rotator cuff muscles: [<Normal> <Edema like signal> <Fatty replacement> <Atrophy>]
Other muscles: [<Normal> <Paraspinal muscles> <Trapezius> <Latissimus dorsi><Serratus anterior>]
Bones:
Cervical ribs: [<Absent> <Present> <Pseudoarthrosis with first rib>]
C7 transverse processes: [<Normal> <Elongated>]
Marrow signal: [<Normal> <Bone contusion or fracture> <Hemangioma> <Mass lesion>]
Joints:
Cervical spine:
Alignment: [<Normal> <Straightening> <Exaggerated lordosis> <Listhesis>]
Spinal Canal: Developmental stenosis: [<Absent> <Present in lower cervical spine or diffusely short pedicles>]
Occipital-C1 and atlantoaxial (C1–C2) articulations: [<Normal> <Osteoarthritis> <Effusion> <Atlantodental bursitis> <Pannus>]
C2–C3:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge> <Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge> <Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
C3–C4:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge> <Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge> <Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
C4–C5:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
C5–C6:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
C6–C7:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
C7–T1:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
Sternoclavicular joints: [<Normal> <Osteoarthritis> <Effusion>]
Acromioclavicular joints: [<Normal> <Osteoarthritis> <Effusion>]
Glenohumeral joints: [<Normal> <Osteoarthritis> <Effusion>]
Thoracic outlet/Cervicothoracobrachial junction/Spaces:
Interscalene triangle: [<Normal> <Narrowed> <Mass>]
Costoclavicular space: [<Normal> <Narrowed> <Mass>]
Retropectoralis minor space: [<Normal> <Narrowed> <Mass>]
Vessels:
[<Within normal limits> <Vascular kinking> <vascular thrombosis> <vascular malformation>]
Masses:
[<None>]
Other:
[<None> <Incidental posterior fossa brain findings> <Cervical lymphadenopathy><Thyroid mass> <Prevertebral edema>]
Postgadolinium discussion: [<No abnormal enhancement>]
Impression
1. [<>]
 BOX 2: The Structured Report: MRN of the Lumbosacral Plexus
BOX 2: The Structured Report: MRN of the Lumbosacral Plexus
The checklist for structured reporting of MR neurography of the lumbosacral plexus. For each field, Normal is considered default in the dictation, whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendices 3 and 4 at the end of the chapter for a sample completed report.
Examination: MR Neurography of Lumbosacral Plexus
FINDINGS:
Nerves:
Lower cord and conus: [<Normal> <Low lying or tethered cord> <Cord edema or compression> <Thickening or clumping of cauda equina>]
Lumbosacral plexus:
 Size: [<Normal> <Enlarged> <Atrophic>]
Size: [<Normal> <Enlarged> <Atrophic>]
 Signal: [<Normal> <Asymmetrically or abnormally hyperintense> < Asymmetrically or abnormally hypointense>]
Signal: [<Normal> <Asymmetrically or abnormally hyperintense> < Asymmetrically or abnormally hypointense>]
 Course: [<Normal> <Deviated> <Impinged>]
Course: [<Normal> <Deviated> <Impinged>]
Sciatic nerve:
 Size: [<Normal> <Enlarged> <Atrophic> <Mass>]
Size: [<Normal> <Enlarged> <Atrophic> <Mass>]
 Signal: [<Normal> <Asymmetrically or abnormally hyperintense> <Hypointense>]
Signal: [<Normal> <Asymmetrically or abnormally hyperintense> <Hypointense>]
 Course: [<Normal> <Variant intramuscular course> <Deviated> <Impinged>]
Course: [<Normal> <Variant intramuscular course> <Deviated> <Impinged>]
 Fascicles: [<Normal> <Asymmetrically enlarged or atrophic> <Effaced>]
Fascicles: [<Normal> <Asymmetrically enlarged or atrophic> <Effaced>]
Femoral and obturator nerves:
 Size: [<Normal> <Enlarged> <Atrophic> <Mass>]
Size: [<Normal> <Enlarged> <Atrophic> <Mass>]
 Signal: [<Normal> <Asymmetrically or abnormally hyperintense> <Hypointense>]
Signal: [<Normal> <Asymmetrically or abnormally hyperintense> <Hypointense>]
 Course: [<Normal> <Variant intramuscular course> <Deviated> <Impinged>]
Course: [<Normal> <Variant intramuscular course> <Deviated> <Impinged>]
 Fascicles: [<Normal> <Asymmetrically enlarged or atrophic> <Effaced>]
Fascicles: [<Normal> <Asymmetrically enlarged or atrophic> <Effaced>]
Lateral femoral cutaneous nerves:
 Size: [<Normal>]
Size: [<Normal>]
 Signal: [<Normal>]
Signal: [<Normal>]
 Course: [<Normal>]
Course: [<Normal>]
Other specific nerves in question: [<Pudendal/genitofemoral>]: [<Normal>]
Muscles/Tendons:
Psoas major:
 Bulk: [<Normal> <Atrophy> <Hypertrophy>]
Bulk: [<Normal> <Atrophy> <Hypertrophy>]
 Intramuscular signal: [<Normal> <Edema-like signal>]
Intramuscular signal: [<Normal> <Edema-like signal>]
 Iliopsoas bursa: [<Normal> <Mild/moderate/severe bursitis>]
Iliopsoas bursa: [<Normal> <Mild/moderate/severe bursitis>]
Piriformis:
 Bulk: [<Normal> <Atrophy> <Hypertrophy>]
Bulk: [<Normal> <Atrophy> <Hypertrophy>]
 Intramuscular signal: [<Normal> <Edema-like signal>]
Intramuscular signal: [<Normal> <Edema-like signal>]
 Iliopsoas bursa: [<Normal> <Mild/moderate/severe bursitis>]
Iliopsoas bursa: [<Normal> <Mild/moderate/severe bursitis>]
Gluteal:
 Bulk: [<Normal> <Atrophy> <Hypertrophy>]
Bulk: [<Normal> <Atrophy> <Hypertrophy>]
 Intramuscular signal: [<Normal> <Edema-like signal>]
Intramuscular signal: [<Normal> <Edema-like signal>]
 Trochanteric bursa: [<Normal> <Mild/moderate/severe bursitis>]
Trochanteric bursa: [<Normal> <Mild/moderate/severe bursitis>]
 Gluteal tendon: [<Normal> <Tendinosis> <Tear>]
Gluteal tendon: [<Normal> <Tendinosis> <Tear>]
Hamstring tendon: [<Normal> <Tendinosis> <Tear>]
Adductor: [<Normal> <Atrophy> <Edema-like signal> <Tear>]
Other: [<Quadriceps femoris> <Quadratus femoris/ischiofemoral impingement><Paraspinal muscles, edema-like signal, atrophy>]
Bones:
Sciatic notches: [<Normal> <Mass lesion>]
Marrow signal: [<Otherwise normal>]
Joints:
Lumbosacral spine: Alignment: [<Normal> <Straightening> <Exaggerated lordosis><Listhesis> <Transitional vertebra present>]
Spinal canal: Developmental stenosis [<Absent> <Present in lower lumbar spine or diffusely short pedicles>]
L1–L2:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
 Uncovertebral joints: [<Normal> <Hypertrophy>]
Uncovertebral joints: [<Normal> <Hypertrophy>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
L2–L3:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
L3–L4:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
L4–L5:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
L5–S1:
 Central canal: [<Patent> <Mild/moderate/severe narrowing>]
Central canal: [<Patent> <Mild/moderate/severe narrowing>]
 Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Neural foramina: Right: [<Normal> <Mild/moderate/severe narrowing>]
Left: [<Normal> <Mild/moderate/severe narrowing>]
 Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
Intervertebral disc: [<Normal> <Dessication> <Decreased height> <Bulge><Herniation> <Disc–osteophyte complex>]
 Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
Facet joints: [<Normal> <Mild/moderate/severe facet hypertrophy> <Synovial cyst>]
 Ligamentum flavum: [<Normal> <Hypertrophy>]
Ligamentum flavum: [<Normal> <Hypertrophy>]
Sacroiliac joints: [<Normal> <Osteoarthritis> <Effusion>]
Pubic symphysis: [<Normal> <Osteoarthritis> <Effusion>]
Hip joints: [<Normal> <Osteoarthritis> <Effusion> <Paralabral cyst>]
Vessels: [<Normal>]
Masses: [<None>]
Other (pelvic viscera): [<None> <Physiologic free fluid in pelvis> <Fibroid/prostate enlargement/adnexal mass/lymphadenopathy>]
Postgadolinium discussion: [<No abnormal enhancement>]
Impression
1. [<>]
 BOX 3: The Structured Report: MRN Generic (Extremity/Tunnel)
BOX 3: The Structured Report: MRN Generic (Extremity/Tunnel)
The checklist for structured reporting of MR neurography of the extremity or tunnel. For each field, Normal is considered default in the dictation, whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendices 5 and 6 at the end of the chapter for a sample of completed reports of the normal and abnormal examination results.
Examination: MR Neurography of Extremity/Carpal, Cubital, or Tarsal Tunnel
FINDINGS:
Nerves:
Size: [<Normal> <Enlarged> <Atrophic> <Mass>]
Signal: [<Normal> <Asymmetrically or abnormally hyperintense> <Asymmetrically or abnormally hypointense>]
Course: [<Normal> <Deviated> <Impinged> <Injured>]
Fascicles: [<Normal> <Asymmetrically enlarged or atrophic> <Effaced>]
Variant anatomy: [<Absent> <Present>]
Perineural fat: [<Normal> <Effaced>]
Muscles/Tendons: [<Normal > <Muscle atrophy or hypertrophy> <Edema-like signal> <Tendinosis> <Tear>]
Bones: [<Normal > <Contusion> <Fracture> <Mass>]
Joints: [<Normal > <Effusion> <Osteoarthritis> <Ligament sprains> <Parameniscal or paralabral cyst>]
Vascular: [<Normal > <Varicosity> <Vascular malformation>]
Masses: [<None> <Intraneural mass> <Extraneural mass> <Neuroma in continuity> <End bulb neuroma>]
Other: [<None> <Ganglion cyst> <Thickened fascia> <Perineural fibrosis>]
Postgadolinium discussion: [<No abnormal enhancement>]
Impression
1. [<>]
How to Fill the Structured Report
This chapter will be dedicated to MRN imaging interpretation as to how to report abnormalities of peripheral nerves and the regional muscles. The evaluation of specific joints has been discussed separately in different chapters in the book.
Nerves:
Size: [<Normal> <Enlarged> <Atrophic><Mass>]
Signal: [<Normal> <Asymmetrically orabnormally hyperintense> <Asymmetrically or abnormally hypointense>]
Course: [<Normal> <Deviated> <Impinged><Injured>]
Fascicles: [<Normal> <Asymmetricallyenlarged or atrophic> <Effaced>]
Variant anatomy: [<Absent> <Present>]
Perineural fat: [<Normal> <Effaced>]
Muscles/Tendons: [<Normal> <Muscle atrophy or hypertrophy> <Edema-like signal><Tendinosis> <Tear>]
Normal Peripheral Nerves
Peripheral nerves are most often part and parcel of neurovascular bundles, which makes it convenient to identify their location, but harder to distinguish them from the adjacent veins on conventional MR imaging due to the frequently present in-plane flow phenomenon and frequently encountered pulsation artifacts. The in-flow phenomenon renders the veins hyperintense on the fat-suppressed fluid sensitive images, similar in signal intensity to what the abnormal nerve would appear. Additionally, poor fat suppression can cause artifactual increase in the regional nerve signal intensity. Therefore, one should use optimal techniques to suppress these artifacts and diligently learn the neuromuscular anatomy before embarking upon the interpretation of these examinations. The technical details of extremity and plexus MRN have been discussed in detail in Chapter 2 of this book (Technical considerations). A normal nerve is made up of axons and various connective tissue sheaths in a well-organized architecture. The axons are covered by Schwann cells, endoneurial fluid, and a connective tissue layer, referred to as the endoneurium. The bundles of axons are clustered together in a fascicle, which is covered by another layer, called the perineurium. The latter forms the blood–nerve barrier and prevents the enhancement of a normal nerve on intravenous contrast examination. Multiple fascicles are arranged in another covering layer, called as the epineurium (Fig. 6). The outer epineurium covers the nerve and the internal epineurium contains the supporting fatty tissue and vascular supply to the nerve, called the vasa nervosa. On MRN, one can see the pencil thin hypointense epineurium and fascicles in most nerves larger than 3 mm. The fascicular bundles are uniformly arranged with symmetrical signal intensity and minimal intra-epineurial fat interspersed around them (Fig. 7). The nerves generally travel a straight course along the extremity and oblique course in the plexus without any abrupt focal deviations or kinks. The nerve caliber is nearly similar or smaller than the adjacent arteries with minimal variations as the nerve turns around the joints.
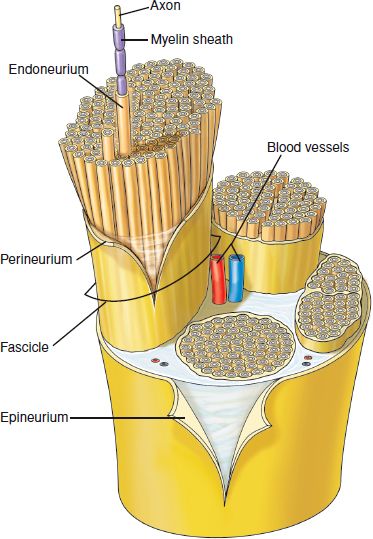
Fig. 6: Peripheral nerve showing axon, endoneurium, perineurium, and outer and inner epineurium.
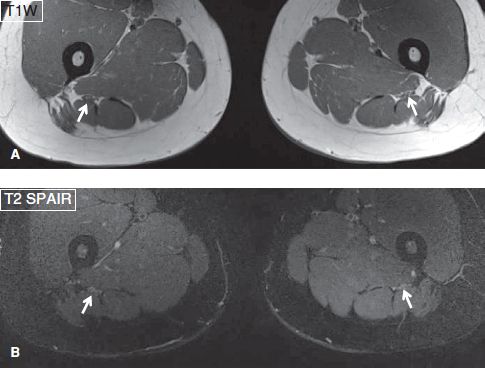
Fig. 7: Normal sciatic nerves. Axial images (A, B) through the thighs exhibit bilateral normal sciatic nerves (arrows), which appear isointense and mildly hyperintense to skeletal muscles on T1W and T2W images, respectively.
Nerve Imaging Abnormalities and Related Pitfalls in Interpretation
Nerve Enlargement and Enhancement
Any focal enlargement or distal diffuse caliber increase usually correlates with neuropathy (Fig. 8). It may represent a post-traumatic effect, intra-neural mass lesion, or a perineural mass lesion mimicking nerve enlargement. One should look carefully for displacement or involvement of the fascicles, which would then confirm intra-neural location of the mass lesion. If there is polyneuropathy condition manifested as multiple nerve abnormalities and/or diffuse nerve enlargement, consider hereditary cause (that would lead to symmetrical abnormalities), systemic causes, or autoimmune/inflammatory neuropathy (that commonly leads to patchy asymmetrical or, less commonly, symmetrical abnormalities) (Fig. 9). Contrast administration becomes essential, if there is no clear cut history of trauma or if the enlargement of nerve is away from the site of entrapment. Since normal nerves do not enhance, the enhancement characteristics may aid in diagnosis (e.g., heterogeneous enhancement in malignancy or degenerated schwannoma, patchy enhancement in amyloidosis and dense nodular enhancement in lymphoma, diffuse enhancement in radiation neuropathy, and no significant enhancement in subacute CIDP, post-traumatic neuroma or chemotherapy related toxic neuropathy) or suggest the potential site of activity, which could be biopsied to obtain the definitive diagnosis. If one finds nodular mass lesion(s) or nodular enhancement, consider other diagnostic possibilities, such as lymphoma, neurocutaneous syndrome, endometriosis, or amyloid (Fig. 10). Other patterns of enhancement include uniform fascicular enhancement and enlargement of perineurioma (honey comb pattern) (Fig. 11), lacework-type mild enhancement in fibrolipomatous hypertrophy of the nerve (Fig. 12), and targetoid enhancement of a peripheral nerve sheath tumor (PNST) (Fig. 13).
