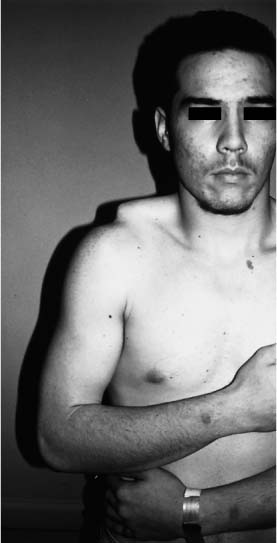
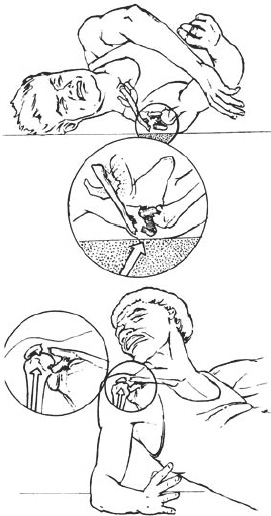
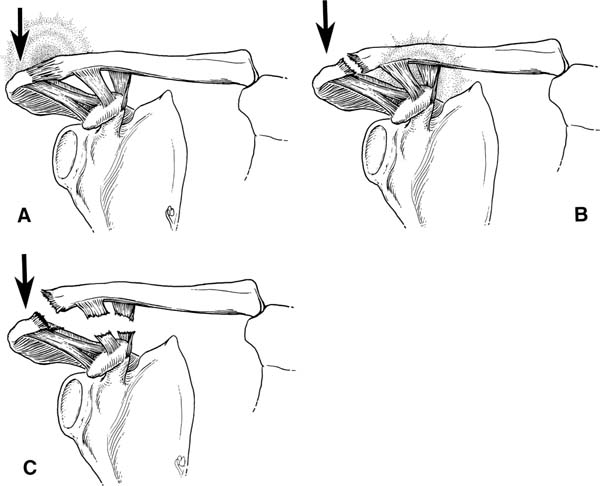
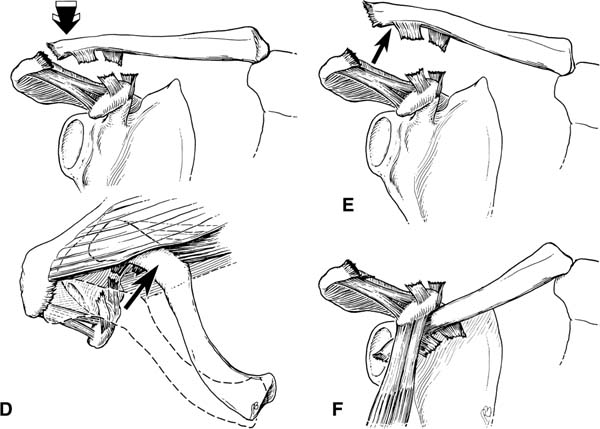
Case 18 A 23-year-old right-hand-dominant heavy laborer falls directly onto the top of his shoulder, presenting with pain and shoulder deformity. The patient demonstrates obvious asymmetry in the area of his acromioclavicular joint (Fig. 18–1). He is tender around this prominence and several superficial abrasions are noted. The patient’s affected upper extremity is neurovascularly intact. Testing reveals full, passive range of motion, but only 20 degrees of active forward flexion. Stability testing of the shoulder is normal. Figure 18–1. A 23-year-old laborer with an obvious asymmetric and tender shoulder after a fall. Figure 18–2. An anteroposterior (AP) radiograph of the affected shoulder. 1. Anterior shoulder dislocation 2. Posterior shoulder dislocation 3. Clavicle fracture 4. Acromioclavicular joint separation 5. Scapula (glenoid/acromion/scapular body) fracture An anteroposterior (AP) view of the shoulder is presented (Fig. 18–2). Acute Disruption of the Acromioclavicular Joint. The obvious clinical deformity, along with the mechanism of injury and the findings on physical exam, point toward an acute acromioclavicular joint separation. These factors, combined with the radiographs, confirm the diagnosis. Occasionally, rotator cuff injury or shoulder dislocation can occur in conjunction with acromioclavicular (AC) disruption. For this reason, a careful and thorough physical exam of the shoulder, including passive range of motion and translation testing, is important. Injury to the AC joint most commonly occurs as a result of a direct force produced by falling on the point of the shoulder with the arm at the side (Fig. 18–3). AC joint injuries occur most commonly in contact sports such as football, hockey, and soccer. A direct blow to the top of the shoulder drives the acromion downward. The clavicle remains in its normal anatomic position; it is the scapula and shoulder girdle that are driven in an inferior direction. This force causes separation of the AC joint with concomitant ligamentous injury. AC joint disruptions constitute a continuum of injury severity. Mild sprains cause limited injury to the AC joint capsule. Moderately severe injuries not only involve damage to the AC joint capsule, but also cause partial tearing of the coracoclavicular ligaments. If the downward force continues, tears of the deltoid and trapezius fascia occur, as well as complete ruptures of the coracoclavicular ligaments. This results in a loss of suspension of the upper extremity by the clavicle, allowing the shoulder girdle to droop downward. Figure 18–3. The most common mechanism of injury to the acromioclavicular (AC) joint is from a direct force to the point of the shoulder (top). Indirect forces to the AC joint may also cause disruption (bottom). (Reprinted from Beim GM, Warner JJP. Clinical and radiographic evaluation of the acromioclavicular joint. Oper Tech Sports Med 1997; 5(2):65–71. With permission.) The most commonly used classification scheme for AC separations was described by Rockwood (1984). The six classifications of AC joint disruption were determined by the degree and direction of displacement of the distal clavicle (Fig. 18–4). Type I AC separations occur secondary to a mild force on the point of the shoulder producing a minor strain to the fibers of the AC ligaments. The AC joint remains stable and the coracoclavicular ligaments remain intact. Type II AC separations result from a moderate force to the point of the shoulder severe enough to cause rupture of the AC ligaments. This allows for subluxation of the AC joint less than one diameter of the distal clavicle. The coracoclavicular ligaments in type II AC separation are only partially disrupted. Type III separations allow for a complete dislocation of the AC joint and result from a complete disruption of both the AC and coracoclavicular ligaments. In type III AC separations, the distal clavicle can be manually reduced into its anatomic location, but it will remain unstable when the pressure is removed. Type IV AC joint separations are characterized by significant posterior displacement of the distal clavicle. The distal clavicle may sometimes be locked within the fibers of the trapezius muscle. Standard radiographs often fail to demonstrate this significant posterior displacement, and careful clinical examination is required. An axillary view can be very helpful in identifying significant posterior displacement of the distal clavicle. Type V AC separations occur from severe forces with complete tearing of the AC and CC ligaments. Extensive soft tissue stripping from the distal clavicle occurs, along with disruption of the deltotrapezial fascia. As a result, the displacement of the distal clavicle is greater than 150% of its cross-sectional diameter. Marked asymmetry and prominence of the distal clavicle is seen. The clavicle can be palpated just deep to the skin and subcutaneous tissues following such an injury. Type VI AC separations are very rare and result from a significant traumatic abduction force to the upper extremity. The distal clavicle is actually dislocated under the coracoid process, posterior to the conjoined tendons. On physical examination, the shoulder has a flattened appearance and the acromion is prominent. Associated trauma such as clavicular fractures, upper rib fractures, and brachial plexis injuries are not uncommon. Figure 18–4. Acromioclavicular joint injuries. (A) Type I: minor AC ligament sprain. Ligaments intact and joint stable. (B) Type II: rupture of the AC ligament and sprain of the coracoclavicular (CC) ligaments. (C) Rupture of both the AC and CC ligaments. Figure 18–4. (D) Type IV: tears of both the AC and CC ligaments with posterior displacement of the distal clavicle. (E) Type V: tears of both the AC and CC ligaments with marked superior displacement of the distal clavicle. Deltotrapezial fascia tears occur as well. (F) Type VI: tears of both the AC and CC ligaments with subcoracoid or subacromial displacement of the distal clavicle. (Reprinted from Beim GM, Warner JJP. Clinical and radiographic evaluation of the acromioclavicular joint. Oper Tech Sports Med 1997; 5(2):65–71. With permission.) The present case demonstrates the marked displacement that occurs in type V AC separations. If treated nonoperatively, this patient not only would have a severe cosmetic deformity, but would likely have poor function and persistent problems associated with the severe soft tissue disruptions, particularly of the deltotrapezial fascia. PEARLS • Shoulder arthroscopy should be given consideration at the time of surgery in patients with severe AC joint separations, or in whom evidence suggests the possibility of intraarticular labral tearing or rotator cuff pathology. • Suture anchor placement into the base of the coracoid process obviates the need for special clamps required for passage of suture around the base of the coracoid process.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree