Acetabular Revision
Uncemented Hemispherical Components
Adolph V. Lombardi Jr. and Joseph J. Kavolus
Key Points
Introduction
Revision of the acetabular component of a total hip arthroplasty (THA) poses a unique set of challenges for the reconstructive surgeon. A full appreciation of the reason for the revision will assist in preoperative planning and execution of an appropriate acetabular reconstruction. Several reasons are known for revision of the acetabular component; they include polyethylene wear with or without osteolysis, aseptic loosening, mechanical failure, recurrent dislocation, acetabular component malposition, and septic loosening. The challenges of acetabular revision are related to loss of bone stock, alteration of the hip center of rotation, and the need to achieve stability of the prosthesis. The aims of revision are (1) to reconstitute acetabular deficits with the primary goal of re-creating the anatomy and biomechanics of the physiologic joint, and (2) to achieve stable fixation while taking special precautions to preserve bone in the event a repeat revision is required.
Over the past 30 years, a cementless hemispherical component has become the preferred system to employ for most acetabular revisions.1–3 Paramount to revision success is that the implant has initial stability to promote bone ingrowth and remodeling of the acetabulum to ensure long-term viability of the arthroplasty. Implant stability is directly related to the characteristics of the acetabular bone deficits, which, therefore, determine the specifics of the reconstruction process. A standard porous cementless hemispherical shell secured with multiple screws is the implant of choice but is feasible only with at least 50% host-bone contact. The utility of hemispherical shells is expanded by utilizing a jumbo cup with a slightly high hip center.4–9 The recent introduction of ultraporous metal surfaces with superior bone ingrowth capability has further increased the capabilities of cementless hemispherical acetabular revision.2,3,10-20
Indications
The driving tenet in the vast majority of arthroplasty procedures is that the physician should operate on the basis of the patient’s complaints, not the patient’s radiographs. However, in acetabular revision, this is not always the case. Patients presenting with polyethylene wear with or without osteolysis may have varying degrees of symptoms ranging from none to severe incapacitating pain. The physical examination may reveal a range from normal findings to significant limp and instability with recurrent dislocations. Radiographic evidence of polyethylene wear with significant osteolysis warrants acetabular revision even in the absence of clinical or functional symptoms. Some surgeons believe that even a marginal degree of osteolysis warrants revision because radiographs underestimate the degree of osteolysis.21–27 Computed tomography (CT) scan evaluation of patients has documented a far greater degree of osteolysis than can be evaluated utilizing standard radiographic techniques.21–27
Imaging studies can be combined with knowledge of the track record of specific devices. For example, a patient presenting with wear and osteolysis who has a liner of a type of polyethylene known to have a poor track record of wear should be considered for revision because this polyethylene liner is associated with significant wear and osteolysis.28 The debate in this specific group of patients involves whether a complete component revision is necessary, or whether isolated polyethylene exchange with retention of the acetabular component should be considered. The requisites for isolated polyethylene exchange alone include an acetabular component that is well-fixed, is in satisfactory position, has a satisfactory track record for component fixation, and has a satisfactory locking mechanism or adequate size to allow cementation of appropriate polyethylene into the device. Patients should be cautioned that this liner exchange does not imply that the procedure is simple or low risk. Instability following polyethylene liner exchange has been reported to be as high as 15% in patients who have undergone the surgical procedure via a posterior approach.29–31 The direct lateral approach has minimized this complication.32–34 In this specific patient population, complete acetabular revision should be considered and is the required course of action in the setting of damage to the locking mechanism or the actual component itself, which precludes the replacement of a new polyethylene liner or the cementation of an appropriate liner into the component, a malpositioned component, or a migrated or unstable component that fails stability testing during the operative intervention.
Symptomatic patients should undergo a complete history and physical examination. Patients presenting with acetabular component loosening will generally localize pain to the groin, buttock, and anterior medial thigh. Pain is generally associated with weight-bearing activities. Patients frequently describe classic start-up pain, which is severe, with the first few steps, followed by a diminution of the severity of pain as the patient ambulates. On physical examination, the patient will ambulate with a limp, noting pain in the groin. Pain is generally elicited with the patient supine performing a straight-leg raise and again localizing the pain to the groin. Radiographic evaluation generally reveals radiolucent lines at the component-bone interface. These may vary from radiolucencies limited to one or two of the DeLee and Charnley zones to radiolucencies involving all three zones.35 Radiolucencies in zones I and II are more indicative of loosening than is an isolated radiolucent line in zone III. Serial radiographs are always useful to determine the stability of an acetabular component with respect to cranial and medial migration. Further imaging studies that may prove useful are CT scans, which can critically evaluate the bone-prosthesis interface and can reveal the degree of osteolysis and osteopenia surrounding the acetabular component.
Increased utilization of alternate bearings in recent years has led to the introduction of several new indications for complete acetabular revision. In patients who have a ceramic-on-ceramic bearing, the incidence of squeaking has been reported to be anywhere from 0.2% to 21%.36–40 A variety of causes have been described. Several reports indicate that squeaking is component specific.36,41,42 Component malposition with associated impingement has been reported in several studies.40,43,44 The ensuing metal transfer from the impingement or from corrosion and modular junctions may lead to metal transfer, which appears to be a cause of significant squeaking.43,45,46 Although squeaking itself has not been shown to have any deleterious effects on the arthroplasty, if secondary to component malposition and impingement, the impingement may cause a stress riser on the femoral neck and ultimately fracture of the femoral neck.43 Additionally, squeaking has been the sole indication for acetabular component revision in patients whose lifestyle is affected by the squeaking itself.38,40,47
The resurgence of metal-on-metal total hip arthroplasty has brought not only the enhanced stability afforded by large-head reconstruction, but also concerns over adverse tissue reaction to metal debris.48,49 Two components have been withdrawn from the market50,51; therefore patients presenting with these components in place with any symptoms should be counseled on the possible need for acetabular revision. Symptomatic patients with metal-on-metal articulation may undergo serum metal ion screening. The Medicines and Healthcare products Regulatory Agency (MHRA) in the United Kingdom has recommended that all patients implanted with metal-on-metal devices should receive follow-up at least annually for 5 years, and more frequently if symptomatic.52 In addition, thorough investigation of symptomatic or at risk patients should include serum ion testing of cobalt and chromium levels, with a second test performed after a modest time interval in selected patients with elevated metal levels. Cross-sectional imaging studies including ultrasound or magnetic resonance imaging (MRI) should be performed, and revision considered if imaging reveals soft tissue reactions, fluid collections, or tissue masses.52 In light of a recent case report of cobalt toxicity in two patients who received metal-on-metal hip implants,53 the American Academy of Orthopaedic Surgeons has warned patients with metal-on-metal devices to inform their doctor or orthopedic surgeon of any new pain or increase in pain 3 months after hip replacement surgery.54 Patients can also be evaluated with a lymphocytic proliferation assay to determine reactivity to various metals.49,55
Patients presenting with acute instability with recurrent dislocation following primary hip arthroplasty should be evaluated carefully for component position. Appropriate anteroposterior (AP) and lateral radiographs maybe sufficient to determine the degree of abduction and anteversion. A CT scan may also be useful in patients with symptomatic metal-on-metal articulations. Late instability in patients who have metal-on-polyethylene articulations may be secondary to severe wear and shortening of the extremity with resultant capsular laxity. Patients may be treated with acetabular liner exchange.32–34 Leg length can be restored or enhanced with modular head/neck exchange,56,57 and the option for utilization of a larger head may be considered to enhance stability.58–60
It is imperative to rule out sepsis in all patients undergoing total hip revision arthroplasty. A careful history is important and may raise or lower the physician index of suspicion with respect to a septic process. Specifically, did the patient have any wound healing issues following the primary arthroplasty? Was the patient treated with antibiotics for wound erythema or extremity cellulitis? Are there any constitutional symptoms suggestive of infection, such as fever, chills, night sweats, etc.? Have there been any recent septic processes such as a dental abscess, upper respiratory infection, or urinary tract infection? Inflammatory markers consisting of a complete blood count (CBC) with differential, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) should be obtained on all patients. If these inflammatory markers are abnormal, hip aspiration should be performed, not only for culture and sensitivity, but also for cell count. Recent literature documents that a synovial fluid white blood cell count (WBC) greater than 2000/mL with more than 60% polymorphonuclear sites is indicative of infection.61,62 An indium WBC scan may be helpful in further delineating sepsis as the cause.63 Finally, at the time of surgical intervention, specimens can be sent for pathology testing, with a look at the number of white cells per high-power field. More than five cells per high-power field is suggestive of infection, and certainly more than 10 WBCs per high-power field is diagnostic of infection.64
Preoperative Planning
Paramount in planning is assessment of the severity and location of acetabular bone deficits. Managing these deficits during the reconstruction is one of the greatest challenges of hip revision. The primary aim of the surgical reconstruction is component stability. Integral to this fundamental requirement is comprehension of the current state of the acetabular bone stock. Preoperative planning starts with the basics: a comprehensive history and physical examination. Does the patient have a history of developmental dysplasia of the hip, Legg-Calvé-Perthes disease, or slipped capital femoral epiphysis? Were any nonarthroplasty surgical procedures performed, and when were they performed? The date of the primary hip arthroplasty and of any required subsequent procedures would be determined. Were there any perioperative complications? Did the primary procedure proceed without difficulty? Were there any concerns regarding the surgical site? Was the patient allowed to fully weight-bear following the procedure? If the patient was limited to protective weight bearing, for how long, and what was offered as an explanation for protected weight bearing? How long did the patient use assistive devices? How quickly did the patient feel that he or she resumed normal gait? Has the patient had any episodes of subluxation or actual dislocation? Has the patient experienced any grinding, clicking, squeaking, or other audible symptoms? The nature, location, and onset of pain should be explored.
Physical examination commences with the assessment of gait. Is the gait normal, antalgic, or Trendelenburg? Is the pelvis level, or is there pelvic obliquity secondary to a leg length discrepancy or spinal deformity? Leg length discrepancy can be assessed with the patient standing, by placing blocks of various thicknesses under the shorter extremity until the pelvis is deemed level. Alternatively, leg length can be evaluated with the patient in the supine position. A straight-leg raise test with the patient supine may elicit pain in the groin or buttock if the acetabular component is loose. Range of motion should be assessed. Patients who are experiencing anterior dislocation may have apprehension with full extension and external rotation; those who are experiencing posterior subluxation/dislocation may have significant apprehension with flexion, internal rotation, and adduction of the hip.
Radiographic evaluation should commence with a standard AP radiograph (Fig. 90-1). The intersection of the transischial line with the proximal femur is useful in determining leg length. Assessment of the Ranawat triangle is useful in determining whether the center of rotation has been restored.65,66 Furthermore, an evaluation of the acetabular component with respect to Kohler’s line is useful in detecting restoration of the center of the head. The abduction angle can be clearly determined on the AP radiograph. Concentric circles can be used to evaluate the degree of polyethylene wear. The AP pelvis is also carefully evaluated for any evidence of osteolysis, and the presence or absence of radiolucent lines in the zones of DeLee and Charnley is noted. If available, evaluation of serial radiographs is helpful in determining whether any cranial or medial migration of the acetabular component has occurred. A lateral radiograph should be evaluated for appropriate anteversion of the acetabular component (Fig. 90-2). If further detail is required, a CT scan with three-dimensional reconstructions can be acquired to determine component position, as well as degree of osteolysis, which is often underestimated by plain radiographs (Fig. 90-3).67–69

Figure 90-1 Anteroposterior (AP) radiograph of the pelvis of a 69-year-old female patient demonstrates bilateral total hip arthroplasty with acetabular findings of the right hip significant for bone deficiency in zone III, complete radiolucency, polyethylene wear, and component migration.

Figure 90-2 A lateral radiograph should be evaluated for appropriate anteversion of the acetabular component. In this case, the acetabular component has migrated into excessive anteversion.

Figure 90-3 A three-dimensional reconstruction from a computed tomography scan further illustrates the extent of acetabular bone loss.
The condition of the acetabulum should be graded using a radiographic classification system. The Paprosky classification is outlined in Chapter 89. The degree and severity of bone loss will determine whether three-point fixation can be attained, which is a requisite for utilization of a cementless hemispherical acetabular component. A review of the previous operative report should reveal the size of the component present and will assist the surgeon in determining the approximate size of the revision acetabular component. This information will be useful in obtaining appropriately sized components, corresponding polyethylene liners, and femoral head options. Furthermore, the need for any special equipment specific to removal of a particular implant can be determined. A treatment plan for the osteolysis should be outlined preoperatively, and appropriate bone graft material should be made available.
Description of Technique
When the decision is made between the surgeon and the patient to proceed with revision arthroplasty, appropriate medical clearance should be obtained. The patient is assessed by anesthesia staff upon arrival on the day of surgery. After successful induction of anesthesia, the patient is evaluated in the supine position to assess leg length. The patient then is placed in a lateral decubitus position with the operative extremity facing the operative field. The extremity is prepped and draped in standard fashion. Previous surgical incisions are outlined. The hip is approached by utilizing as much of the previous skin incision as possible. The actual approach to the hip will vary depending on the surgeon’s preference. The most common approaches utilized are the posterior lateral and direct lateral (anterior lateral). In cases of difficult exposure, a trochanteric slide osteotomy or an extended trochanteric osteotomy may be required.70 The senior author’s preference is the direct lateral approach.71 Upon completion of the skin incision, the fascia is incised along the line of the incision, identifying the lateral aspect of the femur. Commencing 3 to 4 cm distal to the vastus tubercle, the vastus lateralis is split along the lateral aspect of the femur (Fig. 90-4). This dissection is carried proximally in continuity with the gluteus medius and minimus, elevating approximately the anterior one third of the abductors. The femoral neck of the femoral component is identified, and the capsule is incised in the direction of the femoral neck, extending superiorly to the rim of the acetabulum. Dislocation occurs with the flexion in external rotation–adduction maneuver (Fig. 90-5). Exposure is facilitated by releasing the iliopsoas tendon from the lesser trochanter, if required. If the femoral component is modular, the head/neck unit can be removed (Fig. 90-6). If the femoral component is to be removed, this procedure should be performed at this time to facilitate exposure of the acetabulum. The acetabulum is exposed by placing an anterior retractor approximately 1 cm above the pubis. A posterior sharp, long Hohmann retractor is now placed into the ischium to displace the femur posteriorly. Finally, a spike is driven in at the 12 o’clock position approximately 1 cm above the acetabular component. Circumferential exposure of the acetabulum is required, and all scar tissue should be excised.
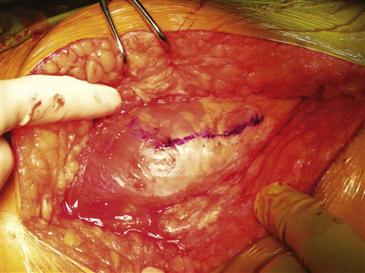
Figure 90-4 Using a direct lateral approach, the vastus lateralis is split along the lateral aspect of the femur, commencing 3 to 4 cm distal to the vastus tubercle, as shown here.

Figure 90-5 Dislocation occurs with the flexion in external rotation–adduction maneuver performed by the assistant.
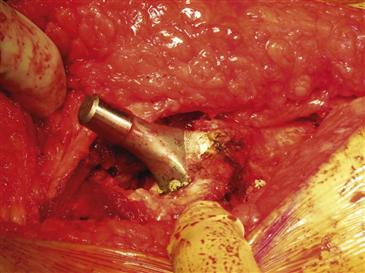
Figure 90-6 The modular head/neck unit of the femoral component is removed to facilitate exposure of the acetabulum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