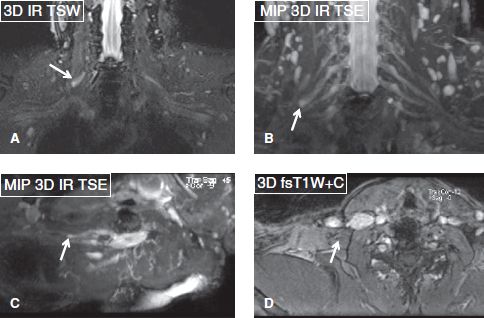
Fig. 8: Post-traumatic neuroma in continuity (Sunderland grade IV injury). Coronal (A, B) and oblique axial (C, D) images exhibit a neuroma in continuity of the right C6 nerve root (arrows) with no enhancement on contrast image (D).

Fig. 9: Polyneuropathy. Multifocal motor neuropathy. Axial image through the arm shows enlarged and abnormally hyperintense peripheral nerves. The median nerve is most affected (long arrow) as compared to the ulnar nerve (short arrow) and the radial nerve (arrowhead).
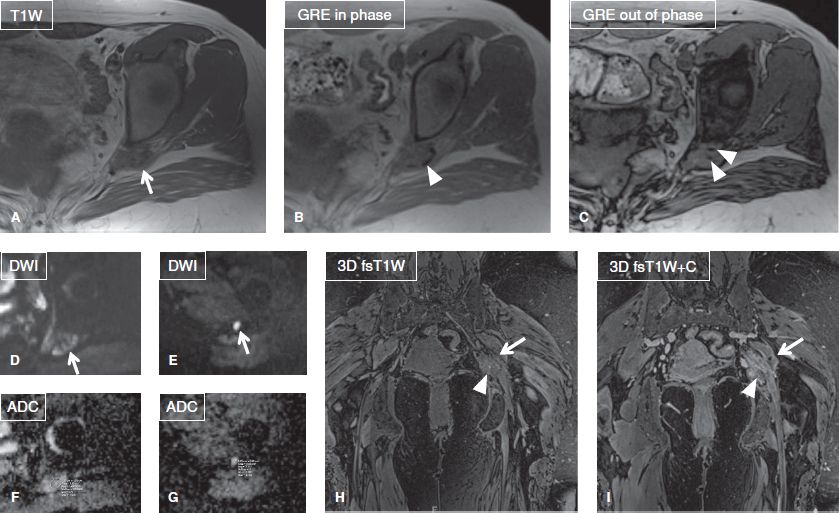
Fig. 10: Endometriosis causing sciatic neuropathy. Axial images (A–C) show a mass-like lesion (arrows) of intermediate T1/T2 signal at the left greater sciatic foramen, which features hypointense foci (arrowheads) on GRE images, indicative of blood products. ADC value of the lesion was 1.4 to 2 × 10−3 mm2/s (D–G). On the respective coronal images (H, I), the lesion (arrowheads) shows patchy contrast enhancement, indicative of hyperemia/inflammation. The findings are classic for sciatic endometriosis in a patient with symptoms of cyclical sciatica.
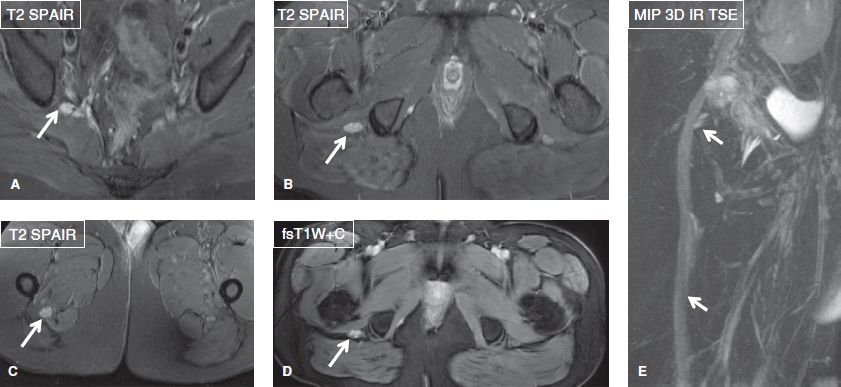
Fig. 11: Perineurioma of the sciatic nerve in a young woman. Axial (A–D) and oblique sagittal (E) images demonstrate diffuse thickening, abnormal T2 hyperintensity, uniform “honey comb” fascicular enlargement and intense enhancement of the right sciatic nerve (arrows).
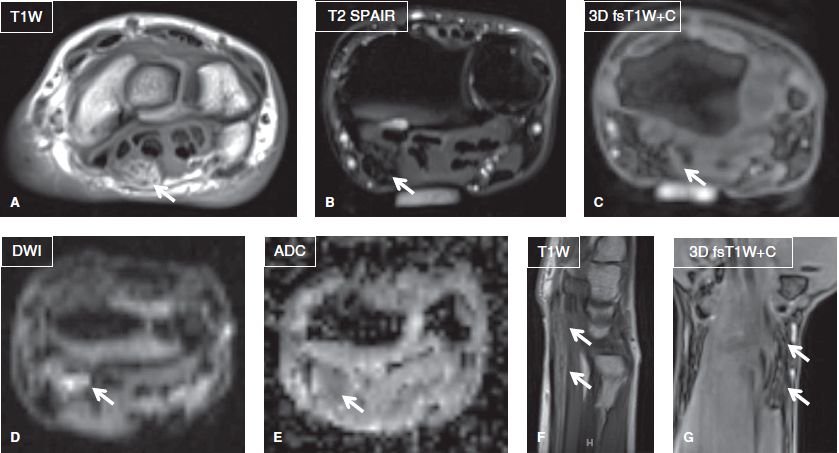
Fig. 12: Fibrolipomatous hamartoma of the median nerve. Axial (A–E), sagittal (F), and coronal (G) images exhibit diffuse enlargement of the median nerve (arrows), which contains fatty tissue, responsible for diffusion restriction. Notice “coxial cable” appearance on axial image (A) and “spaghetti appearance” on the long axis image (F).
Fig. 13: Neurofibroma. Coronal image shows a well-defined lesion (arrow) at the anatomic location of the right brachial plexus trunks, demonstrating targetoid contrast enhancement.
Nerve Signal
The nerve signal is usually isointense on non-fs T2W images while mild hyperintense signals might be normally observed due to good fat suppression on fat-saturated fluid sensitive images. The signal alteration is reflective of enhancement of the endoneurial fluid (Fig. 7). In addition, obliquely traversing nerves can be normally bright due to the magic angle artifact. However, this artifact occurs in expected location(s) along the fixed course of the peripheral nerves and in the plexus. For example, the femoral and sciatic nerves as well as all LS plexus nerves are symmetrically bright in the abdominopelvic region (Fig. 4), while these peripheral nerves outside the pelvis appear isointense to muscles when they have assumed relatively straight course in the extremities. Similar signal alteration may be seen for short segments in otherwise normal peripheral nerves, such as the ulnar nerve at the Guyon canal, medial plantar nerve at the tarsal tunnel, pudendal nerve at the entry into the lesser sciatic foramen, and lateral femoral cutaneous nerve (LFCN) at the iliac spine. Mild, moderate, and severe hyperintensity respectively refer to signal alterations of the nerve, higher than the skeletal muscle or adjacent nerves but considerably less than the regional in-plane venous signal, approaching the regional in-plane venous signal, and similar or higher than the venous signal (Figs. 14, 15). In the brachial or lumbar plexuses, the nerve roots appear uniformly bright, but symmetrical in signal and size bilaterally. To detect abnormal signal alteration, compare the signal intensity of the dorsal nerve root ganglion (DRG) to the nerve root distally. Normally, DRG is the most bright structure along the nerve (about two times the signal of the distal postganglionic segment of the nerve) and distally, the nerve signal gradually fades along its course. With neuropathy, the T2 signal of the postganglionic segment approaches the DRG (∼<1.5 times) or may exceed it sometimes, leading to inconspicuous appearance of the DRG. One should note that mild nerve signal alterations are not uncommon at the sites of everyday friction, for example, in median nerve at the carpal tunnel, ulnar nerve at the cubital tunnel, sciatic nerve at the sciatic notch, and C8, T1 nerves at the thoracic outlet. Such findings in isolation should be reported as non-specific nerve hyperintensity, to be correlated clinically for significance. The peripheral nerves become increasingly hyperintense with worsening severity of lesion(s); however, with chronicity of neuropathy, the nerves may become atrophic and lose the bright signal alteration. Other signal characteristics that help in further characterization of intraneural lesion include fat (lipoma, fibrolipomatous hypertrophy, chronic atrophic neuropathy, e.g., in diabetes mellitus), fibrosis (neuroma in continuity, Sunderland grade IV–VI injury as described below), hemorrhage (endometriosis, synovial sarcoma), calcification (Leprosy), and hyperintense pseudomass formation (hereditary demyelinating neuropathy, Charcot–Marie–Tooth disease—CMT type 1A) (Fig. 16).
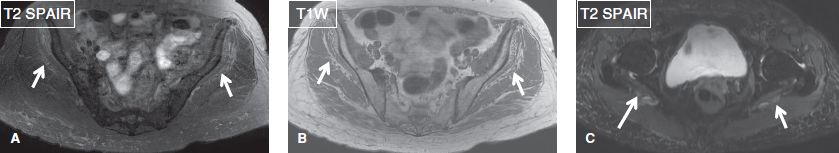
Fig. 14: Mild sciatic hyperintensity in a case of diabetic neuropathy. Gluteus minimus atrophy bilaterally and mild bilateral sciatic neuropathy. Axial images (A–C) show symmetric mild edema like signal (arrows in A) with fatty infiltration and atrophy (arrows in B) of the gluteus minimus muscles due to long standing diabetes. Mild T2 hyperintensity the sciatic nerves (arrows in C) are noted bilaterally in this case with recent symptoms of bilateral sciatica (left > right). Compare sciatic nerve signal to adjacent muscles and vessels.
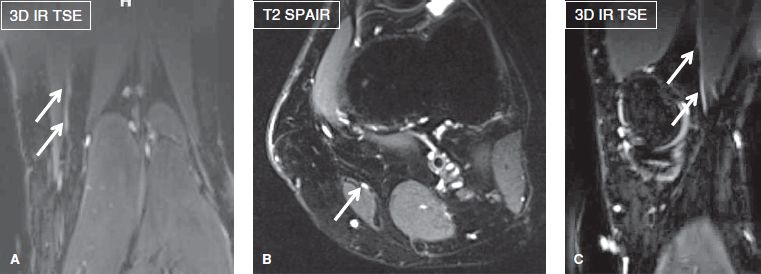
Fig. 15: Moderate nerve hyperintensity. Saphenous neuropathy. Coronal (A), axial (B), and oblique sagittal (C) images through the knee demonstrate a moderately hyperintense saphenous nerve (arrows). Compare nerve signal to the adjacent vessels.
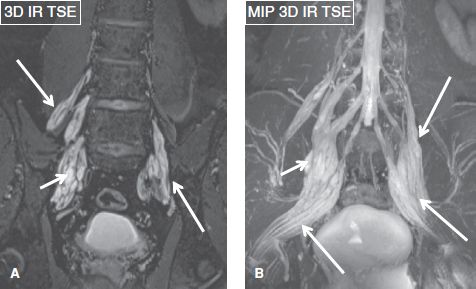
Fig. 16: CMT type 1A with pseudomass. Coronal images (A, B) show diffusely thickened lumbosacral plexus nerves (long arrows) and increased signal (the signal of the nerve exceeds the DRGs, making them inconspicuous) with interspersed pseudomasses (short arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







