The thumb-in-palm deformity is a fixed adduction-flexion posture in the affected hand of the patient with spastic cerebral palsy. This influences both hand function and hygiene.
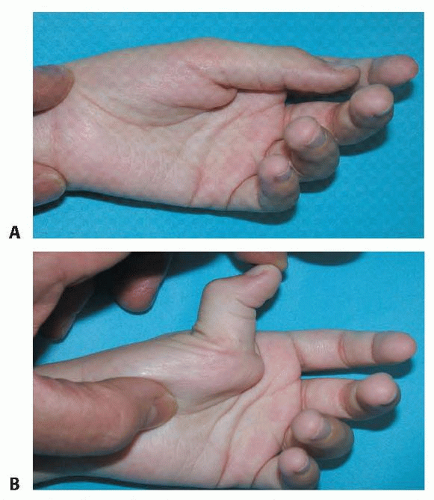
Imbalance of the spastic thumb flexor-adductor and the paretic thumb extensor results in thumb-in-palm deformity (FIG 1A).
The adductor pollicis (AP) is the most commonly involved muscle; the abductor pollicis brevis (APB) is usually not involved.17
The spastic AP, the first dorsal interosseous muscle, or both adduct the thumb and index metacarpals and cause first web space contracture.
If the flexor pollicis brevis (FPB) is spastic, the thumb metacarpophalangeal (MCP) joint will develop a flexion deformity.
Involvement of both the AP and FPB results in a thumb flexion and adduction posture with the thumb lying across the palm.
Involvement of the flexor pollicis longus (FPL) results in added thumb interphalangeal (IP) joint flexion (FIG 1B).
Weak thumb extensor and abductor pollicis longus (APL) may also contribute to the deformity.
Active function of the extensor pollicis longus (EPL) and extensor pollicis brevis (EPB) may result in hyperextension of the thumb MCP joint.
Cerebral palsy is permanent disorder of the development of movement and posture, causing activity limitation, attributed to a nonprogressive neurologic disturbance that occurred in the developing fetal or infant brain. The disorders of cerebral palsy are often accompanied by disturbances of sensation, perception, and cognition.11
The musculoskeletal findings develop secondarily. Spasticity initially results in shortening of the myotendinous unit and ultimately secondary contractures.
Paresis of muscles may contribute to greater deformity when spastic muscles are unopposed. The ultimate deformity depends on the overall imbalance.
A supple thumb-in-palm posture is a normal finding in infants during the first year. Persistence of a tightly closed thumb in palm longer than 1 year is abnormal and should be evaluated.3
The deformity is usually correctable at first and then progresses to a fixed deformity as myostatic contracture develops.
A progressive and variable-size discrepancy of the involved limb may develop, resulting in a smaller thumb.1
The lack of thumb extension and abduction can impair hand grip, function, appearance, and hygiene.
A complete history and physical examination of a child with cerebral palsy should be done carefully and thoroughly.
Input from other professionals such as neurologists and occupational therapists is often helpful.
Associated deformities of the spastic upper extremity such as finger and wrist flexion, forearm pronation, elbow flexion, and shoulder adduction and internal rotation should also be evaluated. Surgical treatment of thumb-in-palm deformity may be only one part of surgical care of the involved extremity.
Thumb muscle involvement, motion, and stability should be evaluated in the physical examination before organizing the treatment plan.
Individual muscle involvement is detected by observing thumb position and palpating spastic or contracted muscles (Table 1). As spasticity is rate-dependent tone, slow gradual stretch should be able to overcome this force, unlike a contracture which is a fixed shortening of a muscle tendon unit or joint.
Motion and stability are assessed by passive and active range of thumb abduction-adduction, flexion-extension, and palmar abduction and opposition.
Table 1 Grading of Thumb-in-Palm Deformity
Classification
Degree of Deformity
Illustration
House (1981)
Tonkin (2001)
Description
Simple deformity
Type I
Spastic or contracted AP, first dorsal interosseous muscle, or both
Intrinsic deformity

Type II
Type 1
Spastic or contracted AP, first dorsal interosseous, or both
Spastic or contracted FPB
Type III
Spastic or contracted AP, first dorsal interosseous, or both
Compensatory action of EPL and EPB to the unstable MCP joint
Absence of spastic FPL
Extrinsic deformity
Type 2
Spastic or contracted FPL Paretic EPL
Most severe: combined intrinsic and extrinsic deformity

Type IV
Type 3
Spastic or contracted AP, first dorsal interosseous, or both
Spastic or contracted FPB and FPL
AP, adductor pollicis longus; FPB, flexor pollicis brevis; EPL, extensor pollicis longus; EPB, extensor pollicis brevis; MCL, metacarpophalangeal; FPL, flexor pollicis longus.
The pattern of voluntary grasp and release of large objects and manipulation of small objects should be determined by observing the child during functional activities.
Sensory deficits impair function. Assessment of sensation should include stereognosis.
Repeated observation or videotaping of the child during various activities can also be useful for accurate evaluation. This can be particularly valuable in detecting dystonia.
Lower extremity function and need for intervention should be considered and coordinated appropriately.
Electrophysiologic testing and selective nerve blocks may help in localizing involved muscles and identifying muscles available for tendon transfers.
Select nerve blocks may help differentiate between spastic, spared, and fibrotic muscles.
Dynamic electromyography (EMG) with motion analysis may offer important information for planning tendon transfer surgery.5
Radiographs may reveal thumb joint instability or growth disturbance.
Clasped thumb
Distal arthrogryposis
Apparent absence of thumb extensor (faux extensor agenesis)
The goals of treatment need to be clearly defined.
No peripheral intervention will overcome the fundamental central nervous system etiology.
For many patients, the goal will be to improve thumb position for function; however, there is a subset of highly involved patients for whom improved hygiene alone may the goal.
Use of tone-reducing medication such as botulinum toxin to the AP can soften the deformities and improve joint range of motion for nonoperative management.4
In mild, nonrigid deformity, nonoperative treatment with orthoses may help in maintaining thumb abduction and improve hand function,13 but too-rigid splinting may result in limited thumb motion.
The principles of surgery for thumb-in-palm deformity are the following2:
Release of spastic muscles or contractures
Augmentation of paretic muscles
Stabilization of unstable thumb joints
Release of contracture with or without augmentation of weak muscles aims to rebalance the thumb muscles, depending on the pattern of motor dysfunction of the thumb and the patient’s degree of voluntary control.
Release of spastic muscle or myostatic contractures can be performed by intrinsic muscle release of the AP, FPB, APB, and first dorsal interosseous.
Extrinsic muscle release of the FPL may be considered if it is affected.
Secondary skin and fascial contracture of the first web space need to be addressed by four-flap or double-opposing Z-plasty.
Augmentation of paretic thumb abduction and extension can be accomplished by a combination of tenodesis and tendon rerouting or transfers and depends on the specific deficit, the muscles available, and the extent of voluntary control of selected muscles.
Thumb MCP joint arthrodesis or sesamoid capsulodesis should be considered for stabilizing the thumb MCP joints when the joint remains unstable.2
These joint stabilization procedures can also enhance tendon transfer procedures for extension-abduction.
Thumb MCP joint arthrodesis is considered when tendon transfer fails to correct the deformities or when sesamoid capsulodesis cannot control the hyperextension of the MCP joint.1
Thumb carpometacarpal (CMC) joint stabilization is indicated when metacarpal adduction cannot be controlled. CMC fusion, which preserves scaphotrapezial motion, is preferable to the rigid intermetacarpal fusion.2
Thumb IP joint fusion is usually not necessary, but this procedure may be indicated when the IP joint flexion contracture is severe or in the rare event of an FPL rupture after lengthening.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree