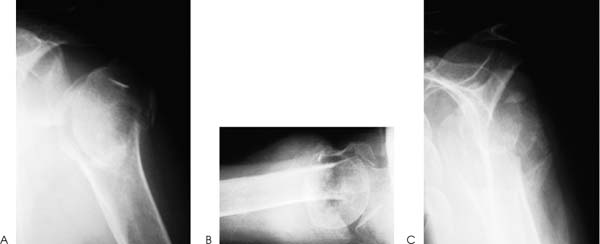
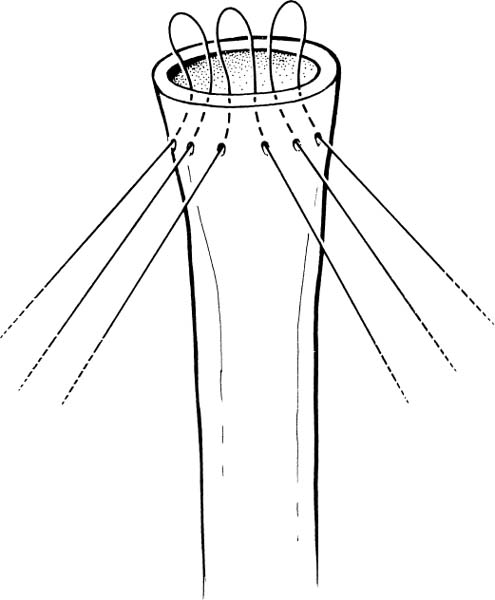
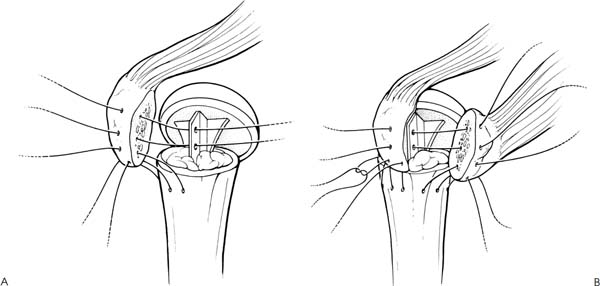
Case 4 A 71-year-old woman presents several hours after a fall onto the affected shoulder. She reports pain and swelling along with crepitation through a limited range of motion. She denies any numbness in her upper extremity or any other injury. On physical examination range of motion is limited by pain. Crepitus is present through this limited range. Moderate swelling about the shoulder is present. Axillary nerve sensation is intact. Radial and ulnar pulses are 2+ distally. No other abnormality is identified. Figure 4–1. Anteroposterior (AP) (A), axillary (B), and scapular Y (C) radiographs demonstrate the fracture pattern. 1. Rotator cuff tear 2. Proximal humerus fracture 3. Fracture dislocation of the proximal humerus 4. Shoulder dislocation An anteroposterior (AP), axillary, and scapular Y view of the shoulder were obtained (Fig. 4–1). Four-Part Fracture. A diagnosis of fracture is suspected based on the patient’s limited range of motion, swelling, and crepitus. Radiographs confirm that a proxi mal humerus fracture is present. Careful evaluation of the radiographs demonstrate significant comminution and displacement of the fracture fragments. Accurate assessment of the degree of comminution, the displacement, and the angulation of the fracture fragments is the key to maximizing functional outcome after such a severe injury. Computed tomography (CT) scanning is very valuable in assessing fracture fragment position and orientation. A CT scan is routinely performed by the authors if any question concerning fracture position exists. This is particularly true when the orientation of the articulating surface of the humeral head is not clearly visualized. This fracture configuration represents a four-part fracture of the proximal humerus. Not uncommonly, the articulating surface of the humeral head is rotated 180 degrees, and no contact between the humeral head articular cartilage and the glenoid exists. Four-part fractures generally occur in elderly, osteopenic patients. This makes fracture fixation difficult to achieve and hemiarthroplasty much more likely. Nonoperative management of four-part fractures will almost certainly result in poor function. Malunion and stiffness due to long immobilization periods will generally occur. Therefore, surgical intervention is performed on all but the most debilitated and functionally limited patients. The treatment of choice for four-part fractures of the proximal humerus is humeral head replacement. Rarely, in young adults with a four-part fracture, the humeral head fragments can be reapproximated using heavy nonabsorbable sutures, with or without screw and/or plate supplementation. Treatment of four-part fractures with internal fixation carries with it a high incidence of avascular necrosis of the articulating segment of the humeral head. Therefore, fracture fixation should be limited only to young adults with good bone stock. The patient is positioned in a semi-sitting position on the operating table. The body is shifted laterally so that the arm can be easily hyperextended over the edge of the table. This is necessary for humeral prosthesis placement. The arm is sterilely prepped and draped free. A long deltopectoral incision is then made, extending inferiorly and slightly obliquely toward the insertion of the deltoid. The subcutaneous tissues are dissected and the deltopectoral interval is identified. The cephalic vein is retracted laterally with the deltoid to expose the subscapularis tendon. Occasionally, it may be necessary to partially free the insertion of the deltoid from the humeral shaft. After the subdeltoid adhesions have been bluntly released, abduct and externally rotate the arm. A Richardson retractor will allow for visualization of the proximal humerus. The upper portion of the insertion of the pectoralis major tendon into the humerus can be released as necessary to improve exposure. The musculo-cutaneous and axillary nerves are then palpated under the conjoined tendon and in the axilla, respectively. Exposure of the fracture fragments is accomplished by gentle mobilization and removal of clot and fracture fragment debris. The biceps tendon serves as an excellent landmark to identify the interval between the lesser and greater tuberosities. The rotator interval capsule can be incised to the glenoid neck to improve exposure of the fracture fragments and to allow for their mobilization. The lesser and greater tuberosity fragments can then be mobilized. This is done after the placement of traction sutures in the subscapularis tendon and supraspinatus tendons. Occasion ally, the greater tuberosity will be comminuted, and if so, the major fragments can be secured together with heavy, nonabsorbable suture so that the majority of the supraspinatus and infraspinatus tendons can be repaired as a unit. With the tuberosities identified and traction sutures placed, the humeral head can be excised. Following removal, the head fragment, if noncomminuted, can be used as a guide to the selection of an appropriate replacement head. After assessment of the size of the head, this fragment can be used as a source of cancellous graft for subsequent use in and around the reapproximated tuberosities after prosthesis placement. The humeral shaft is then prepared by extending the arm off the side of the table. This will deliver the proximal humeral shaft up and out of the wound. Bone and blood clot can be removed from the shaft, and a small humeral shaft broach can be placed into canal. The broach should be small enough to allow the collar to seat closely on the proximal shaft of the humerus. An appropriately sized trial humeral head is then placed and glenohumeral joint stability and range of motion evaluated. After the proper humeral stem and head sizes have been determined, the appropriate amount of retroversion and proximal prominence of the prosthesis is determined. Normal humeral retroversion is 25 to 30 degrees, and in routine replacements this amount of retroversion is placed into the prosthesis. Another important factor to consider in humeral head replacement for four-part fractures is the relative prominence of the prosthesis itself. Generally, loss of the humeral head results in an abnormally shortened humeral shaft. Simply seating the prosthesis as far distally into the remaining shaft as possible will likely shorten the humerus significantly. This will result in an inferior subluxation of the humeral head prosthesis with poor postoperative function. Therefore, methylmethacrylate is almost always used to help stabilize the humeral head prosthesis and maintain the appropriate height to restore normal humeral length. When the proper prosthesis height and retroversion have been determined, the mobilized tuberosities are reap-proximated around the prosthesis, both to one another and to the humeral shaft. Because of the fracture planes and orientation, it is sometimes necessary to debulk the tuberosities, so that they can be repaired around the body of the prosthesis and still allow for good range of motion. Holes should be drilled in the proximal anteromedial, anterolateral, and direct anterior aspect of the shaft prior to placement of the permanent prosthesis. Heavy nonabsorbable sutures (no. 5) are passed through these holes and are used after prosthesis placement to secure the tuberosity fragments to the shaft and the pros-thesis (Fig. 4–2). Placement of the prosthesis into the proximal humeral canal begins with thorough irrigation of the medullary canal to remove blood clot and other debris. Methylmethacrylate is then injected into the proximal humeral canal and the pros-thesis inserted in the appropriate degree of retroversion. A technical trick to aid in maintaining the appropriate amount of retroversion is to notch the proximal humeral shaft at the time of trial prosthesis placement. This makes retroversion easy to reestablish at the time of permanent humeral shaft prosthesis placement. Again, care is taken to maintain the appropriate height of the prosthesis to reapproximate the normal anatomy of the proximal humerus and humeral head. After cement hardening, the prosthesis is reduced into the glenoid fossa. Cancellous bone graft from the humeral head is packed around the fins of the prosthesis. The tuberosities are then reapproximated to the fins, to each other, and to the humeral shaft using the previously placed sutures through the proximal humeral shaft. Additional sutures placed through the tuberosities, their respective tendons, and the holes in the fins of the prosthesis can also be used (Fig. 4–3). Drill holes may be required to pass sutures through the tuberosities, but often osteopenia makes suture passage relatively easy. If the tuberosities are too osteopenic, the sutures should be passed through the tendons to provide for better fixation. The previously incised rotator interval capsule and any other rotator cuff tears should be repaired with nonabsorbable suture (Fig. 4–4). Figure 4–2. Nonabsorbable sutures can be passed through drill holes in the proximal humeral shaft prior to placement of the humeral component. Figure 4–3. The greater (A) and lesser (B) tuberosities are reapproximated to the prosthesis, to each other, and to the shaft using previously placed sutures through the proximal humerus and additional sutures through both the tuberosities, their respective tendons, and the fins of the prosthesis. • After determination of the correct version of the trial humeral component, a small notch can be made in the humeral shaft, making placement of the permanent prosthesis in its proper position more reliable. • Careful repair of the rotator interval following reapproximation of the tuberosity fragments not only helps to ensure rotator cuff repair, but also decreases the tension on the tuberosities postoperatively. • Judicious release of a portion of the deltoid insertion distally serves not only to improve exposure of the fracture but also can protect the deltoid from injury due to retraction.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree